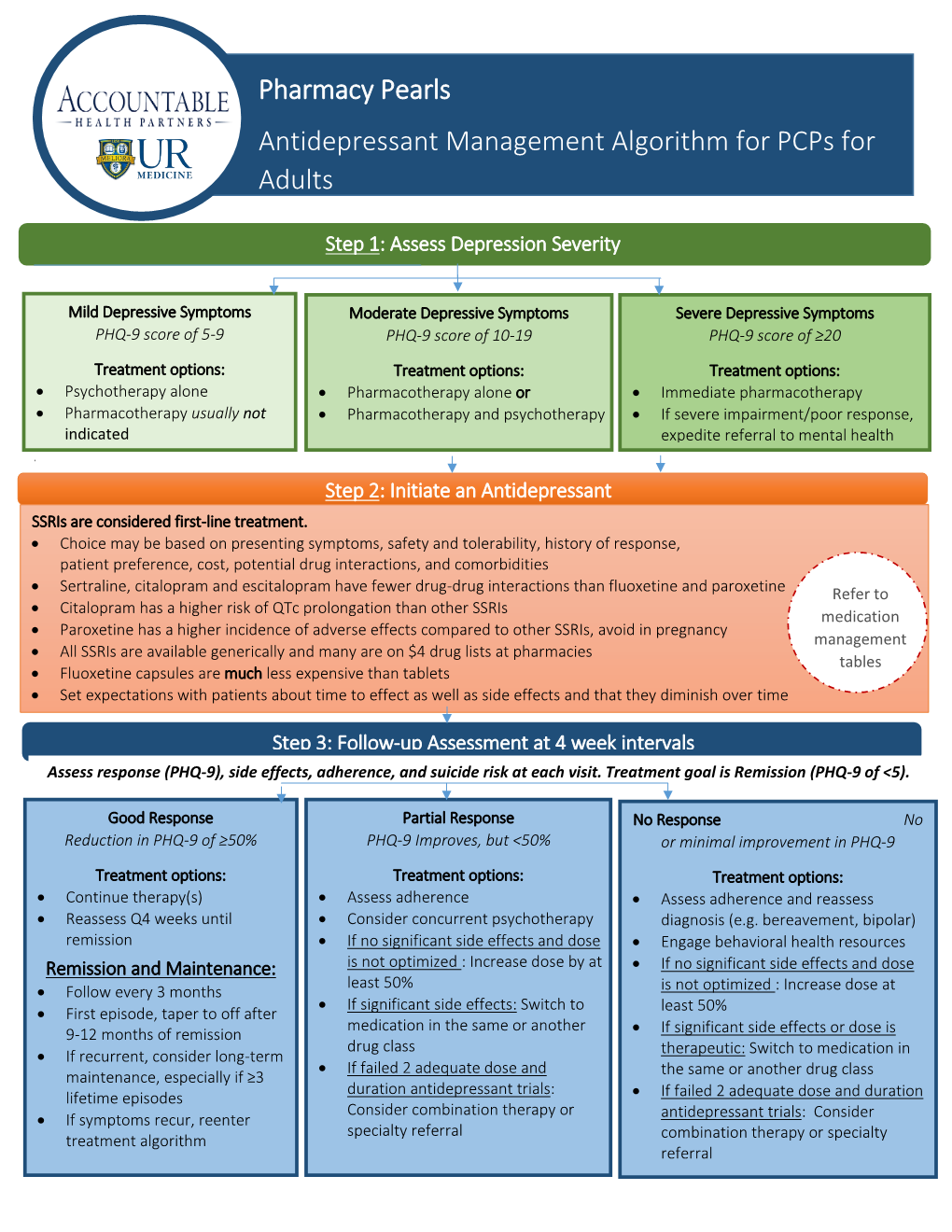
Pharmacy Pearls Antidepressant Management Algorithm for Pcps for Adults
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Efficacy of Treatments for Patients with Obsessive-Compulsive Disorder: a Systematic Review
REVIEW Efficacy of treatments for patients with obsessive-compulsive disorder: A systematic review Yun-Jung Choi, PhD, RN, PMHNP (Lecturer) Keywords Abstract Systematic review; obsessive-compulsive disorder; efficacy of medication. Purpose: This systematic review examines the efficacy of pharmacological therapy for obsessive-compulsive disorder (OCD), addressing two major issues: Correspondence which treatment is most effective in treating the patient’s symptoms and which Yun-Jung Choi, PhD, RN, PMHNP, Red Cross is beneficial for maintaining remission. College of Nursing, 98 Saemoonan-Gil, Data sources: Seven databases were used to acquire articles. The key words Jongno-Gu, Seoul 110-102, Korea; used to search for the relative topics published from 1996 to 2007 were Tel: +82-2-3700-3676; fax: +82-2-3700-3400; ‘‘obsessive-compulsive disorder’’ and ‘‘Yale-Brown obsession-compulsion E-mail: [email protected] scale.’’ Based on the inclusion and exclusion criteria, 25 studies were selected Received: August 2007; from 57 potentially relevant studies. accepted: March 2008 Conclusions: The effects of treatment with clomipramine and selective sero- tonin reuptake inhibitors (SSRIs: fluvoxamine, sertraline, fluoxetine, citalo- doi:10.1111/j.1745-7599.2009.00408.x pram, and escitalopram) proved to be similar, except for the lower adherence rate in case of clomipramine because of its side effects. An adequate drug trial involves administering an effective daily dose for a minimum of 8 weeks. An augmentation strategy proven effective for individuals refractory to monother- apy with SSRI treatment alone is the use of atypical antipsychotics (risperidone, olanzapine, and quetiapine). Implications for practice: Administration of fluvoxamine or sertraline to patients for an adequate duration is recommended as the first-line prescription for OCD, and augmentation therapy with risperidone, olanzapine, or quetiapine is recommended for refractory OCD. -

Formulary and Prescribing Guidelines
Formulary and Prescribing Guidelines SECTION 1: TREATMENT OF DEPRESSION Section 1. Treatment of depression 1.1 Introduction This guidance should be considered as part of a stepped care approach in the management of depressive disorders. Antidepressants are not routinely recommended for persistent sub-threshold depressive symptoms or mild depression but can be considered in these categories where there is a past history of moderate or severe depression, initial presentation of sub-threshold depressive symptoms for at least 2 years, and persistence of either mild or sub-threshold depression after other interventions1 have failed. The most current NICE guidance should be consulted wherever possible to obtain the most up to date information. For individuals with moderate or severe depression, a combination of antidepressant medication and a high intensity psychological intervention (CBT or IPT) is recommended. When depression is accompanied by symptoms of anxiety, usually treat the depression first. If the person has an anxiety disorder and co-morbid depression or depressive symptoms, consider treating the anxiety first. Also consider offering advice on sleep hygiene, by way of establishing regular sleep and wake times; avoiding excess eating, avoiding smoking and drinking alcohol before sleep; and taking regular physical exercise if possible. Detailed information on the treatment of depression in children and adolescents can be found in section 12. Further guidance on prescribing for older adults and for antenatal/postnatal service users can be found in section 11 and section 20, respectively. 1.2 Approved Drugs for the treatment of Depression in Adults For licensing indications, see Annex 1 Drug5 Formulation5 Comments2,3,4 Caps 20mg, 60mg Selective serotonin reuptake inhibitor (SSRI) Fluoxetine Liquid 20mg/5ml 1st line SSRI (based on acquisition cost) Tabs 10mg, 25mg, 50mg Amitriptyline Tricyclic (TCA). -

Antinociceptive Effects of Monoamine Reuptake Inhibitors in Assays of Pain-Stimulated and Pain-Depressed Behaviors
Virginia Commonwealth University VCU Scholars Compass Theses and Dissertations Graduate School 2012 Antinociceptive Effects of Monoamine Reuptake Inhibitors in Assays of Pain-Stimulated and Pain-Depressed Behaviors Marisa Rosenberg Virginia Commonwealth University Follow this and additional works at: https://scholarscompass.vcu.edu/etd Part of the Medical Pharmacology Commons © The Author Downloaded from https://scholarscompass.vcu.edu/etd/2715 This Thesis is brought to you for free and open access by the Graduate School at VCU Scholars Compass. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of VCU Scholars Compass. For more information, please contact [email protected]. ANTINOCICEPTIVE EFFECTS OF MONOAMINE REUPTAKE INHIBITORS IN ASSAYS OF PAIN-STIMULATED AND PAIN-DEPRESSED BEHAVIOR A thesis submitted in partial fulfillment of the requirements for the degree of Master of Science at Virginia Commonwealth University By Marisa B. Rosenberg Bachelor of Science, Temple University, 2008 Advisor: Sidney Stevens Negus, Ph.D. Professor, Department of Pharmacology/Toxicology Virginia Commonwealth University Richmond, VA May, 2012 Acknowledgement First and foremost, I’d like to thank my advisor Dr. Steven Negus, whose unwavering support, guidance and patience throughout my graduate career has helped me become the scientist I am today. His dedication to education, learning and the scientific process has instilled in me a quest for knowledge that I will continue to pursue in life. His thoroughness, attention to detail and understanding of pharmacology has been exemplary to a young person like me just starting out in the field of science. I’d also like to thank all of my committee members (Drs. -

Sertraline and Venlafaxine-Induced Nocturnal Enuresis
Case Report DOI: 10.5455/bcp.20140304091103 Sertraline and Venlafaxine-Induced Nocturnal Enuresis Inci Meltem Atay1, Gulin Ozdamar Unal2 ABS TRACT: Sertraline and venlafaxine-induced nocturnal enuresis Nocturnal enuresis is defined as the involuntary discharge of urine after the age of expected continence that occurs during sleep at night. Although there are a few reports in adults for nocturnal enuresis associated 1Assist. Prof., 2M.D., Suleyman Demirel University, School of Medicine, Department with serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs), the of Psychiatry, Isparta - Turkey mechanism or frequency of this side effect have not been identified yet. We report here a case of nocturnal Corresponding author: Dr. İnci Meltem Atay enuresis associated with both sertraline and venlafaxine in different major depressive episodes in an adult Süleyman Demirel Universitesi, Tıp Fakültesi, Psikiyatri Anabilim Dalı, Isparta - Türkiye patient that resolves after the discontinuation of the medications and continuation with escitalopram. To our E-ma il add ress: knowledge, in literature there have been no reports about nocturnal enuresis caused by those two agents in [email protected] the same patient. This case is discussed in detail for the recurrence of nocturnal enuresis, the importance of Date of submission: detailed assessment of even rare side effects and for their possible mechanisms. February 11, 2014 Date of acceptance: March 04, 2014 Keywords: nocturnal enuresis, venlafaxine, sertraline, depression Declaration of interest: I.M.A, G.O.U.: The authors reported no Klinik Psikofarmakoloji Bulteni - Bulletin of Clinical Psychopharmacology 2015;25(3):287-90 conflict of interest related to this article. INTRODUCTION side effect1-6. -
TAYSIDE PRESCRIBER Issue No
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -
Antidepressants for Functional Gastrointestinal Disorders
Antidepressants for the treatment of Functional Gastrointestinal Disorders Commonly IBS, constipation, diarrhea, functional abdominal pain and esophageal hypersensitivity Document adapted from literature available from the UNC Center for Functional GI & Motility Disorders What are Functional Gastrointestinal Disorders (FGIDs)? There are many different FGIDs (over 20), but among them, IBS is the most common. FGIDs are characterized by abnormal changes in the movement of muscles throughout the intestines (motility abnormality), an increase in the sensations produced by digestive tract activity (visceral hypersensitivity), and brain-gut dysfunction, especially in the brain’s ability to regulate painful signals from the GI tract. People with IBS have an increased awareness and interpretation of these activities as being abnormal. Motility Abnormality Visceral Hypersensitivity Brain-Gut Dysfunction Instead of normal muscular People with IBS, and other When nerve impulses from the gut reach activity (motility) during digestion, FGIDs, may experience an the brain, they may be experienced as people with IBS may experience increased sensitivity in the more severe or less severe based on the painful spasms and cramping. If nerves of the GI tract. This can regulatory activity of the brain-gut axis. motility is too fast it may produce happen after a GI infection or Signals of pain or discomfort travel from diarrhea and if it is too slow it operation which causes injury the intestines back to the brain. The may result in constipation. Motility to the nerves. This produces a brain usually has the ability to “turn abnormalities may be associated lower pain threshold for normal down” the pain by sending signals that with: cramping, belching, digestive sensations, leading to block nerve impulses produced in the GI urgency, and abdominal pain and discomfort. -

Duloxetine for Chronic Pain Relief
Patient Information Leaflet Duloxetine for Chronic Pain Relief Produced By: Chronic Pain Service April 2014 Review due April 2017 1 If you require this leaflet in another language, large print or another format, please contact the Quality Team, telephone 01983 534850, who will advise you. Duloxetine ( Cymbalta ) is a medicine used to relieve chronic pain and treat low mood. It is often helpful for nerve-related pain or pain sensitivity (also called central sensitisation ). It has a different way of relieving pain than standard pain killers and is often prescribed in combination. If used for pain other than diabetes-related neuropathic pain it is formally used outside it’s product license as per individual decision by your pain specialist/doctor. As it affects the central nervous system in complex ways, the effect often takes a while to be felt and requires regular intake . We recommend a trial of at least four weeks to judge the effect. If good, it should be taken on a regular long-term basis; if there is no distinct relief it should be discontinued after the trial period. If you suffer with seizures/epilepsy, glaucoma and poorly controlled high blood pressure, Duloxetine should be used with caution and at a lower dose (up to 60mg per day). The most common side effect is drowsiness/dizziness therefore it is best time to take it in the evening. There are many other possible side effects, but most are uncommon, rare or very rare (please take a look at the product leaflet) We suggest that you avoid driving for at least 2 days after starting or increasing the dose of this medication. -

Milnacipran for Pain in Fibromyalgia in Adults
Milnacipran for pain in fibromyalgia in adults (Review) Cording M, Derry S, Phillips T, Moore RA, Wiffen PJ This is a reprint of a Cochrane review, prepared and maintained by The Cochrane Collaboration and published in The Cochrane Library 2015, Issue 10 http://www.thecochranelibrary.com Milnacipran for pain in fibromyalgia in adults (Review) Copyright © 2015 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 PLAINLANGUAGESUMMARY . 2 SUMMARY OF FINDINGS FOR THE MAIN COMPARISON . ..... 4 BACKGROUND .................................... 6 OBJECTIVES ..................................... 7 METHODS ...................................... 7 RESULTS....................................... 9 Figure1. ..................................... 10 Figure2. ..................................... 12 Figure3. ..................................... 13 Figure4. ..................................... 14 Figure5. ..................................... 18 DISCUSSION ..................................... 21 AUTHORS’CONCLUSIONS . 22 ACKNOWLEDGEMENTS . 23 REFERENCES ..................................... 23 CHARACTERISTICSOFSTUDIES . 27 DATAANDANALYSES. 38 Analysis 1.1. Comparison 1 Milnacipran 100 mg/day versus placebo, Outcome 1 At least 30% pain relief. 39 Analysis 1.2. Comparison 1 Milnacipran 100 mg/day versus placebo, Outcome 2 PGIC ’much improved’ or ’very much improved’.................................... 40 Analysis 1.3. Comparison -

Adverse Effects of First-Line Pharmacologic Treatments of Major Depression in Older Adults
Draft Comparative Effectiveness Review Number xx Adverse Effects of First-line Pharmacologic Treatments of Major Depression in Older Adults Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov This information is distributed solely for the purposes of predissemination peer review. It has not been formally disseminated by the Agency for Healthcare Research and Quality. The findings are subject to change based on the literature identified in the interim and peer-review/public comments and should not be referenced as definitive. It does not represent and should not be construed to represent an Agency for Healthcare Research and Quality or Department of Health and Human Services (AHRQ) determination or policy. Contract No. 290-2015-00012I Prepared by: Will be included in the final report Investigators: Will be included in the final report AHRQ Publication No. xx-EHCxxx <Month, Year> ii Purpose of the Review To assess adverse events of first-line antidepressants in the treatment of major depressive disorder in adults 65 years or older. Key Messages • Acute treatment (<12 weeks) with o Serotonin norepinephrine reuptake inhibitors (SNRIs) (duloxetine, venlafaxine), but not selective serotonin reuptake inhibitors (SSRIs) (escitalopram, fluoxetine) led to a greater number of adverse events compared with placebo. o SSRIs (citalopram, escitalopram and fluoxetine) and SNRIs (duloxetine and venlafaxine) led to a greater number of patients withdrawing from studies due to adverse events compared with placebo o Details of the contributing adverse events in RCTs were rarely reported to more clearly characterize what adverse events to expect. -

Geriatric Psychopharmacology: Anti-Depressants Amber Mackey, D.O
Geriatric Psychopharmacology: Anti-depressants Amber Mackey, D.O. University of Reno School of Medicine Department of Psychiatry Chief Resident, PGY-4 Pharmacologic issues in the elderly More likely to experience drug induced adverse events Cardiac effects: Prolonged QTc, arrhythmias, sudden death Peripheral/central anticholinergic effects: constipation, delirium, urinary retention, delirium, and cognitive dysfunction Antihistaminergic effects: sedation Antiadrenergic effects: postural hypotension Other effects: Hyponatremia, bleeding, altered bone metabolism Pharmacokinetic Organ system Change consequence Circulatory system Decreased concentration Increased or decreased of plasma albumin and free concentration of drugs increased α1-acid in plasma glycoprotein Gastrointestinal Table tract 20-1 Decreased intestinal and Decreased rate of drug splanchnic blood flow absorption Kidney Decreased glomerular Decreased renal filtration rate clearance of active metabolites Liver Decreased liver size; Decreased hepatic decreased hepatic blood clearance flow; variable effects on cytochrome P450 isozyme activity Muscle Decreased lean body mass Altered volume of and increased adipose distribution of lipid-soluble tissue drugs, leading to increased elimination half-life Table 20-1, Physiological changes in elderly persons associated with altered pharmacokinetics, American Psychiatric Publishing Textbook of Geriatric Psychiatry, Fifth Edition, Chapter 20: Psychopharmacology. Other issues Illnesses that effect the elderly also play a role in diminishing -

Cymbalta (Duloxetine Hcl) Prior Authorization of Benefits Form
Cymbalta (Duloxetine HCl) Prior Authorization of Benefits Form CONTAINS CONFIDENTIAL PATIENT INFORMATION Complete form in its entirety and fax to: Prior Authorization of Benefits Center at 844-512-9005 for retail pharmacy or 844-512-7027 for medical injectable. 1. Patient information 2. Physician information Patient name: _________________________________ Prescribing physician: _______________________________ Patient ID #: __________________________________ Physician address: _________________________________ Patient DOB: _________________________________ Physician phone #: _________________________________ Date of Rx: ___________________________________ Physician fax #: ____________________________________ Patient phone #: _______________________________ Physician specialty: _________________________________ Patient email address: __________________________ Physician DEA: ____________________________________ Physician NPI #: ___________________________________ Physician email address: ____________________________ 3. Medication 4. Strength 5. Directions 6. Quantity per 30 days Cymbalta (Duloxetine HCl) ______________________ _____________________ Specify: ________________________ 7. Diagnosis: ____________________________________________________________________________________ 8. Approval criteria: (Check all boxes that apply. Note: Any areas not filled out are considered not applicable to your patient and may affect the outcome of this request.) Major depressive disorder (MDD), depressive disorder or dysthymia: □ Yes □ No Patient has -

Acute Inhibitory Effects of Antidepressants on Lacrimal Gland Secretion in the Anesthetized Rat
Physiology and Pharmacology Acute Inhibitory Effects of Antidepressants on Lacrimal Gland Secretion in the Anesthetized Rat Martin Dankis, Ozgu Aydogdu, Gunnar Tobin, and Michael Winder Department of Pharmacology, Institute of Neuroscience and Physiology, the Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden Correspondence: Michael Winder, PURPOSE. Patients that medicate with antidepressants commonly report dryness of eyes. Department of Pharmacology, The cause is often attributed to the anticholinergic properties of the drugs. However, regu- Institute of Neuroscience and lation of tear production includes a substantial reflex-evoked component and is regulated Physiology, the Sahlgrenska via distinct centers in the brain. Further, the anticholinergic component varies greatly Academy, University of Gothenburg, among antidepressants with different mechanisms of action. In the current study it was Medicinaregatan 13 413 90, Gothenburg, Sweden; wondered if acute administration of antidepressants can disturb production of tears by [email protected]. affecting the afferent and/or central pathway. Received: November 9, 2020 METHODS. Tear production was examined in vivo in anesthetized rats in the presence Accepted: May 10, 2021 or absence of the tricyclic antidepressant (TCA) clomipramine or the selective sero- Published: June 7, 2021 tonin reuptake inhibitor (SSRI) escitalopram. The reflex-evoked production of tears was Citation: Dankis M, Aydogdu O, measured by challenging the surface of the eye with menthol (0.1 mM) and choliner- Tobin G, Winder M. Acute inhibitory gic regulation was examined by intravenous injection with the nonselective muscarinic effects of antidepressants on agonist methacholine (1–5 μg/kg). lacrimal gland secretion in the RESULTS. Acute administration of clomipramine significantly attenuated both reflex- anesthetized rat.