BRS Physiology Cases and Problems 2Nd Edition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
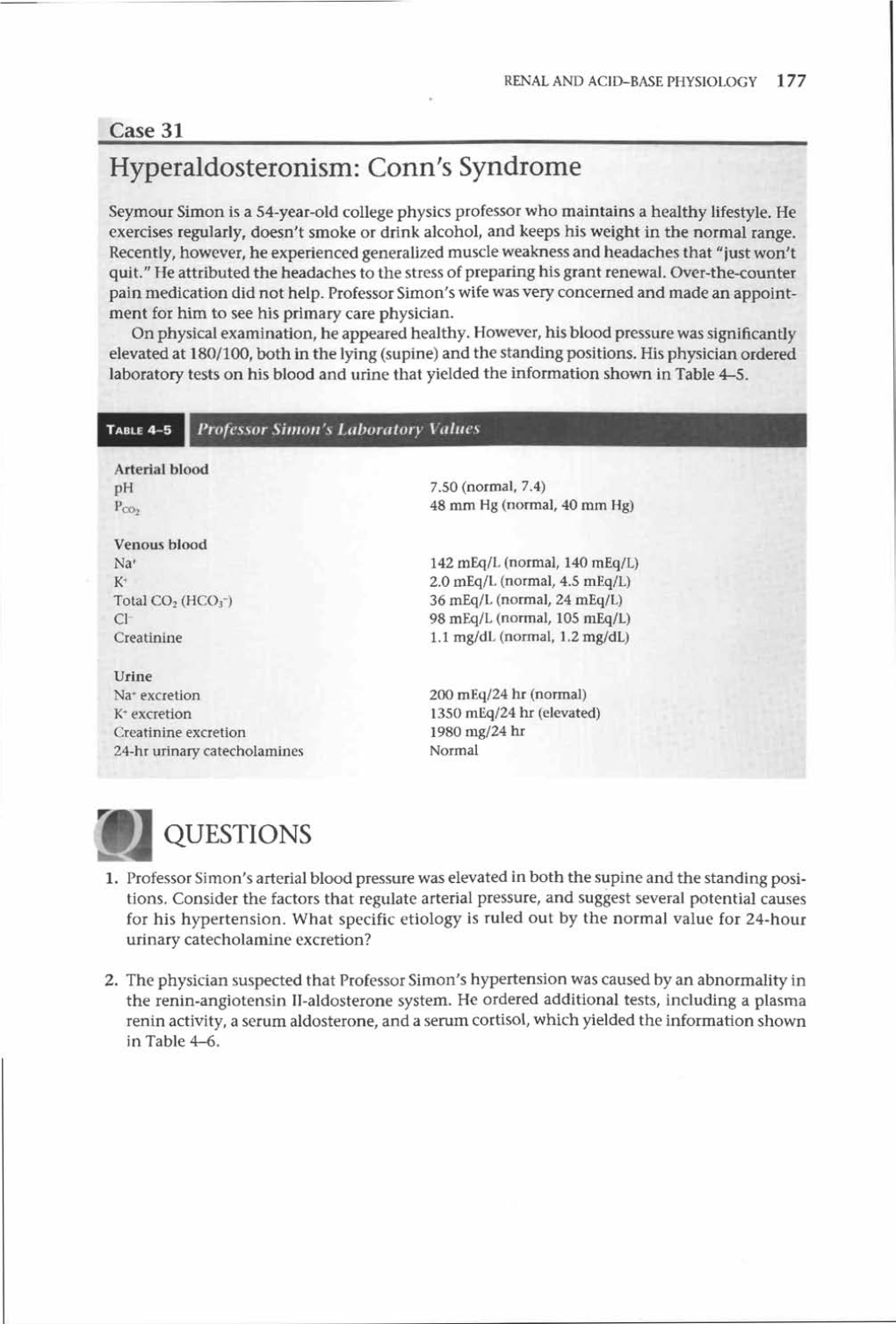
-

Pathophysiology of Acid Base Balance: the Theory Practice Relationship
Intensive and Critical Care Nursing (2008) 24, 28—40 ORIGINAL ARTICLE Pathophysiology of acid base balance: The theory practice relationship Sharon L. Edwards ∗ Buckinghamshire Chilterns University College, Chalfont Campus, Newland Park, Gorelands Lane, Chalfont St. Giles, Buckinghamshire HP8 4AD, United Kingdom Accepted 13 May 2007 KEYWORDS Summary There are many disorders/diseases that lead to changes in acid base Acid base balance; balance. These conditions are not rare or uncommon in clinical practice, but every- Arterial blood gases; day occurrences on the ward or in critical care. Conditions such as asthma, chronic Acidosis; obstructive pulmonary disease (bronchitis or emphasaemia), diabetic ketoacidosis, Alkalosis renal disease or failure, any type of shock (sepsis, anaphylaxsis, neurogenic, cardio- genic, hypovolaemia), stress or anxiety which can lead to hyperventilation, and some drugs (sedatives, opoids) leading to reduced ventilation. In addition, some symptoms of disease can cause vomiting and diarrhoea, which effects acid base balance. It is imperative that critical care nurses are aware of changes that occur in relation to altered physiology, leading to an understanding of the changes in patients’ condition that are observed, and why the administration of some immediate therapies such as oxygen is imperative. © 2007 Elsevier Ltd. All rights reserved. Introduction the essential concepts of acid base physiology is necessary so that quick and correct diagnosis can The implications for practice with regards to be determined and appropriate treatment imple- acid base physiology are separated into respi- mented. ratory acidosis and alkalosis, metabolic acidosis The homeostatic imbalances of acid base are and alkalosis, observed in patients with differing examined as the body attempts to maintain pH bal- aetiologies. -

Chapter 26: Fluid, Electrolyte, and Acid-Base Balance
Chapter 26: Fluid, Electrolyte, and Acid-Base Balance Chapter 26 is unusual because it doesn’t introduce much new material, but it reviews and integrates information from earlier chapters to cover 3 types of regulation: regulation of fluid volume, regulation of electrolyte (=ion) concentrations, and regulation of pH. • Outline of slides: • 1. Regulating fluid levels (blood/ECF) • Compartments of the body • Regulation of fluid intake and excretion • 2. Regulating ion concentrations (blood/ECF) • 3. Regulating pH (blood/ECF) • Chemical buffers • Physiological regulation • Respiratory • Renal 1 3 subsections to this chapter – we will cover the middle one only briefly. 1 Ch. 26: Test Question Templates • Q1. Given relevant plasma data, classify a patient’s possible acid-base disorder as a metabolic or respiratory acidosis or alkalosis that is or is not fully compensated. Or, if given such a disorder, give expected plasma pH and CO2 level (high, normal, or low). • Example A: Plasma pH is 7.32, CO2 levels in blood are low. What is this? • Example B: A patient’s plasma has a pH of 7.5. Explain how you could make an additional measurement to determine whether the cause of this unusual pH is metabolic or respiratory. • Example C: A patient’s plasma CO2 levels are very low, yet plasma pH is normal. How can this be? 2 Q1. Example A: (slight) metabolic acidosis. Example B: Measure the CO2 level in the plasma. If the high plasma pH is due to a respiratory problem, the CO2 concentration will be low. If the high pH is NOT due to a respiratory problem, the CO2 will not be low, and may be high if the person is undergoing respiratory compensation for a metabolic alkalosis. -

The Electro-Physiology-Feeedback Measures of Interstitial Fluids
INTERNATIONAL MEDICAL UNIVERSITY The elecTro-Physiology-Feeedback Measures oF inTersTiTial Fluids BY PROFESSOR OF MEDICINE DESIRÉ DUBOUNET IMUNE PRESS 2008 Electro-Physiology -FeedBack Measures of Interstitial Fluids edited by Professor Emeritus Desire’ Dubounet, IMUNE ISBN 978-615-5169-03-8 1 CHAPTER 1 THE ELECTRO-PHYSIOLOGY-FEEDBACK MEASURES OF INTERSTITIAL FLUIDS The interstitial liquid constitutes the true interior volume that bathe the organs of the human body. It is by its presence that all the exchanges between plasma and the cells are performed. With the vascular, lymphatic and nervous systems, it seems to be the fourth communication way of information's between all the cells. No direct methods for sampling interstitial fluid are currently available. The composition of interstitial fluid, which constitutes the environment of the cells and is regulated by the electrical process of electrochemistry. This has previously been sampled by the suction blister or liquid paraffin techniques or by implantation of a perforated capsule or wick. The results have varied, depending on the sampling technique and animal species investigated. In one study, the ion distribution between vascular and interstitial compartments agreed with the Donnan equilibrium; in others, the concentrations of sodium and potassium were higher in interstitial fluid than in plasma. The concentration of protein in interstitial fluid is lower than in plasma, and the free ion activities theoretically differ from those of plasma because of the Donnan effect. In spite of these differences, and for practical reasons only, plasma is used clinically to monitor fluid and electrolytes. The relation between plasma and interstitial fluid is important in treating patients with abnormal plasma volume or homeostasis. -

New Jersey Chapter American College of Physicians Resident
New Jersey Chapter American College of Physicians Resident Abstract Competition 2018 Submissions Category Name Additional Authors Program Abstract Title Abstract Clinical Vignette Ankit Bansal Ankit Bansal MD, Robert Atlanticare Rare Case of A 62‐year‐old male IV drug abuser with hepatitis C and diabetes presented to the emergency Lyman MS IV, Saraswati Regional Necrotizing department with progressively worsening right forearm pain and swelling for two days after injecting Racherla MD Medical Myositis leading to heroin. Vitals included temperature 98.8°F and heart rate 107 bmp. Physical examination showed Center Thoracic and erythematous skin with surrounding edema and abscess formation of the right biceps extending into (Dominik Abdominal the axilla, and tenderness to palpation of the right upper extremity (RUE). Labs were white blood cell Zampino) Compartment count 16.1 x103/uL with bands 26%, hemoglobin 12.4 g/dL, platelets 89 x103/uL and blood lactate 2.98 Syndrome mmol/L. Patient was admitted to telemetry for sepsis secondary to right arm cellulitis and abscess. Bedside incision and drainage was performed. Blood and wound cultures were drawn and patient was started on Vancomycin and Levofloxacin. On the third day of admission, patient became febrile, obtunded and had signs of systemic toxicity. Labs showed a worsening leukocytosis and lactic acidosis. CT RUE was consistent with complex fluid collection and with extensive gas tracking encircling the entire length of the right biceps brachii muscle. Surgical debridement was performed twice over the next few days. Blood cultures grew corynbacterium and coagulase negative staphylococcus; wound culture grew coagulase negative staphylococcus. Levofloxacin was switched to Aztreonam. -

Acid-Base Disorders Made So Easy Even a Caveman Can Do It
ACID-BASE DISORDERS MADE SO EASY EVEN A CAVEMAN CAN DO IT Lorraine R Franzi, MS/HSM, RD, LDN, CNSD Nutrition Support Specialist University of Pittsburgh Medical Center Pittsburgh, PA I. LEARNING OBJECTIVES The clinician after participating in the roundtable will be able to: 1) Indicate whether the pH level indicates acidosis or alkalosis. 2) State whether the cause of the pH imbalance is respiratory or metabolic. 3) Identify if there is any compensation for the acid-base imbalance. II. INTRODUCTION Acid-Base balance is an intricate concept which requires an intimate and detailed knowledge of the body’s metabolic pathways used to eliminate the H+ ion. Clinicians may find it daunting to understand when first introduced to the subject. This roundtable session will demonstrate how to analyze blood gas levels in a very elementary manner so as to diagnose any acid-base disorder in a matter of minutes. The body is in a constant state of flux delicately stabilizing the pH so as to maintain its normalcy. In order to prevent untoward effects of alkalosis or acidosis the body has three major buffering systems that it uses to adjust the pH. They are: 1) Plasma protein (Prot-) 2) Plasma hemoglobin (Hb-) 3) Bicarbonate (HCO3-) The Bicarbonate-Carbonic acid system is the most dominate buffering system and controls the majority of the hydrogen ion (H+) equilibrium. Maintaining homeostasis when these acid-base shifts occur is vital to survival. Metabolic and respiratory processes work in unison to keep the H+ normal and static. II. ACID-BASE ABNORMALITIES The four principal acid-base imbalances are illustrated in Table 1. -

Arterial Acid–Base Status During Digestion and Following Vascular Infusion of Nahco3 and Hcl in the South American Rattlesnake, Crotalus Durissus
Comparative Biochemistry and Physiology, Part A 142 (2005) 495 – 502 www.elsevier.com/locate/cbpa Arterial acid–base status during digestion and following vascular infusion of NaHCO3 and HCl in the South American rattlesnake, Crotalus durissus Sine K. Arvedsen a,b, Johnnie B. Andersen a,b, Morten Zaar a,b, Denis Andrade b, Augusto S. Abe b, Tobias Wang a,b,* a Department of Zoophysiology, The University of Aarhus, Denmark b Departamento de Zoologia, Instituto de Biocieˆncias, UNESP, Rio Claro, SP, Brazil Received 17 May 2005; received in revised form 30 September 2005; accepted 2 October 2005 Available online 10 November 2005 Abstract Digestion is associated with gastric secretion that leads to an alkalinisation of the blood, termed the ‘‘alkaline tide’’. Numerous studies on À different reptiles and amphibians show that while plasma bicarbonate concentration ([HCO3 ]pl) increases substantially during digestion, arterial pH (pHa) remains virtually unchanged, due to a concurrent rise in arterial PCO2 (PaCO2) caused by a relative hypoventilation. This has led to the suggestion that postprandial amphibians and reptiles regulate pHa rather than PaCO2. Here we characterize blood gases in the South American rattlesnake (Crotalus durissus) during digestion and following systemic infusions of NaHCO3 and HCl in fasting animals to induce a metabolic alkalosis or acidosis in fasting animals. The magnitude of these acid–base disturbances À À 1 were similar in magnitude to that mediated by digestion and exercise. Plasma [HCO3 ] increased from 18.4T1.5 to 23.7T1.0 mmol L during digestion and was accompanied by a respiratory compensation where PaCO2 increased from 13.0T0.7 to 19.1T1.4 mm Hg at 24 h. -

Respiratory Considerations in the Patient with Renal Failure
Respiratory Considerations in the Patient With Renal Failure David J Pierson MD FAARC Introduction Physiologic Connections Between the Lungs and the Kidneys Diseases That Affect Both Lungs and Kidneys Wegener’s Granulomatosis Systemic Lupus Erythematosus Goodpasture’s Syndrome Respiratory Effects of Chronic Renal Failure Pulmonary Edema Fibrinous Pleuritis Pericardial Effusion Tuberculosis and Other Infections Pulmonary Calcification Urinothorax Sleep Apnea Anemia Respiratory Effects of Acute Renal Failure Hemodialysis-Related Hypoxemia How Critical Illness and Mechanical Ventilation Can Damage the Kidneys Summary Lung and kidney function are intimately related in both health and disease. Respiratory changes help to mitigate the systemic effects of renal acid-base disturbances, and the reverse is also true, although renal compensation occurs more slowly than its respiratory counterpart. A large number of diseases affect both the lungs and the kidneys, presenting most often with alveolar hemorrhage and glomerulonephritis. Most of these conditions are uncommon or rare, although three of them— Wegener’s granulomatosis, systemic lupus erythematosus, and Goodpasture’s syndrome—are not infrequently encountered by respiratory care clinicians. Respiratory complications of chronic renal failure include pulmonary edema, fibrinous pleuritis, pulmonary calcification, and a predisposition to tuberculosis. Urinothorax is a rare entity associated with obstructive uropathy. Sleep distur- bances are extremely common in patients with end-stage renal disease, with sleep apnea occurring in 60% or more of such patients. The management of patients with acute renal failure is frequently complicated by pulmonary edema and the effects of both fluid overload and metabolic acidosis. These processes affect the management of mechanical ventilation in such patients and may interfere with weaning. -

Neurologic Complications of Electrolyte Disturbances and Acid–Base Balance
Handbook of Clinical Neurology, Vol. 119 (3rd series) Neurologic Aspects of Systemic Disease Part I Jose Biller and Jose M. Ferro, Editors © 2014 Elsevier B.V. All rights reserved Chapter 23 Neurologic complications of electrolyte disturbances and acid–base balance ALBERTO J. ESPAY* James J. and Joan A. Gardner Center for Parkinson’s Disease and Movement Disorders, Department of Neurology, UC Neuroscience Institute, University of Cincinnati, Cincinnati, OH, USA INTRODUCTION hyperglycemia or mannitol intake, when plasma osmolal- ity is high (hypertonic) due to the presence of either of The complex interplay between respiratory and renal these osmotically active substances (Weisberg, 1989; function is at the center of the electrolytic and acid-based Lippi and Aloe, 2010). True or hypotonic hyponatremia environment in which the central and peripheral nervous is always due to a relative excess of water compared to systems function. Neurological manifestations are sodium, and can occur in the setting of hypovolemia, accompaniments of all electrolytic and acid–base distur- euvolemia, and hypervolemia (Table 23.2), invariably bances once certain thresholds are reached (Riggs, reflecting an abnormal relationship between water and 2002). This chapter reviews the major changes resulting sodium, whereby the former is retained at a rate faster alterations in the plasma concentration of sodium, from than the latter (Milionis et al., 2002). Homeostatic mech- potassium, calcium, magnesium, and phosphorus as well anisms protecting against changes in volume and sodium as from acidemia and alkalemia (Table 23.1). concentration include sympathetic activity, the renin– angiotensin–aldosterone system, which cause resorption HYPONATREMIA of sodium by the kidneys, and the hypothalamic arginine vasopressin, also known as antidiuretic hormone (ADH), History and terminology which prompts resorption of water (Eiskjaer et al., 1991). -

ACS/ASE Medical Student Core Curriculum Acid-Base Balance
ACS/ASE Medical Student Core Curriculum Acid-Base Balance ACID-BASE BALANCE Epidemiology/Pathophysiology Understanding the physiology of acid-base homeostasis is important to the surgeon. The two acid-base buffer systems in the human body are the metabolic system (kidneys) and the respiratory system (lungs). The simultaneous equilibrium reactions that take place to maintain normal acid-base balance are: H" HCO* ↔ H CO ↔ H O l CO g To classify the type of disturbance, a blood gas (preferably arterial) and basic metabolic panel must be obtained. A basic understanding of normal acid-base buffer physiology is required to understand alterations in these labs. The normal pH of human blood is 7.40 (7.35-7.45). This number is tightly regulated by the two buffer systems mentioned above. The lungs contain carbonic anhydrase which is capable of converting carbonic acid to water and CO2. The respiratory response results in an alteration to ventilation which allows acid to be retained or expelled as CO2. Therefore, bradypnea will result in respiratory acidosis while tachypnea will result in respiratory alkalosis. The respiratory buffer system is fast acting, resulting in respiratory compensation within 30 minutes and taking approximately 12 to 24 hours to reach equilibrium. The renal metabolic response results in alterations in bicarbonate excretion. This system is more time consuming and can typically takes at least three to five days to reach equilibrium. Five primary classifications of acid-base imbalance: • Metabolic acidosis • Metabolic alkalosis • Respiratory acidosis • Respiratory alkalosis • Mixed acid-base disturbance It is important to remember that more than one of the above processes can be present in a patient at any given time. -

Special Propedeutics of Internal Diseases
VITEBSK STATE MEDICAL UNIVERSITY DEPARTMENT OF PROPEDEUTICS OF INTERNAL DISEASES SPECIAL PROPEDEUTICS OF INTERNAL DISEASES LECTURE COURSE Compiled by L.M. Nemtsov, MD (2-е издание) Vitebsk, EI «VSMU» 2016 УДК 616.1/.4-07(07) ББК 54.1 С 71 Рецензенты: директор Белорусского государственного медицинского колледжа доктор медицинских наук И.И. Бураков; профессор кафедры общей и клинической фармакологии Витебского государственного медицинского университета доктор медицинских наук М.Р. Конорев Немцов Л.М. С 71 Special propedeutics of internal diseases : lecture course (Частная пропедевтика внутренних болезней : курс лекций (на английском языке) / Л.М. Немцов. – 2-е изд. – Витебск: ВГМУ, 2016. – 318 с. ISBN 978-985-466-822-2 Курс лекций «Частная пропедевтика внутренних болезней» составлен в соответствии с типовой учебной программой по пропедевтике внутренних болезней, утвержденной Министерством Здравоохранения Республики Беларусь в 1997 г., регистрационный № 08-14/5906, и рабочей учебной программой по пропедевтике внутренних болезней для студентов лечебно-профилактического факультета, утвержденной ВГМУ 29.08.2003 г. по специальности «Лечебное дело». УДК 616.1/.4-07(07) ББК 54.1 Первый выпуск в 2011 г. Немцов Л.М., 2016 УО «Витебский государственный медицинский университет», 2016 ISBN 978-985-466-822-2 CONTENT pp reface 5 Diseases of respiratory system Clinical, laboratory and instrumental methods of diagnostics 6 Basic clinical syndromes of pulmonary diseases 13 Respiratory insufficiency (failure) 18 Bronchitis 21 Pulmonary emphysema 25 Cor pulmonale -

The ABC's of Acid-Base Balance
JPPT REVIEW ARTICLE The ABC’s of Acid-Base Balance Gordon S. Sacks, PharmD The University of Wisconsin—Madison, Madison, Wisconsin A step-wise systematic approach can be used to determine the etiology and proper management of acid-base disorders. The objectives of this article are to: (1) discuss the physiologic processes in- volved in acid-base disturbances, (2) identify primary and secondary acid-base disturbances based upon arterial blood gas and laboratory measurements, (3) utilize the anion gap for diagnostic pur- poses, and (4) outline a stepwise approach for interpretation and treatment of acid-base disorders. Case studies are used to illustrate the application of the discussed systematic approach. KEYWORDS: acid-base J Pediatr Pharmacol Ther 2004;9:235-42 Although acid-base disorders are frequently terms of H+, but due to confusing terminology it encountered in hospital and ambulatory care set- was proposed to convert H+ terminology to pH.1 tings, they are often considered the most difficult When taking the negative logarithm of the H+ areas to understand in medicine. Misdiagnosis due to common misconceptions of acid-base ho- ABBREVIATIONS: AG, Anion gap; HCO3, Bicarbonate; CNS, meostasis often delays identification of the pri- Central nervous system; ECF, Extracellular fluid; Hgb, Hemoglobin; ICU, Intensive care unit; THAM, Tromethamine mary disorder, causing a disruption in the deliv- ery of appropriate therapy. By understanding the concentration, pH represents a measure of H+ basic principles of acid-base physiology, the inter- activity. Optimal function for tissues and organs pretation of acid-base data, and the mechanisms within the human body depends on maintaining responsible for acid-base perturbations, the clini- blood pH between 7.10 and 7.60. -

Abim Certification Exam: Nephrology
7/12/16 Disclosures • I am site PI for the REPRISE study evaluating efficacy of ABIM CERTIFICATION tolvaptan in autosomal dominant polycystic kidney EXAM: NEPHROLOGY disease (Otsuka pharmaceuticals) JULY 2016 UCSF CME Division of NephroloGy Department of Medicine Meyeon Park, MD MAS As s is tant Pr ofes s or Roadmap for today • Glomerular diseases (30 min) ---------Scheduled 15 min break------- • Common electrolyte abnormalities (30 min) • Acid-base (45 min) • Acute kidney injury (20 min) GLOMERULAR DISEASES • Secondary hypertension (10 min) 1 7/12/16 Case Laboratory studies A 74 yo man is evaluated for a 5-month history of sinusitis • Hemoglobin 11.5 g/dl and intermittent otitis media. He has lost 9 lbs (4.1 kg) • Leukocyte count 10.8x10^9 /L and has occasional joint pains. • Blood urea nitrogen 28 mg/dl Physical exam: Afebrile • Creatinine 1.6 m/dl HEENT: crusting in right nares; opaque right tympanic • Albumin 3.8 g/dl membrane; bilateral maxillary sinus tenderness • C3 100 mg/dl CV: 2/6 systolic murmur • C4 32 mg/dl Lungs: rhonchi • Urinalysis: 18 dysmorphic erythrocytes and 1 erythrocyte Extremities: 2+ edema bilateral lower ext cast/hpf • CXR: nodule in RUL, hazy density in LLL Case Question Case answer review A. Antinuclear antibody – lupus nephritis – wrong age / Which one of the following studies is most appropriate? sex – low complements A. Antinuclear antibody B. Anti-glomerular basement membrane antibody – wrong B. Anti-glomerular basement membrane antibody history; usually younger men; no respiratory C. Myeloperoxidase antineutrophil cytoplasmic antibody involvement D. Proteinase-3 antineutrophil cytoplasmic antibody C. Myeloperoxidase ANCA – can exist in granulomatous E.