Regional Meeting on Heath System Governance and Community Participation in Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Kyankwanzi Survey Report 2017
GROUND SURVEY FOR MEDIUM - LARGE MAMMALS IN KYANKWANZI CONCESSION AREA Report by F. E. Kisame, F. Wanyama, G. Basuta, I. Bwire and A. Rwetsiba, ECOLOGICAL MONITORING AND RESEARCH UNIT UGANDA WILDLIFE AUTHORITY 2018 1 | P a g e Contents Summary.........................................................................................................................4 1.0. INTRODUCTION ..................................................................................................5 1.1. Survey Objectives.....................................................................................................6 2.0. DESCRIPTION OF THE SURVEY AREA ..........................................................6 2.2. Location and Size .....................................................................................................7 2.2. Climate.....................................................................................................................7 2.3 Relief and Vegetation ................................................................................................8 3.0. METHOD AND MATERIALS..............................................................................9 Plate 1. Team leader and GPS person recording observations in the field.........................9 3.1. Survey design .........................................................................................................10 4.0. RESULTS .............................................................................................................10 4.1. Fauna......................................................................................................................10 -
Action for Rural Women's Empowerment
ACTION FOR RURAL WOMEN’S EMPOWERMENT Action For Rural ARUWE Women’s Empowerment Empowering Communities through women and Children (ARUWE) UGANDA ANNUAL REPORT 2014 - 2015 ANNUAL REPORT 1 ARUWE EMPOWERS THE RURAL COMMUNITIES THROUGH WOMEN AND CHILDREN 2015 Action For Rural ARUWE Women’s Empowerment Empowering Communities through women and Children ARUWE EMPOWERS THE RURAL COMMUNITIES THROUGH WOMEN AND CHILDREN ARUWE ANNUAL REPORT 2014 / 2015 ANNUAL REPORT 2 2015 Word From The Bod Chairperson________________________________________ 2 The Executive Director___________________________________________________ 3 Introduction_____________________________________________________________ 5 Vision, Mission, Core Programs__________________________________________ 5 Geographical Scope_____________________________________________________ 5 Promoting food security, nutrition and income generation________________ 8 Food security____________________________________________________________ 7 Integrating crop growing and livestock rearing___________________________ 9 Promotion of proper nutrition practices__________________________________ 9 Income generation______________________________________________________ 11 Community Fund - MFI__________________________________________________ 11 TABLE OF CONTENTS TABLE Rights awareness and leadership education_____________________________ 13 Water, Sanitation and Hygiene promotion________________________________ 14 Promotion of best practices_____________________________________________ 15 Community participation________________________________________________ -
![Childfund Uganda SITREP [9] [20-05-2020]](https://docslib.b-cdn.net/cover/3664/childfund-uganda-sitrep-9-20-05-2020-463664.webp)
Childfund Uganda SITREP [9] [20-05-2020]
ChildFund Uganda SITREP [9] [20-05-2020] ChildFund International Humanitarian Situation Report Humanitarian Situation Report [9] COVID-19 – [Uganda] [20th May 2020] [Point of Contact – Moses Otai, Country Director, +256 792666620] [Date Range: 14th to 20th May 2020] FOR UPDATES, PLEASE HIGHLIGHT UPDATED SECTIONS IN RED Part 1: The Overall Situation COUNTRY Total Number of COVID-19 Number of Deaths Number of Cases Recuperated Cases Reported 260 0 63 SOURCE: https://www.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 ChildFund-supported areas (Provide only if you have reliable data on this. You can report on a consolidated basis or by program state/region/province/etc. if you have this detail.) Geographical area Total Number of Number of Deaths Number of Cases (country or COVID19 Cases Recuperated state/region/province Reported Country 260 0 63 SOURCE: Uganda Ministry of Health SitRep Any relevant background information about areas affected Of the 260 cases, 53 are Ugandans, 2 are Chinese the majority of whom had recent travel history to Dubai, and other high-risk countries. 24 of those had no travel history but had links with a confirmed cases Only 2 had no link to a confirmed case; 1 case is a boarder trader in Adjumani, and another is an 8 months baby in Iganga whose father had a recent travel history to Kisumu- Kenya. Two cases are Chinese nationals who were part of the group of six re arrested when they 1 | P a g e ChildFund Uganda SITREP [9] [20-05-2020] were attempting to cross to DR Congo and had escaped from the quarantine center. -

WHO UGANDA BULLETIN February 2016 Ehealth MONTHLY BULLETIN
WHO UGANDA BULLETIN February 2016 eHEALTH MONTHLY BULLETIN Welcome to this 1st issue of the eHealth Bulletin, a production 2015 of the WHO Country Office. Disease October November December This monthly bulletin is intended to bridge the gap between the Cholera existing weekly and quarterly bulletins; focus on a one or two disease/event that featured prominently in a given month; pro- Typhoid fever mote data utilization and information sharing. Malaria This issue focuses on cholera, typhoid and malaria during the Source: Health Facility Outpatient Monthly Reports, Month of December 2015. Completeness of monthly reporting DHIS2, MoH for December 2015 was above 90% across all the four regions. Typhoid fever Distribution of Typhoid Fever During the month of December 2015, typhoid cases were reported by nearly all districts. Central region reported the highest number, with Kampala, Wakiso, Mubende and Luweero contributing to the bulk of these numbers. In the north, high numbers were reported by Gulu, Arua and Koti- do. Cholera Outbreaks of cholera were also reported by several districts, across the country. 1 Visit our website www.whouganda.org and follow us on World Health Organization, Uganda @WHOUganda WHO UGANDA eHEALTH BULLETIN February 2016 Typhoid District Cholera Kisoro District 12 Fever Kitgum District 4 169 Abim District 43 Koboko District 26 Adjumani District 5 Kole District Agago District 26 85 Kotido District 347 Alebtong District 1 Kumi District 6 502 Amolatar District 58 Kween District 45 Amudat District 11 Kyankwanzi District -
Sustainable and Resilient Grandmothers Project Report in Mulagi, Kyankwanzi District, Uganda
SUSTAINABLE AND RESILIENT GRANDMOTHERS PROJECT REPORT IN MULAGI, KYANKWANZI DISTRICT, UGANDA End of project report from 1st February 2013 to 31st July 2013 Funded by The Stephen Lewis Foundation Agency Agreement Date: 1stAugust 2012 Agency Agreement Amount: 25,000 CN Compiled and Prepared by: Agnes Mirembe Sylvia Nalubega Action For Rural ARUWE Women’s Empowerment SUSTAINABLETimothy Gasana AND RESILIENT GRANDMOTHERS PROJECT REPORT 1 Peace Rwankiiko INTRODUCTION ince 2010 Stephen Lewis Foundation has partnered with Action for Rural Women’s Empowerment (ARUWE) to support grandmothers and their Orphaned and Vulnerable Children in Mulagi Sub County, Kyankwanzi district. InS 2012-2013 SLF supported the “Sustainable and Resilient Grandmothers Project in Mulagi Sub County, Kyankwanzi district” as a continuation of the last project phase. The main goal of the project was to strengthen the capacities of 150 Grandmothers and 1000 orphaned grandchildren to learn new skills; increase household food security; earn, manage and reinvest income; serve as moral leaders to their families and communities; and keep their orphans safe, healthy, educated and loved. In order to achieve the main project goal, the objectives set included; 1. Increase household food security and income through increased skills, access to agricultural inputs and revolving loan 2. Support health, nutrition and psycho-social enhancing interventions to 150 Grandmothers of orphaned grandchildren in Mulagi Sub County, Kyankwanzi district. Objective One: To increase household food security and income through increased skills, access to agricultural inputs and revolving loan, the project implemented the following activities; Training grandmothers and their caretakers in sustainable agricultural methods To increase household food production, the project conducted trainings in sustainable agriculture methods and practices among the 150 grandmothers and their caretakers 100. -

Uganda Road Fund Annual Report FY 2011-12
ANNUAL REPORT 2011-12 Telephone : 256 41 4707 000 Ministry of Finance, Planning : 256 41 4232 095 & Economic Development Fax : 256 41 4230 163 Plot 2-12, Apollo Kaggwa Road : 256 41 4343 023 P.O. Box 8147 : 256 41 4341 286 Kampala Email : [email protected] Uganda. Website : www.finance.go.ug THE REPUBLIC OF UGANDA In any correspondence on this subject please quote No. ISS 140/255/01 16 Dec 2013 The Clerk to Parliament The Parliament of the Republic of Uganda KAMPALA. SUBMISSION OF UGANDA ROAD FUND ANNUAL REPORT FOR FY 2010/11 In accordance with Section 39 of the Uganda Road Act 2008, this is to submit the Uganda Road Fund Annual performance report for FY 2011/12. The report contains: a) The Audited accounts of the Fund and Auditor General’s report on the accounts of the Fund for FY 2011/12; b) The report on operations of the Fund including achievements and challenges met during the period of reporting. It’s my sincere hope that future reports shall be submitted in time as the organization is now up and running. Maria Kiwanuka MINISTER OF FINANCE, PLANNING AND ECONOMIC DEVELOPMENT cc: The Honourable Minister of Works and Transport cc: The Honourable Minister of Local Government cc: Permanent Secretary/ Secretary to the Treasury cc: Permanent Secretary, Ministry of Works and Transport cc: Permanent Secretary Ministry of Local Government cc: Permanent Secretary Office of the Prime Minister cc: Permanent Secretary Office of the President cc: Chairman Uganda Road Fund Board TABLE OF CONTENTS Abbreviations and Acronyms iii our vision iv -

Dairy Development in Uganda
DAIRY DEVELOPMENT IN UGANDA MinistryThe Republic of Agriculture of Uganda Animal Industry and Fisheries (MAAIF) Food and Agriculture A Review of Uganda’s Dairy Industry Organization of the United Nations Dairy Development Authority (DDA) Author: David Balikowa National Consultant, GOU/FAO Dairy Project, TCP/UGA/3202(D); Senior Business Advisor, TechnoServe/East Africa Dairy Development Project (EADD) March 2011 i TABLE OF CONTENTS LIST OF TABLES .................................................................................................................................. v LIST OF FIGURES ................................................................................................................................ v ACRONYMS AND ABBREVIATIONS .....................................................................................................vi EXECUTIVE SUMMARY ...................................................................................................................... vii CHAPTER 1 ........................................................................................................................................ 1 1. INTRODUCTION ......................................................................................................................... 1 1.1 Geographical Location of Uganda ....................................................................................... 1 1.2 Contribution of Agriculture to the National Economy ......................................................... 1 1.3 Historical Overview of -
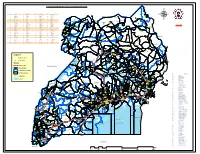
Legend " Wanseko " 159 !
CONSTITUENT MAP FOR UGANDA_ELECTORAL AREAS 2016 CONSTITUENT MAP FOR UGANDA GAZETTED ELECTORAL AREAS FOR 2016 GENERAL ELECTIONS CODE CONSTITUENCY CODE CONSTITUENCY CODE CONSTITUENCY CODE CONSTITUENCY 266 LAMWO CTY 51 TOROMA CTY 101 BULAMOGI CTY 154 ERUTR CTY NORTH 165 KOBOKO MC 52 KABERAMAIDO CTY 102 KIGULU CTY SOUTH 155 DOKOLO SOUTH CTY Pirre 1 BUSIRO CTY EST 53 SERERE CTY 103 KIGULU CTY NORTH 156 DOKOLO NORTH CTY !. Agoro 2 BUSIRO CTY NORTH 54 KASILO CTY 104 IGANGA MC 157 MOROTO CTY !. 58 3 BUSIRO CTY SOUTH 55 KACHUMBALU CTY 105 BUGWERI CTY 158 AJURI CTY SOUTH SUDAN Morungole 4 KYADDONDO CTY EST 56 BUKEDEA CTY 106 BUNYA CTY EST 159 KOLE SOUTH CTY Metuli Lotuturu !. !. Kimion 5 KYADDONDO CTY NORTH 57 DODOTH WEST CTY 107 BUNYA CTY SOUTH 160 KOLE NORTH CTY !. "57 !. 6 KIIRA MC 58 DODOTH EST CTY 108 BUNYA CTY WEST 161 OYAM CTY SOUTH Apok !. 7 EBB MC 59 TEPETH CTY 109 BUNGOKHO CTY SOUTH 162 OYAM CTY NORTH 8 MUKONO CTY SOUTH 60 MOROTO MC 110 BUNGOKHO CTY NORTH 163 KOBOKO MC 173 " 9 MUKONO CTY NORTH 61 MATHENUKO CTY 111 MBALE MC 164 VURA CTY 180 Madi Opei Loitanit Midigo Kaabong 10 NAKIFUMA CTY 62 PIAN CTY 112 KABALE MC 165 UPPER MADI CTY NIMULE Lokung Paloga !. !. µ !. "!. 11 BUIKWE CTY WEST 63 CHEKWIL CTY 113 MITYANA CTY SOUTH 166 TEREGO EST CTY Dufile "!. !. LAMWO !. KAABONG 177 YUMBE Nimule " Akilok 12 BUIKWE CTY SOUTH 64 BAMBA CTY 114 MITYANA CTY NORTH 168 ARUA MC Rumogi MOYO !. !. Oraba Ludara !. " Karenga 13 BUIKWE CTY NORTH 65 BUGHENDERA CTY 115 BUSUJJU 169 LOWER MADI CTY !. -

Kiboga-Kyankwanzi R4d Platform Formation Report
Humidtropics Kiboga/Kyankwanzi platform Report KIBOGA/KYANKWANZI R4D PLATFORM FORMATION REPORT By Anna Sole Amat Kampala, Uganda 6th, February, 2014 Humidtropics, a CGIAR Research Program led by IITA, seeks to transform the lives of the rural poor in tropical America, Asia and Africa. Research organizations involved in core partnership with Humidtropics are AVRDC, Bioversity International, CIAT, CIP, FARA, icipe, ICRAF, ILRI, IITA, IWMI and WUR. humidtropics.cgiar.org Published by Humidtropics February, 2014. This document is licensed for use under a Creative http://humidtropics.cgiar.org Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License Content 0. ACRONYMS .................................................................................................................................................................... ii 1. HUMIDTROPICS SUMMARY ..................................................................................................................................... 4 2. GROUP WORK .............................................................................................................................................................. 4 3. PRIORITIZATION OF ENTRY POINTS .................................................................................................................... 12 4. SELECTION OF R4D PLATFORM COMMITTEE ................................................................................................... 13 5. AGENDA ..................................................................................................................................................................... -

Forests, Livelihoods and Poverty Alleviation: the Case of Uganda Forests, Livelihoods and Poverty Alleviation: the Case of Uganda
Forests, livelihoods and poverty alleviation: the case of Uganda Forests, livelihoods and poverty alleviation: the case of Uganda G. Shepherd and C. Kazoora with D. Mueller Food and Agriculture Organization of the United Nations Rome, 2013 The Forestry Policy and InstitutionsWorking Papers report on issues in the work programme of Fao. These working papers do not reflect any official position of FAO. Please refer to the FAO Web site (www.fao.org/forestry) for official information. The purpose of these papers is to provide early information on ongoing activities and programmes, to facilitate dialogue and to stimulate discussion. The Forest Economics, Policy and Products Division works in the broad areas of strenghthening national institutional capacities, including research, education and extension; forest policies and governance; support to national forest programmes; forests, poverty alleviation and food security; participatory forestry and sustainable livelihoods. For further information, please contact: Fred Kafeero Forestry Officer Forest Economics, Policy and Products Division Forestry Department, FAO Viale Delle terme di Caracalla 00153 Rome, Italy Email: [email protected] Website: www.fao.org/forestry Comments and feedback are welcome. For quotation: FAO.2013. Forests, Livelihoods and Poverty alleviation: the case of Uganda, by, G. Shepherd, C. Kazoora and D. Mueller. Forestry Policy and Institutions Working Paper No. 32. Rome. Cover photo: Ankole Cattle of Uganda The designations employed and the presentation of material in this information product do not imply the expression af any opinion whatsoever on the part of the Food and Agriculture Organization of the United Nations concerning the legal or development status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -

Characterisation of the Livestock Production System and Potential for Enhancing Productivity Through Improved Feeding in Kiboga
Characterisation of the livestock production system and potential for enhancing productivity through improved feeding in Kiboga West DFBA, Kyankwanzi district, Uganda By: Jane Kugonza, Ronald Wabwire, Pius Lutakome, Ben Lukuyu and Josephine Kirui East African Dairy Development Project (EADD) The Feed Assessment Tool (FEAST) is a systematic method to assess local feed resource availability and use. It helps in the design of intervention strategies aiming to optimize feed utilization and animal production. More information and the manual can be obtained at www.ilri.org/feast FEAST is a tool in constant development and improvement. Feedback is welcome and should be directed [email protected]. The International Livestock Research Institute (ILRI) is not responsible for the quality and validity of results obtained using the FEAST methodology. The Feed Assessment Tool (FEAST) was used to characterize the livestock production system and in particular feed‐related aspects in Kiboga West dairy farmers association (DFBA) of Kyankwanzi, Kyankwanzi district, Uganda. The assessment was carried out through structured group discussions and completion of short questionnaires by key farmers’ representatives1. The following are the findings of the assessment and conclusions for further action. Farming system Kyankwanzi was formerly in Kiboga district but obtained district status in 2004 and is located in the extreme part of Buganda region. The travel distance by road is approximately 220 kilometres from the capital city of Uganda, Kampala. Households in this area are composed of approximately 14 (range 6-20) members and utilise on average 15 acres of pastoral land. Table 1 shows farmers perceptions about average land sizes for different categories of farmers. -
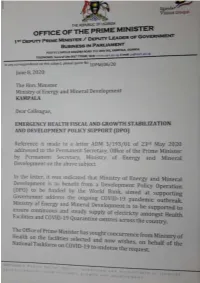
Emergency Health Fiscal and Growth Stabilization and Development
LIST OF COVID-19 QUARANTINE CENTRES IN WATER AND POWER UTILITIES OPERATION AREAS WATER S/N QUARANTINE CENTRE LOCATION POWER UTILITY UTILITY 1 MASAFU GENERAL HOSPITAL BUSIA UWS-E UMEME LTD 2 BUSWALE SECONDARY SCHOOL NAMAYINGO UWS-E UMEME LTD 3 KATAKWI ISOLATION CENTRE KATAKWI UWS-E UMEME LTD 4 BUKWO HC IV BUKWO UWS-E UMEME LTD 5 AMANANG SECONDARY SCHOOL BUKWO UWS-E UMEME LTD 6 BUKIGAI HC III BUDUDA UWS-E UMEME LTD 7 BULUCHEKE SECONDARY SCHOOL BUDUDA UWS-E UMEME LTD 8 KATIKIT P/S-AMUDAT DISTRICT KATIKIT UWS-K UEDCL 9 NAMALU P/S- NAKAPIRIPIRIT DISTRICT NAMALU UWS-K UEDCL 10 ARENGESIEP S.S-NABILATUK DISTRICT ARENGESIEP UWS-K UEDCL 11 ABIM S.S- ABIM DISTRICT ABIM UWS-K UEDCL 12 KARENGA GIRLS P/S-KARENGA DISTRICT KARENGA UWS-K UMEME LTD 13 NAKAPELIMORU P/S- KOTIDO DISTRICT NAKAPELIMORU UWS-K UEDCL KOBULIN VOCATIONAL TRAINING CENTER- 14 NAPAK UWS-K UEDCL NAPAK DISTRICT 15 NADUNGET HCIII -MOROTO DISTRICT NADUNGET UWS-K UEDCL 16 AMOLATAR SS AMOLATAR UWS-N UEDCL 17 OYAM OYAM UWS-N UMEME LTD 18 PADIBE IN LAMWO DISTRICT LAMWO UWS-N UMEME LTD 19 OPIT IN OMORO OMORO UWS-N UMEME LTD 20 PABBO SS IN AMURU AMURU UWS-N UEDCL 21 DOUGLAS VILLA HOSTELS MAKERERE NWSC UMEME LTD 22 OLIMPIA HOSTEL KIKONI NWSC UMEME LTD 23 LUTAYA GEOFREY NAJJANANKUMBI NWSC UMEME LTD 24 SEKYETE SHEM KIKONI NWSC UMEME LTD PLOT 27 BLKS A-F AKII 25 THE EMIN PASHA HOTEL NWSC UMEME LTD BUA RD 26 ARCH APARTMENTS LTD KIWATULE NWSC UMEME LTD 27 ARCH APARTMENTS LTD KIGOWA NTINDA NWSC UMEME LTD 28 MARIUM S SANTA KYEYUNE KIWATULE NWSC UMEME LTD JINJA SCHOOL OF NURSING AND CLIVE ROAD JINJA 29 MIDWIFERY A/C UNDER MIN.OF P.O.BOX 43, JINJA, NWSC UMEME LTD EDUCATION& SPORTS UGANDA BUGONGA ROAD FTI 30 MAAIF(FISHERIES TRAINING INSTITUTE) NWSC UMEME LTD SCHOOL PLOT 4 GOWERS 31 CENTRAL INN LIMITED NWSC UMEME LTD ROAD PLOT 2 GOWERS 32 CENTRAL INN LIMITED NWSC UMEME LTD ROAD PLOT 45/47 CHURCH 33 CENTRAL INN LIMITED NWSC UMEME LTD RD CENTRAL I INSTITUTE OF SURVEY & LAND PLOT B 2-5 STEVEN 34 NWSC 0 MANAGEMENT KABUYE CLOSE 35 SURVEY TRAINING SCHOOL GOWERS PARK NWSC 0 DIVISION B - 36 DR.