FP Project Completion Report, Highlighting Overall Progress and Lessons Learned
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nepal Electricity Authority
NEPAL ELECTRICITY AUTHORITY ENVIRONMENTAL AND SOCIALMANAGEMENT PLAN OF SUPPLY AND INSTALLATION OF DISTRIBUTION PROJECTS (33KV TRANSMISSION LINE) UNDER THE GRID SOLAR AND ENERGY EFFICIECY PROJECT VOLUME II Prepared and Submitted by: Environment and Social Studies Department Kharipati, Bhaktapur Phone No.: 01-6611580, Fax: 01-6611590 Email: [email protected] September, 2018 SIDP Abbreviations and Acronyms ABBREVIATIONS AND ACRONYMS BS : Bikram Sambat (Nepali Era) DADO : District Agriculture Development Office DCC : District Coordination Committee DFO : District Forest Office DoED : Department of Electricity Development ESMF : Environment and Social Management Framework ESMP : Environment and Social Management Plan EPR : Environment Protection Rules, 1997 ESSD : Environment and Social Studies Department GoN : Government of Nepal GSEEP : Grid Tied and Solar Energy Efficiency Project GRC : Grievance Redress Cell GRM : Grievance Redress Mechanism HHs : Households IEE : Initial Environmental Examination MoEWRI : Ministry of Energy, Water Resource and Irrigation MoFE : Ministry of Forest and Environment NEA : Nepal Electricity Authority PAS : Project Affected Settlement PMO : Project Management Office SIDP : Supply and Installation of Distribution Project WB : World Bank Units ha : Hectare km : Kilometer kV : Kilo Volt m2 : Square meter ESMP Report i NEA-ESSD SIDP Table of Contents Table of Contents ABBREVIATIONS AND ACRONYMS ........................................................................................ I 1 INTRODUCTION ............................................................................................................ -

Nepal Earthquake District Profile - Gorkha OSOCC Assessment Cell 09.05.2015
Nepal Earthquake District Profile - Gorkha OSOCC Assessment Cell 09.05.2015 This report is produced by the OSOCC Assessment Cell based on secondary data from multiple sources, including the Government of Nepal, UNDAC, United Nations Agencies, non-governmental organisation and media sources. I. Situation Overview Gorkha, with a population of more than 271,000, is one of the worst-affected districts.1 The epicenter of the earthquake was in Brapok, 15km from Gorkha town. As of 6 May, 412 people have been reported killed and 1,034 injured. In the southern part of the district, food has been provided, but field observations indicate that the food supplied might not be enough for the actual population in the area. Several VDCs in the mountainous areas of Gorkha are yet to be reached by humanitarian assistance. There are no roads in these northern areas, only footpaths. The level of destruction within the district and even within VDCs varies widely, as does the availability of food. A humanitarian hub has been set up at the Chief District Officer’s (CDO) premises in Gorkha town. Reported number of people in need (multiple sources) The figures featured in this map have been collected via multiple sources (district authorities, Red Cross, local NGO, media). Where multiple figures for the same location have been reported the highest one was taken. These figures are indicative and do not represent the overall number of people in need. 1 This is an updated version of the Gorkha District Profile that was published by ACAPS on 1 May 2015. As with other mountain areas of Nepal, Gorkha contains popular locations for foreign trekkers. -

Food Insecurity and Undernutrition in Nepal
SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics Acknowledgements The completion of both this and the earlier feasibility report follows extensive consultation with the National Planning Commission, Central Bureau of Statistics (CBS), World Food Programme (WFP), UNICEF, World Bank, and New ERA, together with members of the Statistics and Evidence for Policy, Planning and Results (SEPPR) working group from the International Development Partners Group (IDPG) and made up of people from Asian Development Bank (ADB), Department for International Development (DFID), United Nations Development Programme (UNDP), UNICEF and United States Agency for International Development (USAID), WFP, and the World Bank. WFP, UNICEF and the World Bank commissioned this research. The statistical analysis has been undertaken by Professor Stephen Haslett, Systemetrics Research Associates and Institute of Fundamental Sciences, Massey University, New Zealand and Associate Prof Geoffrey Jones, Dr. Maris Isidro and Alison Sefton of the Institute of Fundamental Sciences - Statistics, Massey University, New Zealand. We gratefully acknowledge the considerable assistance provided at all stages by the Central Bureau of Statistics. Special thanks to Bikash Bista, Rudra Suwal, Dilli Raj Joshi, Devendra Karanjit, Bed Dhakal, Lok Khatri and Pushpa Raj Paudel. See Appendix E for the full list of people consulted. First published: December 2014 Design and processed by: Print Communication, 4241355 ISBN: 978-9937-3000-976 Suggested citation: Haslett, S., Jones, G., Isidro, M., and Sefton, A. (2014) Small Area Estimation of Food Insecurity and Undernutrition in Nepal, Central Bureau of Statistics, National Planning Commissions Secretariat, World Food Programme, UNICEF and World Bank, Kathmandu, Nepal, December 2014. -
Landslide Inventory, Characterization and Engineering Design for Mitigation Works of Chure Area in Ten Districts
LANDSLIDE INVENTORY, CHARACTERIZATION AND ENGINEERING DESIGN FOR MITIGATION WORKS OF CHURE AREA IN TEN DISTRICTS Submitted to: Submitted by: Government of Nepal Central Department of Environmental President Chure-Tarai Madhesh Science Conservation Development Board Tribhuvan University, Kirtipur Kathmandu September, 2016 © September 2016 President Chure-Tarai Madhesh Conservation Development Board and Central Department of Environmental Science, Tribhuvan University Citation: TU-CDES (2016). Landslide Inventory Characterization and Engineering Design for Mitigation Works of Chure Area in Ten Districts. Central Department of Environmental Science, Tribhuvan University and Government of Nepal, President Chure-Tarai Madhesh Conservation Development Board, Kathmandu. Project Steering Committee Chair Dr. Annapurna Das, Secretary , PCTMCDB/GoN Prof. Dr. Madan Koirala, Professor, TU-CDES Member Prof. Dr. Kedar Rijal, Head of Department, TU-CDES Member Prof. Dr. Rejina Maskey, Project Team Leader, TU-CDES Member Dr. Prem Paudel, Under Secretary, PCTMCDB/GoN Member Dr. Subodh Dhakal, Project Coordinator, TU-CDES Member Mr. Gehendra Keshari Upadhya, Joint Secretary , PCTMCDB/GoN Member Mr. Pashupati Koirala, Under- Secretary, PCTMCDB/GoN Project Team Team Leader Prof. Dr. Rejina Maskey Project Co-ordinator Dr. Subodh Dhakal Geo-Technical Engineer Dr. Ram Chandra Tiwari GIS Expert Mr. Ajay Bhakta Mathema Geologist Mr. Suman Panday Assistant Geologist Mr. Niraj Bal Tamang Assistant GIS Analyst Mr. Padam Bahadur Budha Assistant GIS Analyst Ms. Shanta Banstola Social Surveyor Mr. Kumod Lekhak Field Assistant Mr. Nabin Nepali Review Technical Reviewer: Dr. Ranjan Kumar Dahal English Reviewer: Dr. Dinesh Raj Bhuju ii ACKNOWLEDGEMENTS Hazards like earthquake, landslide, soil erosion and sedimentation all shape the landscape and relief of the Himalaya. Land degradation of the Chure area of Nepal is primarily contributed by different types of landslides and mass wasting phenomena. -
Map of Dolakha District Show Ing Proposed Vdcs for Survey
Annex 3.6 Annex 3.6 Map of Dolakha district showing proposed VDCs for survey Source: NARMA Inception Report A - 53 Annex 3.7 Annex 3.7 Summary of Periodic District Development Plans Outlay Districts Period Vision Objectives Priorities (Rs in 'ooo) Kavrepalanchok 2000/01- Protection of natural Qualitative change in social condition (i) Development of physical 7,021,441 2006/07 resources, health, of people in general and backward class infrastructure; education; (ii) Children education, agriculture (children, women, Dalit, neglected and and women; (iii) Agriculture; (iv) and tourism down trodden) and remote area people Natural heritage; (v) Health services; development in particular; Increase in agricultural (vi) Institutional development and and industrial production; Tourism and development management; (vii) infrastructure development; Proper Tourism; (viii) Industrial management and utilization of natural development; (ix) Development of resources. backward class and region; (x) Sports and culture Sindhuli Mahottari Ramechhap 2000/01 – Sustainable social, Integrated development in (i) Physical infrastructure (road, 2,131,888 2006/07 economic and socio-economic aspects; Overall electricity, communication), sustainable development of district by mobilizing alternative energy, residence and town development (Able, local resources; Development of human development, industry, mining and Prosperous and resources and information system; tourism; (ii) Education, culture and Civilized Capacity enhancement of local bodies sports; (III) Drinking -

Japan International Cooperation Agency (JICA)
Chapter 3 Project Evaluation and Recommendations 3-1 Project Effect It is appropriate to implement the Project under Japan's Grant Aid Assistance, because the Project will have the following effects: (1) Direct Effects 1) Improvement of Educational Environment By replacing deteriorated classrooms, which are danger in structure, with rainwater leakage, and/or insufficient natural lighting and ventilation, with new ones of better quality, the Project will contribute to improving the education environment, which will be effective for improving internal efficiency. Furthermore, provision of toilets and water-supply facilities will greatly encourage the attendance of female teachers and students. Present(※) After Project Completion Usable classrooms in Target Districts 19,177 classrooms 21,707 classrooms Number of Students accommodated in the 709,410 students 835,820 students usable classrooms ※ Including the classrooms to be constructed under BPEP-II by July 2004 2) Improvement of Teacher Training Environment By constructing exclusive facilities for Resource Centres, the Project will contribute to activating teacher training and information-sharing, which will lead to improved quality of education. (2) Indirect Effects 1) Enhancement of Community Participation to Education Community participation in overall primary school management activities will be enhanced through participation in this construction project and by receiving guidance on various educational matters from the government. 91 3-2 Recommendations For the effective implementation of the project, it is recommended that HMG of Nepal take the following actions: 1) Coordination with other donors As and when necessary for the effective implementation of the Project, the DOE should ensure effective coordination with the CIP donors in terms of the CIP components including the allocation of target districts. -
VBST Short List
1 आिेदकको दर्ा ा न륍बर नागररकर्ा न륍बर नाम थायी जि쥍ला गा.वि.स. बािुको नाम ईभेꅍट ID 10002 2632 SUMAN BHATTARAI KATHMANDU KATHMANDU M.N.P. KEDAR PRASAD BHATTARAI 136880 10003 28733 KABIN PRAJAPATI BHAKTAPUR BHAKTAPUR N.P. SITA RAM PRAJAPATI 136882 10008 271060/7240/5583 SUDESH MANANDHAR KATHMANDU KATHMANDU M.N.P. SHREE KRISHNA MANANDHAR 136890 10011 9135 SAMERRR NAKARMI KATHMANDU KATHMANDU M.N.P. BASANTA KUMAR NAKARMI 136943 10014 407/11592 NANI MAYA BASNET DOLAKHA BHIMESWOR N.P. SHREE YAGA BAHADUR BASNET136951 10015 62032/450 USHA ADHIJARI KAVRE PANCHKHAL BHOLA NATH ADHIKARI 136952 10017 411001/71853 MANASH THAPA GULMI TAMGHAS KASHER BAHADUR THAPA 136954 10018 44874 RAJ KUMAR LAMICHHANE PARBAT TILAHAR KRISHNA BAHADUR LAMICHHANE136957 10021 711034/173 KESHAB RAJ BHATTA BAJHANG BANJH JANAK LAL BHATTA 136964 10023 1581 MANDEEP SHRESTHA SIRAHA SIRAHA N.P. KUMAR MAN SHRESTHA 136969 2 आिेदकको दर्ा ा न륍बर नागररकर्ा न륍बर नाम थायी जि쥍ला गा.वि.स. बािुको नाम ईभेꅍट ID 10024 283027/3 SHREE KRISHNA GHARTI LALITPUR GODAWARI DURGA BAHADUR GHARTI 136971 10025 60-01-71-00189 CHANDRA KAMI JUMLA PATARASI JAYA LAL KAMI 136974 10026 151086/205 PRABIN YADAV DHANUSHA MARCHAIJHITAKAIYA JAYA NARAYAN YADAV 136976 10030 1012/81328 SABINA NAGARKOTI KATHMANDU DAANCHHI HARI KRISHNA NAGARKOTI 136984 10032 1039/16713 BIRENDRA PRASAD GUPTABARA KARAIYA SAMBHU SHA KANU 136988 10033 28-01-71-05846 SURESH JOSHI LALITPUR LALITPUR U.M.N.P. RAJU JOSHI 136990 10034 331071/6889 BIJAYA PRASAD YADAV BARA RAUWAHI RAM YAKWAL PRASAD YADAV 136993 10036 071024/932 DIPENDRA BHUJEL DHANKUTA TANKHUWA LOCHAN BAHADUR BHUJEL 136996 10037 28-01-067-01720 SABIN K.C. -

WASH Cluster Nepal 4W - May 12Th 2015
WASH Cluster Nepal 4W - May 12th 2015 Please find following the analysis of the 4W data – May 12th Introduction (Round 2) This is the second round of the 4W analysis. As this is the second round and still early in the emergency response, many agencies are still planning their interventions and caseloads, hence much of the data is understandably incomplete. In the coming week/s we will receive far more comprehensive partner data and will be able to show realistic gaps. In addition, we are receiving better affected population data and there are many ongoing assessments, the results of which will help us to understand both the response data and the affected population data and enable us to deliver a far more profound analysis of the WASH response. Please assist us as we have a lot of information gaps in the data provided so far and hence the maps are not yet providing a true picture of the response. We would like to quickly move to VDC mapping including planned/reached beneficiaries. Since the first round of reporting, agencies have provided substantially more VDC‐level data – as of today, of 740 WASH activities identified, 546 of these (74%) are matched to an identified VDC ‐ this is a big improvement from last week (which had VDC data for 192 of 445 activities, or 43%) The Highlights ・ 47 Organisations – number of organisations that reported in Round 1 and/or Round 2 of the WASH 4W ・ 206 VDCs – where WASH interventions taking place/planned (in 15 districts) 4W – WASH May 12th 2015 Water0B Spread of water activities ‐ targeted Temporary -
![NEPAL: Gorkha - Operational Presence Map [As of 14 July 2015]](https://docslib.b-cdn.net/cover/2101/nepal-gorkha-operational-presence-map-as-of-14-july-2015-1052101.webp)
NEPAL: Gorkha - Operational Presence Map [As of 14 July 2015]
NEPAL: Gorkha - Operational Presence Map [as of 14 July 2015] 60 Samagaun Partners working in Gorkha Chhekampar 1-10 11-15 16-20 21-25 26-35 Lho Bihi Prok Chunchet Partners working in Nepal Sirdibas Health 26 Keroja Shelter and NFI Uhiya 23 Ghyachok Laprak WASH 18 Kharibot Warpak Gumda Kashigaun Protection 13 Lapu HansapurSimjung Muchchok Manbu Kerabari Sairpani Thumo Early Recovery 6 Jaubari Swara Thalajung Aaruaarbad Harmi ShrithankotTar k u k ot Amppipal ArupokhariAruchanaute Education 5 Palungtar Chhoprak Masel Tandrang Khoplang Tap le Gaikhur Dhawa Virkot PhinamAsrang Nutrition 1 Chyangling Borlang Bungkot Prithbinarayan Municipality Namjung DhuwakotDeurali Bakrang GhairungTan gli ch ok Tak lu ng Phujel Manakamana Makaising Darbung Mumlichok Ghyalchok IMPLEMENTING PARTNERS BY CLUSTER Early Recovery Education Health 6 partners 5 partners 26 partners Nb of Nb of Nb of organisations organisations organisations 1 >=5 1 >=5 1 >=5 Nutrition Protection Shelter and NFI 1 partners 13 partners 23 partners Nb of Nb of Nb of organisations organisations organisations 1 >=5 1 >=5 1 >=5 WASH 18 partners Want to find out the latest 3W products and other info on Nepal Earthquake response? visit the Humanitarian Response website at http:www.humanitarianresponse.info/en/op Nb of Note: organisations Implementing partners represent the organization on the ground, erations/nepal in the affected district doing operational work, such as send feedback to 1 >=5 distributing food, tents, water purification kits etc. [email protected] Creation date:23 July 2015 Glide number: EQ-2015-000048-NPL Sources: Cluster reporting The boundaries and names shown and the designations used on this map do not imply official endorsement or acceptance by the United Nations. -
![Uf]/Vf K'gm;J]{If0f Ug'{Kg]{ Nfeu|Fxl Ljj/0F](https://docslib.b-cdn.net/cover/5832/uf-vf-kgm-j-if0f-ug-kg-nfeu-fxl-ljj-0f-1055832.webp)
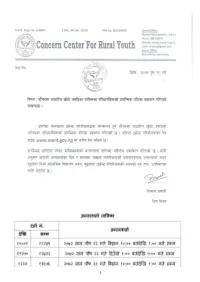
Uf]/Vf K'gm;J]{If0f Ug'{Kg]{ Nfeu|Fxl Ljj/0F
g]kfn ;/sf/ ;+3Lo dfldnf tyf :yfgLo ljsf; dGqfno s]Gb|Lo cfof]hgf sfof{Gjog OsfO{ e"sDkLo cfjf; k'glg{df{0f cfof]hgf Hjfun, nlntk'/ uf]/vf k'gM;j]{If0f ug'{kg]{ nfeu|fxL ljj/0f . S.N G_ID RV/RS Grievant Name District VDC/MUN (P) Ward(P) Tole GP/NP WARD Slip No Remarks 1 281924 RS Nettra Bahadur Thap Gorkha Aanppipal 1 bajredanda Palungtar 3 21350 2 290180 RS Sabitri Devi Bhattrai Gorkha Aanppipal 1 bajredanda Palungtar 3 212331 3 288425 RS Jit Bahadur Rana Magar Gorkha Aanppipal 1 jal jala Palungtar 3 4 290553 RS Dhan Bahadur Rana Gorkha Aanppipal 1 judi thumka Palungtar 3 5 290114 RS Rithe Sarki Gorkha Aanppipal 1 pathivara Palungtar 3 6 288914 RS Tulka Sarki Gorkha Aanppipal 1 pathivara Palungtar 3 7 288959 RS Arjun Baniya Gorkha Aanppipal 1 pathivara Palungtar 3 8 290178 RS Sanak Bahadur Bhattrai Gorkha Aanppipal 1 pathivara Palungtar 3 9 290030 RS Jibarayal Miya Gorkha Aanppipal 2 dumre danda Palungtar 3 10 290560 RS Gurungseni Sunar Gorkha Aanppipal 2 maibal Palungtar 3 215317 11 290034 RS Damar Kumari Thapa Gorkha Aanppipal 2 maibal Palungtar 3 12 288925 RS Amar Bahadur Kuwar Gorkha Aanppipal 2 pachchyan Palungtar 3 13 290556 RS Rajendra Dhakal Gorkha Aanppipal 2 raute pani Palungtar 3 215570 14 286299 RS Sarala Devkota Gorkha Aanppipal 2 raute pani Palungtar 3 423666 15 288462 RS Bijaya Raj Devkota Gorkha Aanppipal 2 raute pani Palungtar 3 16 288920 RS Shree Niwas Devkota Gorkha Aanppipal 2 raute pani Palungtar 3 17 290055 RS Uttam Kumar Shtestha Gorkha Aanppipal 2 raute pani Palungtar 3 18 290047 RS Brendra Devkota Gorkha Aanppipal -

DAMS & DEVELOPMENT: Emerging Trendsinnepal's Hydropower Terrain
Recognising Entitlements and Sharing Benefits: Emerging TrendsinNepal’s Hydropower Terrain Dialogue on DAMS & DEVELOPMENT:NEPAL Copyright: © 2005 IUCN-The World Conservation Union Nepal and Nepal Water Conservation Foundation Published in support of the Dams and Development Strategic Priorities Series for the National Steering Committee on Dams and Development by IUCN Nepal and Nepal Water Conservation Foundation The role of German Technical Cooperation (GTZ) in supporting the Dams and Development Strategic Priorities Series is gratefully acknowledged. The material in this publication may be reproduced in whole or in part and in any form for educational or non-profit uses, without prior written permission from the copyright holder, provided acknowledgement of the source is made. IUCN Nepal would appreciate receiving a copy of any publication which uses this publication as a source. DISCLAIMER No use of this publication may be made for resale or other commercial purposes without prior written permission of IUCN Nepal and NWCF. This Dams and Development Strategic Citation: Dixit, Ajay & Basnet, Shreshna (2005). Recognising Entitle- Priorities Series summaries the find- ments and Sharing Benefits: Emerging Trends in Nepal's Hydropower Terrain ings and serves as a platform for con- IUCN Nepal + 38 pp. tinuing the dialogue on the issues of water resources development and dams Technical Advice: Bhawani P. Kharel and Deependra Joshi in Nepal. This report can assist in the ISBN: 99933-860-9 evolution of the policy process, but it is not the policy document of any of the Printed by: Quality Printers Kathmandu, Nepal organizations involved in the specific priorities series consultative processes. ii Foreword t is five years since the report of the World Commission Priorities. -

(Tor) for SUPPLYING CONSTRUCTION MATERIALS for HSRP, NUWAKOT
Terms of Reference (ToR) FOR SUPPLYING CONSTRUCTION MATERIALS FOR HSRP, NUWAKOT Project Title Health System Recovery Project, Nuwakot Type of project Health Location Bidur-04, Nuwakot Name of the company/firm External company/firm/supplier Deadline of Bid submission 29th August, 2018 Anticipated completion of project 30th September, 2018 1.0 GENERAL INTRODUCTION Good Neighbors International (GNI) Nepal has been working in Nepal since 2002 with the objective of improving lives of the poor people especially children through education, child protection, and income generating activities, health, WASH, and disaster risk reduction. GNI Nepal has been operating its activities in 20 districts. GNI Nepal with support from the Korea International Cooperation Agency (KOICA) has been implementing Health System Recovery Project (HSRP) in two Municipalities and five Rural Municipalities of Nuwakot District since December 2015 with the major objective of improving the health status and psychosocial well-being of community members through post-disaster recovery. In total, 10 former VDCs of Nuwakot (Belkot, Charghare, Duipipal, Ghyangphedi, Likhu, Okharpauwa, Panchakanya, Ratmate, Suryamati and Thaprek) are the working areas of HSRP. One of the major objectives of the project is to improve adolescent sexual and reproductive health (ASRH) status in the project areas. This includes, in addition to other activities, building hygienic environment at 32 basic and secondary public schools. The Project has constructed/is constructing Gender Friendly Toilets (GFT) at 14-targeted public schools. In addition to GFT construction, the Project is installing Safe Drinking Water Management System in 22 schools of project areas. HSRP is planning to provide HDPE pipe and then install Bio- sand filter in 7 additional needful schools and to provide materials for school compound fencing at two schools of project area.