Therapeutic Class Overview Ophthalmic Antihistamines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Histamine and Antihistamines
ACTA FACULTATIS MEDICAE NAISSENSIS UDC: 615.218 DOI: 10.1515/afmnai-2015-0001 Review article Histamine and Antihistamines Nikola Stojković1, Snežana Cekić2, Milica Ristov3, Marko Ristić1, Davor Đukić1, Maša Binić1, Dragan Virijević1 1University of Niš, Faculty of Medicine, PhD student, Serbia 2Institute of Physiology, University of Niš, Faculty of Medicine , Serbia 3Doctor of Medicine SUMMARY In recent years, there has been a steady increase in the prevalence of allergic diseases. Allergic immune response represents a complex network of cellular events involving numerous immune cells and mediators. It represents the interaction of innate and acquired immune response. The key role in the immune cascade is taken by histamine, a natural component of the body, which in the allergic inflammatory response is releasesd by the mast cells and basophils. The aim of this study was to highlight the role of histamine in allergic immunological events, their effect on Th1 and Th2 subpopulation of lymphocytes and the production of the corresponding cytokines, as well as the role of histamine blockers in the treatment of these conditions. Histamine achieves its effect by binding to the four types of its receptors, which are widely distributed in the body. Histamine blockers block a numerous effects of histamine by binding to these receptors. As a highly selective second-generation antihistamine, cetirizine not only achieves its effects by binding to H1 receptors, but also attenuates numerous events during the inflammatory process. Knowledge of the effects -

Download Large Text CMI (PDF)
Children's Paedamin Antihistamine Oral Liquid Decongestant and Antihistamine Children 6-12 years Consumer Medicine Information What is in this leaflet? • Itchy, watery eyes Before you give • Nasal congestion Children's Paedamin This leaflet answers some common Children's Paedamin Decongestant Decongestant and questions about Children's and Antihistamine contains Antihistamine Paedamin® Decongestant and Diphenhydramine Hydrochloride Antihistamine. and Phenylephrine Hydrochloride. When you must not give it It does not contain all the available Diphenhydramine Hydrochloride Do not use Children's Paedamin information. It does not take the belongs to a group of medicines Decongestant and Antihistamine if place of talking to your doctor or called 'antihistamines'. you/ your child have an allergy to: pharmacist. Antihistamines help reduce allergic All medicines have risks and symptoms, such as sneezing, runny • any medicine containing benefits. Your doctor or pharmacist nose or itchy, watery eyes, by Diphenhydramine has weighed the risks of you/your preventing the effects of a substance Hydrochloride or other child taking Children's Paedamin called histamine. Histamine is antihistamines Decongestant and Antihistamine produced by the body in response to • any medicine containing against the benefits they expect it foreign substances that the body is Phenylephrine Hydrochloride will have for you. allergic to. • any of the ingredients listed at If you have any concerns about Phenylephrine Hydrochloride the end of this leaflet taking this medicine, ask your belongs to a group of medicines Some of the symptoms of an doctor or pharmacist. called decongestants. allergic reaction may include: Keep this leaflet with the It works by reducing congestion in • shortness of breath medicine. -

Inhibition of Histamine-Induced Human Conjunctival Epithelial Cell Responses by Ocular Allergy Drugs
LABORATORY SCIENCES Inhibition of Histamine-Induced Human Conjunctival Epithelial Cell Responses by Ocular Allergy Drugs John M. Yanni, PhD; Lori K. Weimer, BA; Najam A. Sharif, PhD; Shou X. Xu, MS; Daniel A. Gamache, PhD; Joan M. Spellman, MS Objective: To evaluate the effects of topical ocular drugs secretion (50% inhibitory concentration, 1.7-5.5 nmol/L) with histamine H1-antagonist activity on histamine- than predicted from binding data, while antazoline and stimulated phosphatidylinositol turnover and interleu- pheniramine were far less potent (20- to 140-fold) in func- kin (IL) 6 and IL-8 secretion from human conjunctival tional assays. Levocabastine (dissociation constant, 52.6 epithelial cells. nmol/L) exhibited greater functional activity (50% in- hibitory concentration, 8-25 nmol/L) than either antazo- Methods: Primary human conjunctival epithelial cell cul- line or pheniramine. tures were stimulated with histamine in the presence or ab- sence of test drugs. Phosphatidylinositol turnover was quan- Conclusions: Histamine-stimulated phosphatidylino- tified by ion exchange chromatography and cytokine con- sitol turnover and cytokine secretion by human conjunc- tentofsupernatantsbyenzyme-linkedimmunosorbentassay. tival epithelial cells are attenuated by compounds with H1-antagonist activity. However, antihistaminic po- Results: Antazoline hydrochloride, emedastine difuma- tency alone does not predict anti-inflammatory poten- rate, levocabastine hydrochloride, olopatadine hydro- tial. Olopatadine, emedastine, and levocabastine were no- chloride, and pheniramine maleate attenuated histamine- tably more potent than pheniramine and antazoline. stimulated phosphatidylinositol turnover and IL-6 and IL-8 secretion. Emedastine was the most potent in li- Clinical Relevance: Selected topical ocular drugs with gand binding, phosphatidylinositol turnover, and IL-6 se- antihistaminic activity may offer therapeutic advan- cretion, with dissociation constant and 50% inhibitory tages to patients with allergic conjunctivitis by inhibit- concentrations of 1-3 nmol/L. -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -

Emadine, INN-Emedastine
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT EMADINE 0.5 mg/ml, eye drops, solution 2. QUALITATIVE AND QUANTITATIVE COMPOSITION 1 ml of solution contains emedastine 0.5 mg (as difumarate) Excipient with known effect Benzalkonium chloride 0.1 mg/ml For the full list of excipients, see section 6.1 3. PHARMACEUTICAL FORM Eye drops, solution. Clear, colourless solution. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Symptomatic treatment of seasonal allergic conjunctivitis. 4.2 Posology and method of administration EMADINE has not been studied in clinical trials beyond six weeks. Posology The dose is one drop of EMADINE to be applied to the affected eye(s) twice daily. When used with other ophthalmic medicines, an interval of ten minutes should be allowed between applications of each medicinal product. Eye ointments should be administered last. Elderly population EMADINE has not been studied in elderly patients older than 65 years, and therefore its use is not recommended in this population. Paediatric population EMADINE may be used in paediatric patients (3 years of age and older) at the same posology as in adults. Hepatic and Renal impairment Use EMADINE has not been studied in these patients and therefore, its use is not recommended in this population. Method of administration For ocular use. 2 To prevent contamination of the dropper tip and solution, care should be taken not to touch the eyelids, surrounding areas or other surfaces with the dropper tip of the bottle. After cap is removed, if tamper evident snap collar is loose, remove before using product. -
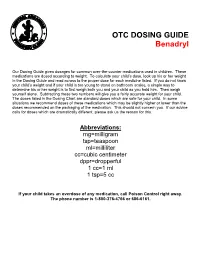
OTC DOSING GUIDE Benadryl
OTC DOSING GUIDE Benadryl Our Dosing Guide gives dosages for common over-the-counter medications used in children. These medications are dosed according to weight. To calculate your child’s dose, look up his or her weight in the Dosing Guide and read across to the proper dose for each medicine listed. If you do not know your child’s weight and if your child is too young to stand on bathroom scales, a simple way to determine his or her weight is to first weigh both you and your child as you hold him. Then weigh yourself alone. Subtracting these two numbers will give you a fairly accurate weight for your child. The doses listed in the Dosing Chart are standard doses which are safe for your child. In some situations we recommend doses of these medications which may be slightly higher or lower than the doses recommended on the packaging of the medication. This should not concern you. If our advice calls for doses which are dramatically different, please ask us the reason for this. Abbreviations: mg=milligram tsp=teaspoon ml=milliliter cc=cubic centimeter dppr=dropperful 1 cc=1 ml 1 tsp=5 cc If your child takes an overdose of any medication, call Poison Control right away. The phone number is 1-800-376-4766 or 686-6161. CHILDREN’S BENADRYL ALLERGY LIQUID (Generic Name: Diphenhydramine) (Antihistamine) NEVER GIVE TO INFANTS LESS THAN 6 MONTHS OLD. DO NOT GIVE TO CHILDREN LESS THAN 2 YEARS OLD UNLESS ADVISED BY A PHYSICIAN. Dosage: Every 4 -6 hours. -
Doxylamine Succinate-Pyridoxine Hydrochloride
Doxylamine succinate-pyridoxine hydrochloride This sheet is about exposure to doxylamine succinate-pyridoxine hydrochloride in pregnancy and while breastfeeding. This information should not take the place of medical care and advice from your healthcare providers. What is doxylamine succinate-pyridoxine hydrochloride? The combination of 10mg of doxylamine succinate and 10mg of pyridoxine hydrochloride is a medication used to treat nausea and vomiting of pregnancy (NVP), also called “morning sickness.” For more information on NVP, please see the MotherToBaby fact sheet Nausea and Vomiting of Pregnancy (https://mothertobaby.org/fact-sheets/nausea-vomiting-pregnancy-nvp/pdf/). Doxylamine succinate is an antihistamine. Antihistamines lessen the symptoms of allergic reactions and colds and help to treat insomnia (hard time sleeping). Pyridoxine hydrochloride is a form of vitamin B6. In the United States, the combination of doxylamine and pyridoxine has been sold under the name Diclegis® since 2013. In Canada, it has been sold under the brand name Diclectin®. Diclegis® and Diclectin® are delayed-release tablets available by prescription. Delayed-release means that the tablet coating prevents the ingredients from being absorbed too quickly by the body. Doxylamine succinate and/or pyridoxine hydrochloride may also be available as over-the- counter medicines. I take doxylamine succinate-pyridoxine hydrochloride. Can it make it harder for me to get pregnant? Based on the data available, it is not known if doxylamine succinate-pyridoxine hydrochloride can make it harder to become pregnant. I just found out I am pregnant. Should I stop taking doxylamine succinate-pyridoxine hydrochloride? Talk with your healthcare providers before making any changes to how you take your medication(s). -

Doxylamine/Pyridoxine
BonjestaTM (doxylamine/pyridoxine) – New Drug Approval • On November 7, 2016, the FDA approved Duchesnay’s Bonjesta (doxylamine/pyridoxine) for the treatment of nausea and vomiting of pregnancy in women who do not respond to conservative management. — Bonjesta has not been studied in women with hyperemesis gravidarum. • Bonjesta is a fixed dose combination product containing an antihistamine (doxylamine) and a vitamin B6 analog (pyridoxine). The exact mechanism of Bonjesta is not known. — Doxylamine/pyridoxine is also available as Diclegis®, which contains 10 mg of doxylamine and 10 mg of pyridoxine as delayed-release tablets for the same indication. • There have been no efficacy and safety trials for Bonjesta. However, a placebo-controlled study was conducted to support the safety and efficacy of 10 mg doxylamine succinate and 10 mg pyridoxine hydrochloride tablets (a different formulation and dosage strength than Bonjesta) in the treatment of nausea and vomiting of pregnancy. • Bonjesta is contraindicated in women with known hypersensitivity to doxylamine, other ethanolamine derivative antihistamines, or pyridoxine or any inactive ingredient in the formulation; monoamine oxidase (MAO) inhibitors intensify and prolong the adverse central nervous system effects of Bonjesta. • Warnings and precautions of Bonjesta include somnolence and concomitant medical conditions. • The most common adverse event (≥ 5% and exceeding placebo) with combination 10 mg doxylamine and 10 mg pyridoxine tablets was somnolence. • The recommended dose of Bonjesta is one tablet orally at bedtime on day 1. If the dose adequately controls symptoms the next day, the patient may continue taking one tablet daily at bedtime only. However, if symptoms persist on day 2, the dose may be increased to one tablet in the morning and one tablet at bedtime. -

Doxepin (Dox-E-Pin) Description: Tricyclic Antidepressant; Antihistamine Other Names for This Medication: Sinequan®, Silenor® Common Dosage Forms: Veterinary: None
Prescription Label Patient Name: Species: Drug Name & Strength: Directions (amount to give how often & for how long): Prescribing Veterinarian's Name & Contact Information: Refills: [Content to be provided by prescribing veterinarian] Doxepin (dox-e-pin) Description: Tricyclic Antidepressant; Antihistamine Other Names for this Medication: Sinequan®, Silenor® Common Dosage Forms: Veterinary: None. Human: 3 mg, 6 mg, 10 mg, 25 mg, 50 mg, 75 mg, 100 mg, & 150 mg capsules; 10 mg/mL oral liquid concentrates. This information sheet does not contain all available information for this medication. It is to help answer commonly asked questions and help you give the medication safely and effectively to your animal. If you have other questions or need more information about this medication, contact your veterinarian or pharmacist. Key Information When used as an antihistamine, doxepin should be used on a regular, ongoing basis in animals that respond to it. This drug works better if used before exposure to an allergen (eg, pollens). When used for behavior modification, it may take several days to weeks to determine if doxepin is effective. May be given with or without food. If your animal vomits or acts sick after receiving the drug on an empty stomach, try giving the next dose with food or a small treat. If vomiting continues, contact your veterinarian. Most common side effects are sleepiness, dry mouth, and constipation. Be sure your animal always has access to plenty of fresh, clean water. Rare side effects that can be serious (contact veterinarian immediately) include abnormal bleeding, lack of an appetite, seizures, collapse, or profound sleepiness. -

Histamine and Antihistamines Sites of Action Conditions Which Cause Release Aron H
Learning Objectives I Histamine Pharmacological effects Histamine and Antihistamines Sites of action Conditions which cause release Aron H. Lichtman, Ph.D. Diagnostic uses Associate Professor II Antihistamines acting at the H1 and H2 receptor Pharmacology and Toxicology Pharmacological effects Mechanisms of action Therapeutic uses Side effects and drug interactions Be familiar with the existence of the H3 receptor III Be able to describe the main mechanism of action of cromolyn sodium and its clinical uses Histamine Pharmacology First autacoid to be discovered. (Greek: autos=self; Histamine Formation akos=cure) Synthesized in 1907 Synthesized in mammalian tissues by Demonstrated to be a natural constituent of decarboxylation of the amino acid l-histidine mammalian tissues (1927) Involved in inflammatory and anaphylactic reactions. Local application causes swelling redness, and edema, mimicking a mild inflammatory reaction. Large systemic doses leads to profound vascular changes similar to those seen after shock or anaphylactic origin Histamine Stored in complex with: Heparin Chondroitin Sulfate Eosinophilic Chemotactic Factor Neutrophilic Chemotactic Factor Proteases 1 Conditions That Release Histamine 1. Tissue injury: Any physical or chemical agent that injures tissue, skin or mucosa are particularly sensitive to injury and will cause the immediate release of histamine from mast cells. 2. Allergic reactions: exposure of an antigen to a previously sensitized (exposed) subject can immediately trigger allergic reactions. If sensitized by IgE antibodies attached to their surface membranes will degranulate when exposed to the appropriate antigen and release histamine, ATP and other mediators. 3. Drugs and other foreign compounds: morphine, dextran, antimalarial drugs, dyes, antibiotic bases, alkaloids, amides, quaternary ammonium compounds, enzymes (phospholipase C). -

Marrakesh Agreement Establishing the World Trade Organization
No. 31874 Multilateral Marrakesh Agreement establishing the World Trade Organ ization (with final act, annexes and protocol). Concluded at Marrakesh on 15 April 1994 Authentic texts: English, French and Spanish. Registered by the Director-General of the World Trade Organization, acting on behalf of the Parties, on 1 June 1995. Multilat ral Accord de Marrakech instituant l©Organisation mondiale du commerce (avec acte final, annexes et protocole). Conclu Marrakech le 15 avril 1994 Textes authentiques : anglais, français et espagnol. Enregistré par le Directeur général de l'Organisation mondiale du com merce, agissant au nom des Parties, le 1er juin 1995. Vol. 1867, 1-31874 4_________United Nations — Treaty Series • Nations Unies — Recueil des Traités 1995 Table of contents Table des matières Indice [Volume 1867] FINAL ACT EMBODYING THE RESULTS OF THE URUGUAY ROUND OF MULTILATERAL TRADE NEGOTIATIONS ACTE FINAL REPRENANT LES RESULTATS DES NEGOCIATIONS COMMERCIALES MULTILATERALES DU CYCLE D©URUGUAY ACTA FINAL EN QUE SE INCORPOR N LOS RESULTADOS DE LA RONDA URUGUAY DE NEGOCIACIONES COMERCIALES MULTILATERALES SIGNATURES - SIGNATURES - FIRMAS MINISTERIAL DECISIONS, DECLARATIONS AND UNDERSTANDING DECISIONS, DECLARATIONS ET MEMORANDUM D©ACCORD MINISTERIELS DECISIONES, DECLARACIONES Y ENTEND MIENTO MINISTERIALES MARRAKESH AGREEMENT ESTABLISHING THE WORLD TRADE ORGANIZATION ACCORD DE MARRAKECH INSTITUANT L©ORGANISATION MONDIALE DU COMMERCE ACUERDO DE MARRAKECH POR EL QUE SE ESTABLECE LA ORGANIZACI N MUND1AL DEL COMERCIO ANNEX 1 ANNEXE 1 ANEXO 1 ANNEX -
A Practical Approach to Management of Allergic Eye Conditions in Children
Volume 6 No. 3, September 2010 Review Article A Practical Approach to Management of Allergic Eye Conditions in Children Dexter Yu-Lung LEUNG Hong Kong Eye Hospital; Department of Ophthalmology & Visual Sciences, The Chinese University of Hong Kong; and Hong Kong Ophthalmological Society, Hong Kong Introduction In USA, expenditure related to ocular prescription medication rose from US$6 million in early 1990s to While nasal allergy all along has been important in >US$200 million in the new millennium, projecting an allergy research, ocular allergy is now increasingly annual growth of 25% per year in USA.7 recognized as a distinct symptoms-and-signs complex that imposes significant disease burden with reduction of quality of life of patients. Allergic conjunctivitis is Classification highly prevalent in Hong Kong and has a close epidemiologic relationship with allergic rhinitis. The emphasis of this article will also be on what a paediatrician can do prior to the point of referral: recognition of the ocular symptoms, recognition of potential sight-threatening situations, and effective initial treatment. Disease burden While we are still awaiting published evidence for official incidence of ocular allergy in Hong Kong, a recent survey from the Eye Institute of the University of Hong Kong, conducted during May and June 2009 on 1,000 parents with children less than 12 years old in Hong Kong, has estimated that approximately 30% SAC and PAC are more common, and while they are of children suffered from eye allergy.1 symptomatic, they are less likely to result in long term ocular complications. VKC and AKC are rarer, more The incidence of ocular allergy varies in different chronic but are potentially associated with severe geographical regions and tends to be more common blinding ocular complications.