Proposal for Evaluating the Quality of Reports of Surgical Interventions in the Treatment of Trigeminal Neuralgia: the Surgical Trigeminal Neuralgia Score
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Indian S&T Journals in International Indexing and Abstracting Databases
Annals of Library and Information Studies Vol. 59, December 2012, pp. 247-279 Indian S&T journals in international indexing and abstracting databases: A study Rabishankar Giri1, Prakash Chand2 and B K Sen3 1Indira Gandhi Institute of Technology, GGS Indraprastha University, Kashmere Gate, Delhi-110006, Email: [email protected], 2,aEx-Scientist, CSIR-National Institute of Science Communication and Information Resources, 14-Satsang Vihar Marg, New Delhi – 110067, Email: [email protected] 3,bFormer Visiting Professor, University of Malaya, Malaysia, Email: [email protected] The coverage of Indian science and technology (S&T) periodicals in major international indexing and abstracting (I&A) services has been studied. It is found that about 1200 Indian S&T journals are being covered by at least one of the international I&A services and over 300 S&T journals are openly accessible. However, coverage of Indian S&T journals by major citation databases, Web of Science (WoS) & Scopus is relatively poor. The newly launched Indian Citation Index (ICI) promises to cover more Indian journals. Keywords: Indian S&T journals, indexing & abstracting services, citation measure, impact factor Introduction Zoological Record, Excerpta Medica/Embase. India is the world's second fastest growing Medline, Index Copernicus, Mathematical Reviews, economy only next to China, with a large R & D Zentralblatt MATH, INIS, GeoBase along with two infrastructure. According to a recent report of Ernst & citation databases Scopus and Science Citation Index Young, India’s current higher education spending is Expanded (SCI-E) besides DOAJ to understand the estimated at Rs. 4,620 billion and projected to grow new open access phenomenon. -
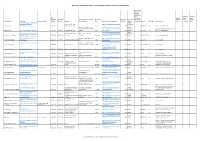
Open Access Journals Ohne Article Processing Charge Im Web of Science (Mit Impact Factor)
Open Access Journals ohne Article Processing Charge im Web of Science (mit Impact Factor) durchschnittl iche Dauer zwischen Einreichung und Im Science im Social ISSN Publikation im Sience Citation Sience (gedruckte ISSN (online herausgebende Gesellschaft Erscheinungs Open Access Sprache der eines Artikel Citation Index Citation Zeitschriftentitel Homepage alternativer Titel Version) Version) Verleger oder Institution land Webseite mit APC Information Inhalt ab Volltexte (in Wochen) Lizenze DOAJ Sigel Themenbereich Index expanded Index http://www.scielo.br/scielo.php/scr English, ipt_sci_serial/pid_0044- Instituto Nacional de http://www.scielo.br/revistas/aa/iins Portuguese, Acta Amazonica 5967/lng_en/nrm_iso/lng_en 0044-5967 Pesquisas da Amazônia Brazil truc.htm 2003 Spanish 22 CC BY-NC No Science: Science (General) x Universidad de Chile, Centro http://www.actabioethica.uchile.cl/i English, Interdisciplinario de Estudios en ndex.php/AB/about/submissions#aut Portuguese, Medicine: Medicine (General): Medical Acta Bioethica http://www.actabioethica.uchile.cl/ 0717-5906 1726-569X Universidad de Chile Bioética Chile horGuidelines 2000 Spanish 12 CC BY-SA No philosophy. Medical ethics x x http://www.revistas.unal.edu.co/ind English, http://www.revistas.unal.edu.co/in Universidad Nacional de Universidad Nacional de ex.php/actabiol/about/editorialPolici Portuguese, Acta Biológica Colombiana dex.php/actabiol 0120-548X 1900-1649 Colombia Colombia Colombia es#openAccessPolicy 2005 Spanish 13 CC BY-NC-SA No Science: Biology (General) x http://www.scielo.br/scielo.php/scr -

Measuring Growth and Impact of Neuroscience Researches in India: a Scientometric Analysis Based on Scopus
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Library Philosophy and Practice (e-journal) Libraries at University of Nebraska-Lincoln 2020 Measuring Growth and Impact of Neuroscience Researches in India: A Scientometric analysis based on Scopus Vinod Kumar Gautam Mr. Banaras Hindu University, [email protected] Rajani Mishra Banaras Hindu University, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/libphilprac Part of the Library and Information Science Commons Gautam, Vinod Kumar Mr. and Mishra, Rajani, "Measuring Growth and Impact of Neuroscience Researches in India: A Scientometric analysis based on Scopus" (2020). Library Philosophy and Practice (e-journal). 4447. https://digitalcommons.unl.edu/libphilprac/4447 Measuring Growth and Impact of Neuroscience Researches in India: A Scientometric analysis based on Scopus Vinod Kumar Gautam *Dr. Rajani Mishra (Research Scholar) (Associate Professor) Department of Library and Information Department of Library and Information Science Science BHU, Varanasi-221005 BHU, Varanasi-221005 Email. [email protected] Email: [email protected] Abstract Present study focuses on growth of neuroscience research in India and its impact on scholarly world. Total 4812 data were collected from Scopus database for the period of 2004-2018. Analysis of the data revealed considerable increase in Annual Growth Rate in neuroscience research with 10.52% CAGR for the entire period. Relative Growth Rate (RGR) was increasing with minor fluctuations i.e. growth in Neuroscience research is not exponential ratio rather than it is arithmetic ratio and Doubling Time is similar to RGR. Trend (Least Square) of the neuroscience publications showed an increase trend during the study period. -

(NIMHANS), India
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Library Philosophy and Practice (e-journal) Libraries at University of Nebraska-Lincoln Winter 1-29-2020 Scientometric analysis on scholarly communications of National Institute of Mental Health and Neurosciences (NIMHANS), India RADHAKRISHNAN NATARAJAN Periyar University, Salem, India, [email protected] Prabahar Ponniah Mr. Periyar University, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/libphilprac Part of the Library and Information Science Commons NATARAJAN, RADHAKRISHNAN and Ponniah, Prabahar Mr., "Scientometric analysis on scholarly communications of National Institute of Mental Health and Neurosciences (NIMHANS), India" (2020). Library Philosophy and Practice (e-journal). 3934. https://digitalcommons.unl.edu/libphilprac/3934 Scientometric analysis on scholarly communications of National Institute of Mental Health and Neurosciences (NIMHANS), India PonniahPrabahar1 and Natarajan Radhakrishnan2 Research Student1 Professor2 Department of Library and Information Science Periyar University, Salem- 636 011 India E-mail:[email protected] E-mail:[email protected] Abstract: The study investigated the research publications of the National Institute of Mental Health and Neurosciences (NIMHANS) during the period 2009-2018 as reflected in Web of Science database. The results show that 1694 papers were published and gained 20158 citations. The average number of citations per paper identified is 11.89%. Neuroscience Neurology, Psychiatry, and Surgery are the most preferred domains to publish the articles. The global collaboration of NIMHANS is mostly with the USA, England, and Australia. The degree of collaboration is 0.99. The researchers of NIMHANS prefer to publish their papers in Indian journals. Lotka's law was tested to measure the scientific productivity of authors. -

Fate of Submitted Manuscripts Rejected from the American Journal of Neuroradiology: Outcomes RESEARCH PERSPECTIVES and Commentary
Fate of Submitted Manuscripts Rejected from the American Journal of Neuroradiology: Outcomes RESEARCH PERSPECTIVES and Commentary R.J. McDonald BACKGROUND AND PURPOSE: The purpose of this study was to determine the publication fate of H.J. Cloft submissions previously rejected from the American Journal of Neuroradiology (AJNR) to provide guidance to authors who receive rejection notices. D.F. Kallmes MATERIALS AND METHODS: A retrospective search by using MEDLINE of all submissions rejected from AJNR in 2004 was performed to identify subsequently published manuscripts. The fate of subsequently published manuscripts was analyzed as a function of submission type (major study, technical note, or case report), publication delay, publishing journal type (neuroradiology, general radiology, or clinical neuroscience journal), impact factor, publication volume, and circulation volume. RESULTS: Of the 554 rejected submissions to AJNR, 315 (56%) were subsequently published in 115 different journals, with the journal Neuroradiology publishing the greatest number of articles (37 [12%] of 315). The mean publication delay was 15.8 Ϯ 7.5 months. Major studies were more likely than case reports to be subsequently published (P ϭ .034), but all 3 subtypes were published at rates greater than 50%. Radiologic journals collectively published approximately 60% of subsequent publications, whereas neurosurgery and neurology journals published 27% of rejected manuscripts. The mean impact factor of journals subsequently publishing rejected manuscripts was 1.8 Ϯ 1.3 (AJNR ϭ 2.5), and 24 (7.5%) manuscripts were subsequently published in journals with higher impact factors than AJNR. CONCLUSIONS: These findings should give hope to authors receiving a rejection from AJNR, because greater than 50% of articles rejected from AJNR are subsequently published within 2–3 years, irrespective of publication type, into high-quality journals. -

Parkinson's Disease Research by India
Gupta BM, et al., J Brain Neursci 2021, 5: 017 HSOA Journal of Brain & Neuroscience Research Research Article neurodegenerative disease [1-3]. As the PD disease worsens, non- Parkinson’s Disease Research by motor symptoms begin to impact the quality of life [4,5]. The pathological features of the Parkinson disease result from the India: A Scientometric Assessment substantial cell loss or cell deaths in the substantianigra (a region of the midbrain) [4] and the concomitant loss of Dopamine (DA) of Publications Output for the neurotransmitter or not enough dopamine in this region of the brain. Though the cause of cell death is poorly understood, but it does Period 1990-2019 involve the build-up or deposition of proteins within the brain as intracellular inclusions called Lewy bodies in the neurons [4,6,7]. 1 2 Gupta BM * and Dhawan SM The disease is clinically manifested after the death of ~70% of these 1CSIR-NISTADS, New Delhi, India neurons [4,6]. The symptoms usually emerge slowly [4]. Early in the 2CSIR-NPL, New Delhi, India disease, the most obvious symptoms are shaking, rigidity, slowness of movement, and difficulty with walking [4]. Thinking and behavioral problems may also occur [2]. Dementia becomes common in the advanced stages of the disease [7]. Depression and anxiety are also Abstract common, occurring in more than a third of people with PD [5]. Other symptoms include sensory, sleep, and emotional problems [1,2]. The The paper analyzes Parkinson’s disease research publications main motor symptoms are collectively called “parkinsonism” or a output by India in the global context using bibliometric indicators “parkinsonian syndrome” [4,6]. -

Open Access : India Is Moving Towards Third World Superpower
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by E-LIS Open Access : India is moving towards Third world Superpower Dr (Smt) Mangala Hirwade Dr (Smt) D. Rajyalakshmi Librarian Reader and Head Shivaji Science College DLIS, RTM Nagpur University Congress Nagar, Nagpur Nagpur [email protected] [email protected] Abstract The past few years have seen tremendous developments in information production, acquisition, and dissemination. Budgetary restrictions in research libraries have led to a period known as the serial cutting era. The new millennium has also ushered in the concept of the virtual library with seamless access to an integrated collection of print, electronic, and multimedia resources regardless of their physical location or ownership. Research scientists, policy makers, and reference librarians the world over are coming together to introduce reforms to make scientific knowledge affordable. Providing access to information free of charge in electronic formats is a concept that is gaining momentum. Open Access is one step ahead of Free Access. Open Access holds promise to remove both price and permission barriers to the scientific communication by using Internet. The present paper outlines the features of open access and the two vehicles viz. open access journals and open access archives. A few current open access initiatives in India are described in detail. In India, there is a large opportunity for open access publishing but still the number of registered archives is very less. Indian scientific communities and organizations like Indian Academy of Sciences, Indian Institute of Science, Indian National Science Academy, NISCAIR, INFLIBNET, etc are now actively taking initiatives towards creation of institutional repositories and providing open access to their publications. -

Open Access to Scholarly Literature in India — a Status Report (With Emphasis on Scientific Literature)
Open Access to Scholarly Literature in India — A Status Report (with Emphasis on Scientific Literature) Prof. Subbiah Arunachalam Madhan Muthu Centre for Internet and Society, Bangalore, India 9 April 2011 (Draft) Page | 1 Table of Contents Chapter 1: Scholarly Communication........................................................................... 4 Introduction ............................................................................................................... 4 Scholarly Communication ......................................................................................... 4 Scholarly Communication and Evaluation of Science .............................................. 8 Chapter 2: Science in India ......................................................................................... 12 Structure and Organization of Science in India....................................................... 12 Changing face of Indian Science ............................................................................. 13 Chapter 3: Open Access .............................................................................................. 16 What is Open Access? ............................................................................................. 16 Why Open Access?.................................................................................................. 17 Chapter 4: Open Access in India................................................................................. 24 Box 1, Vidhanidhi (Electronic Theses and Dissertations)...................................... -

Comparison of Web of Science and Scopus Impact Factors of Indian Journals
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Library Philosophy and Practice (e-journal) Libraries at University of Nebraska-Lincoln 2-2011 Comparison of Web of Science and Scopus Impact Factors of Indian Journals Aragudige Nagaraja SriKrishna Institute of Technology, [email protected] M. Vasanthakumar Adichunchanagiri Institute of Medical Sciences, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/libphilprac Part of the Library and Information Science Commons Nagaraja, Aragudige and Vasanthakumar, M., "Comparison of Web of Science and Scopus Impact Factors of Indian Journals" (2011). Library Philosophy and Practice (e-journal). 596. https://digitalcommons.unl.edu/libphilprac/596 Library Philosophy and Practice 2011 ISSN 1522-0222 Comparison of Web of Science and Scopus Impact Factors of Indian Journals Aragudige Nagaraja Librarian SriKrishna Institute of Technology Hesaraghatta Road Chikkabanavara Post Bangalore, India Dr. M Vasanthakumar Senior Librarian Adichunchanagiri Institute of Medical Sciences Nagamangala Taluk Mandya District, Karnataka, India Introduction Many periodicals and magazines have been published in India. The Directory of Indian Scientific Periodicals published from Council for Scientific and Industrial Research (CSIR) New Delhi provides information about 2000 journals published from India. Every year library budgets are decreasing. Hence librarians are facing difficulties when selecting journals for collection development. Since few national or international systematic approaches exist for journal selection, this article asserts that the best methods for librarians often include the following: 1. Check the catalogue or collections of journals subscribed by similar type libraries. 2. Measure the opinion of subject experts working in the same organization or others by survey or other scientific methods. -

Conversion of Thesis to Peer-Reviewed Publication
Published online: 27.08.2019 THIEME Original Article 93 Conversion of Thesis to Peer-Reviewed Publication Dhaval Shukla1 Manjul Tripathi2 Bhagavatula Indira Devi1 1Department of Neurosurgery, National Institute of Mental Health Address for correspondence Dhaval Shukla, MCh, Department of and Neurosciences, Bangalore, India Neurosurgery, National Institute of Mental Health and Neurosciences, 2Department of Neurosurgery, Postgraduate Institute of Medical Bangalore 560029, India (e-mail: [email protected]). Education and Research, Chandigarh, India Indian J Neurosurg 2019;8:93–98 Abstract Introduction Writing a thesis or dissertation during a postgraduate medical or surgi- cal training is a part of curriculum, which is considered a major component of training during residency. We aimed to analyze and find out the fate of thesis of our residents, their outcome, and impact. We have also evaluated the reasons for not publishing the thesis in a peer-reviewed paper. Methods This study was conducted at a neurosurgical department of a premier training institute. PubMed and Google Scholar were searched for the topics of thesis and names of residents to find out whether any paper was published similar to topic of thesis. The faculties and residents were also personally contacted to evaluate the publication status of their thesis. A questionnaire was sent to the students who did not publish their thesis to find out the reasons for not submitting for publication. Results Total 56 residents submitted 85 thesis. The conversion rate to peer-reviewed Keywords publication was 32.5%. There was decreasing trend of conversion to publication over ► thesis 10 years. The most common reasons for not publishing was a bad design of study, or ► dissertation deemed worthless for publication. -

India's Efforts in Open Access Publishing
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by UNL | Libraries University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Library Philosophy and Practice (e-journal) Libraries at University of Nebraska-Lincoln 5-2012 India's Efforts in Open Access Publishing Bhaskar Mukherjee Banaras Hindu University, Varanasi, Uttar Pradesh, India, [email protected] Bidyut Kumar Mal VBS Purvanchal University Follow this and additional works at: https://digitalcommons.unl.edu/libphilprac Part of the Library and Information Science Commons Mukherjee, Bhaskar and Kumar Mal, Bidyut, "India's Efforts in Open Access Publishing" (2012). Library Philosophy and Practice (e-journal). 751. https://digitalcommons.unl.edu/libphilprac/751 http://unllib.unl.edu/LPP/ Library Philosophy and Practice 2012 ISSN 1522-0222 India's Efforts in Open Access Publishing Bhaskar Mukherjee Assistant Professor Department of Library & Information Science Banaras Hindu University Varanasi, U.P. Bidyut Kumar Mal In-Charge Vivekanand Central Library VBS Purvanchal University JAUNPUR-222001(U.P.) Introduction For a long time, India has been generating a great deal of scholarly resources in all disciplines. After independence, there was a lot of investment in science and technology, and S&T were used to leverage development efforts and to improve the standard of living. However, one in four Indians still lives below the poverty line. There is a considerable research effort in a wide variety of areas including science, -

Open Access Publishing in Indian Premier Research Institutions Page 1 of 11
Open access publishing in Indian premier research institutions Page 1 of 11 VOL. 14 NO. 3, SEPTEMBER, 2009 Contents | Author index | Subject index | Search | Home Open access publishing in Indian premier research institutions Mohammad Hanief Bhat Islamia College of Science & Commerce, Srinagar (J&K), India 190002 Abstract Introduction. Publishing research findings in open access journals is a means of enhancing visibility and consequently increasing the impact of publications. This study provides an overview of open access publishing in premier research institutes of India. Method. The publication output of each institution from 2003 to 2007 was ascertained through Scopus and the name of source journals along with the number of publications recorded. All 4232 journal titles were searched in the Directory of Open Access Journals and then using the Google search engine to find out which journals are openly accessible. Analysis. The data are tabulated and analysed in a systematic way to reveal findings in accordance with desired objectives. Results. The 17,516 research articles are contributed by the five institutions and appear in 4232 journals. The Indian Institute of Science publishes 8.26% of its research output in open access journals, All India Institute of Medical Sciences 19.37%, Baba Atomic Research Centre 4.84%, Indian Institute of Technology, Delhi 3.04% and Indian Institute of Technology, Kharagpur 3.26%. Conclusions. The study reveals that a small portion of research publications of Indian research institutes is published in open access journals, the majority in journals of Indian origin. The medical institutions are contributing more of their publications to open access journals compared to other institutions.