Structural Modeling of Tissue-Specific Mitochondrial Alanyl-Trna Synthetase (AARS2) Defects Predicts Differential Effects On
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

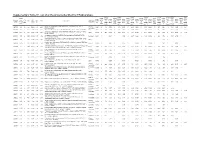
Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Abstracts from the 50Th European Society of Human Genetics Conference: Electronic Posters
European Journal of Human Genetics (2019) 26:820–1023 https://doi.org/10.1038/s41431-018-0248-6 ABSTRACT Abstracts from the 50th European Society of Human Genetics Conference: Electronic Posters Copenhagen, Denmark, May 27–30, 2017 Published online: 1 October 2018 © European Society of Human Genetics 2018 The ESHG 2017 marks the 50th Anniversary of the first ESHG Conference which took place in Copenhagen in 1967. Additional information about the event may be found on the conference website: https://2017.eshg.org/ Sponsorship: Publication of this supplement is sponsored by the European Society of Human Genetics. All authors were asked to address any potential bias in their abstract and to declare any competing financial interests. These disclosures are listed at the end of each abstract. Contributions of up to EUR 10 000 (ten thousand euros, or equivalent value in kind) per year per company are considered "modest". Contributions above EUR 10 000 per year are considered "significant". 1234567890();,: 1234567890();,: E-P01 Reproductive Genetics/Prenatal and fetal echocardiography. The molecular karyotyping Genetics revealed a gain in 8p11.22-p23.1 region with a size of 27.2 Mb containing 122 OMIM gene and a loss in 8p23.1- E-P01.02 p23.3 region with a size of 6.8 Mb containing 15 OMIM Prenatal diagnosis in a case of 8p inverted gene. The findings were correlated with 8p inverted dupli- duplication deletion syndrome cation deletion syndrome. Conclusion: Our study empha- sizes the importance of using additional molecular O¨. Kırbıyık, K. M. Erdog˘an, O¨.O¨zer Kaya, B. O¨zyılmaz, cytogenetic methods in clinical follow-up of complex Y. -

Supplementary Data.Xlsx
Electronic Supplementary Material (ESI) for Molecular BioSystems. This journal is © The Royal Society of Chemistry 2016 Average Average spectral spectral Fold UniProt IDGene Protein Name counts- counts- enrichm negative positive ent sample sample P12821 ACE HUMAN - ACE Angiotensin-converting enzyme 0 79.75 #DIV/0! Q71U36 TBA1A HUMAN - TUBA1A Tubulin alpha-1A chain 0 59.5 #DIV/0! P17812 PYRG1 HUMAN - CTPS1 CTP synthase 1 0 43.5 #DIV/0! P23921 RIR1 HUMAN - RRM1 Ribonucleoside-diphosphate reductase large subunit 0 35 #DIV/0! P49915GUAA HUMAN - GMPS GMP synthase 0 30.5 #DIV/0! P30153 2AAA HUMAN - PPP2R1A Serine/threonine-protein phosphatase 2A 65 kDa0 regulatory subunit29 A#DIV/0! alpha isoform P55786 PSA HUMAN - NPEPPS Puromycin-sensitive aminopeptidase 0 28.75 #DIV/0! O43143 DHX15 HUMAN - DHX15 Putative pre-mRNA-splicing factor ATP-dependent RNA0 helicase28.25 DHX15#DIV/0! P15170 ERF3A HUMAN - GSPT1 Eukaryotic peptide chain release factor GTP-binding0 subunit ERF3A24.75 #DIV/0! P09874PARP1HUMAN - PARP1 Poly 0 23.5 #DIV/0! Q9BXJ9 NAA15 HUMAN - NAA15 N-alpha-acetyltransferase 15, NatA auxiliary subunit0 23 #DIV/0! B0V043 B0V043 HUMAN - VARS Valyl-tRNA synthetase 0 20 #DIV/0! Q86VP6 CAND1 HUMAN - CAND1 Cullin-associated NEDD8-dissociated protein 1 0 19.5 #DIV/0! P04080CYTB HUMAN - CSTB Cystatin-B 0 19 #DIV/0! Q93009 UBP7 HUMAN - USP7 Ubiquitin carboxyl-terminal hydrolase 7 0 18 #DIV/0! Q9Y2L1 RRP44 HUMAN - DIS3 Exosome complex exonuclease RRP44 0 18 #DIV/0! Q13748 TBA3C HUMAN - TUBA3D Tubulin alpha-3C/D chain 0 18 #DIV/0! P29144 TPP2 HUMAN -

Autocrine IFN Signaling Inducing Profibrotic Fibroblast Responses By
Downloaded from http://www.jimmunol.org/ by guest on September 23, 2021 Inducing is online at: average * The Journal of Immunology , 11 of which you can access for free at: 2013; 191:2956-2966; Prepublished online 16 from submission to initial decision 4 weeks from acceptance to publication August 2013; doi: 10.4049/jimmunol.1300376 http://www.jimmunol.org/content/191/6/2956 A Synthetic TLR3 Ligand Mitigates Profibrotic Fibroblast Responses by Autocrine IFN Signaling Feng Fang, Kohtaro Ooka, Xiaoyong Sun, Ruchi Shah, Swati Bhattacharyya, Jun Wei and John Varga J Immunol cites 49 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html http://www.jimmunol.org/content/suppl/2013/08/20/jimmunol.130037 6.DC1 This article http://www.jimmunol.org/content/191/6/2956.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2013 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 23, 2021. The Journal of Immunology A Synthetic TLR3 Ligand Mitigates Profibrotic Fibroblast Responses by Inducing Autocrine IFN Signaling Feng Fang,* Kohtaro Ooka,* Xiaoyong Sun,† Ruchi Shah,* Swati Bhattacharyya,* Jun Wei,* and John Varga* Activation of TLR3 by exogenous microbial ligands or endogenous injury-associated ligands leads to production of type I IFN. -

The Promise of Whole-Exome Sequencing in Medical Genetics
Journal of Human Genetics (2014) 59, 5–15 & 2014 The Japan Society of Human Genetics All rights reserved 1434-5161/14 www.nature.com/jhg REVIEW The promise of whole-exome sequencing in medical genetics Bahareh Rabbani1, Mustafa Tekin2 and Nejat Mahdieh3 Massively parallel DNA-sequencing systems provide sequence of huge numbers of different DNA strands at once. These technologies are revolutionizing our understanding in medical genetics, accelerating health-improvement projects, and ushering to a fully understood personalized medicine in near future. Whole-exome sequencing (WES) is application of the next-generation technology to determine the variations of all coding regions, or exons, of known genes. WES provides coverage of more than 95% of the exons, which contains 85% of disease-causing mutations in Mendelian disorders and many disease-predisposing SNPs throughout the genome. The role of more than 150 genes has been distinguished by means of WES, and this statistics is quickly growing. In this review, the impacts of WES in medical genetics as well as its consequences leading to improve health care are summarized. Journal of Human Genetics (2014) 59, 5–15; doi:10.1038/jhg.2013.114; published online 7 November 2013 Keywords: cancer; common disease; medical genomics; Mendelian disorder; whole-exome sequencing INTRODUCTION VALUE OF WES IN MEDICINE DNA sequencing is one of the main concerns of medical research Human genome comprises B3 Â 109 bases having coding and nowadays. Union of chain termination sequencing by Sanger et al.1 noncoding sequences. About 3 Â 107 base pairs (1%) (30 Mb) of and the polymerase chain reaction (PCR) by Mullis et al.2 established the genome are the coding sequences. -

Hormone and Inhibitor Treatment T47DM Cells Were Used for All Experiments Unless Otherwise Stated
Extended Data Extended Materials Methods Cell culture; hormone and inhibitor treatment T47DM cells were used for all experiments unless otherwise stated. For hormone induction experiments, cells were grown in RPMI medium without Phenol Red, supplemented with 10% dextran-coated charcoal-treated FBS (DCC/FBS) after 24 h in serum-free conditions; cells were incubated with R5020 (10 nM) or vehicle (ethanol) as described (Vicent et al. 2011). For hormone induction experiments in MCF7 cells a similar procedure was performed; cells were grown in DMEM medium without Phenol Red, supplemented with 10% dextran-coated charcoal-treated FBS (DCC/FBS) after 24 h in serum-free conditions; cells were incubated with Estradiol (10 nM) or vehicle (ethanol). PARG and PARP inhibition were carried out via incubating cells with 5uM TA (tannic acid) or 10uM 3AB (3-amino-benzamide) respectively 1 hour prior to hormone treatment. All transfections were performed using Lipofectamine2000 (Invitrogen) according to manufacturers instructions. PAR-capture ELISA Hormone and or inhibitor treatments were carried out as described, and sample preparation was carried out as follows: At the required time point, cells were washed twice with ice-cold PBS and scraped in lysis buffer (0.4 M NaCl, 1% Triton X-100) plus protease inhibitors. Cell suspensions were then incubated for 30 min on ice with periodic vortexing. The disrupted cell suspension was centrifuged at 10,000g for 10 min at 4°C, and the supernatant was recovered, snap-frozen, and stored at 80°C until required. Ninety-six-well black-walled plates were incubated with 2 ng/mL anti-PAR monoclonal antibody (Trevigen) in 50 mM sodium carbonate (pH 7.6) overnight at 4°C. -

Anti-AARS2 (Internal Region) Polyclonal Antibody (DPAB-DC2592) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-AARS2 (internal region) polyclonal antibody (DPAB-DC2592) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description The protein encoded by this gene belongs to the class-II aminoacyl-tRNA synthetase family. Aminoacyl-tRNA synthetases play critical roles in mRNA translation by charging tRNAs with their cognate amino acids. The encoded protein is a mitochondrial enzyme that specifically aminoacylates alanyl-tRNA. Mutations in this gene are a cause of combined oxidative phosphorylation deficiency 8. Immunogen A synthetic peptide corresponding to amino acids 478-489 at internal region of human AARS2. The sequence is CQHRARQAEPVQK Source/Host Goat Species Reactivity Human Purification Antigen affinity purification Conjugate Unconjugated Applications WB (Transfected lysate), ELISA, Format Liquid Concentration 0.5 mg/mL Size 100 μg Buffer In Tris saline, pH 7.3 (0.02% sodium azide, 0.5% BSA) Preservative 0.02% Sodium Azide Storage Store at -20°C.Aliquot to avoid repeated freezing and thawing. GENE INFORMATION Gene Name AARS2 alanyl-tRNA synthetase 2, mitochondrial [ Homo sapiens (human) ] Official Symbol AARS2 Synonyms AARS2; alanyl-tRNA synthetase 2, mitochondrial; AARSL; COXPD8; MTALARS; MT-ALARS; 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved alanine--tRNA ligase, mitochondrial; alanyl-tRNA synthetase like; probable alanyl-tRNA synthetase, mitochondrial; alanine -

Impact of Exome Sequencing in Characterizing Mendelian Disorders
Journal of Human Genetics (2012) 57, 621–632 & 2012 The Japan Society of Human Genetics All rights reserved 1434-5161/12 $32.00 www.nature.com/jhg REVIEW Next-generation sequencing: impact of exome sequencing in characterizing Mendelian disorders Bahareh Rabbani1, Nejat Mahdieh1, Kazuyoshi Hosomichi, Hirofumi Nakaoka and Ituro Inoue Traditional approaches for gene mapping from candidate gene studies to positional cloning strategies have been applied for Mendelian disorders. Since 2005, next-generation sequencing (NGS) technologies are improving as rapid, high-throughput and cost-effective approaches to fulfill medical sciences and research demands. Using NGS, the underlying causative genes are directly distinguished via a systematic filtering, in which the identified gene variants are checked for novelty and functionality. During the past 2 years, the role of more than 100 genes has been distinguished in rare Mendelian disorders by means of whole-exome sequencing (WES). Combination of WES with traditional approaches, consistent with linkage analysis, has had the greatest impact on those disorders following autosomal mode of inheritance; in more than 60 identified genes, the causal variants have been transmitted at homozygous or compound heterozygous state. Recent literatures focusing on identified new causal genes in Mendelian disorders using WES are reviewed in the present survey. Journal of Human Genetics (2012) 57, 621–632; doi:10.1038/jhg.2012.91; published online 26 July 2012 Keywords: exome sequencing; mendelian disorder; mutation; next-generation sequencing; NGS; WES INTRODUCTION genes and 4535 disorders with known molecular basis (http:// One of the major concerns of medical sciences is finding the causal omim.org/statistics/geneMap). -

Overexpression of Human Mitochondrial Alanyl-Trna Synthetase Suppresses Biochemical Defects of the Mt-Trnaala Mutation in Cybrid
Int. J. Biol. Sci. 2018, Vol. 14 1437 Ivyspring International Publisher International Journal of Biological Sciences 2018; 14(11): 1437-1444. doi: 10.7150/ijbs.27043 Research Paper Overexpression of human mitochondrial alanyl-tRNA synthetase suppresses biochemical defects of the mt-tRNAAla mutation in cybrids Xiaoxu Zhao1,2#, Jiamin Han1,2#, Ling Zhu1,Yun Xiao2, Chenghui Wang1,2, Fang Hong1, Pingping Jiang1,2, 1,2 Min-Xin Guan 1. Division of Medical Genetics and Genomics, The Children’s Hospital, Zhejiang University School of Medicine, Hangzhou, 310058, China. 2. Institute of Genetics Zhejiang University, and Department of Human Genetics, Zhejiang University School of Medicine, Hangzhou, 310058, China. # These two authors contributed equally to this work. Corresponding author: Pingping Jiang, Ph.D., Institute of Genetics Zhejiang University, and Department of Human Genetics, Zhejiang University School of Medicine, Hangzhou 310058, China. Telephone: 86-571-88982356; FAX: 86-571-88982377; E-mail: [email protected] © Ivyspring International Publisher. This is an open access article distributed under the terms of the Creative Commons Attribution (CC BY-NC) license (https://creativecommons.org/licenses/by-nc/4.0/). See http://ivyspring.com/terms for full terms and conditions. Received: 2018.05.03; Accepted: 2018.07.17; Published: 2018.08.06 Abstract Mutations of mitochondrial transfer RNAs (mt-tRNAs) play a major role in a wide range of mitochondrial diseases because of the vital role of these molecules in mitochondrial translation. It has previously been reported that the overexpression of mitochondrial aminoacyl tRNA synthetases is effective at partially suppressing the defects resulting from mutations in their cognate mt-tRNAs in cells. -
Supplementary Table S1. List of All the Proteins Identified by Itraq Analysis
Supplementary Table S1. List of all the proteins identified by iTRAQ analysis. OVSA OVISE OVMA RMG- JHOS4 OVCA OVSA SKOV Seque OVISE OVMA RMG- JHOS4 OVCA OVSA HO/H SKOV # OVISE /HOSE OVMA NA/HO RMG- I/HOS JHOS4 /HOSE OVCA R3/HO HO/H SKOV 3/HOS Accession nce MW calc. Subcellular /HOSE NA/HO I/HOS /HOSE R3/HO HO/H OSE2 3/HOS Pept # AAs Score Protein name /HOSE 2C NA/HO SE2C I/HOS E2C /HOSE 2C R3/HO SE2C OSE2 3/HOS E2C number covera [kDa] pI localization 2C SE2C E2C 2C SE2C OSE2 C E2C ides 2C Variabi SE2C Variabi E2C Variabi 2C Variabi SE2C Variabi C E2C Variabi ge(%) Count Count Count Count Count C Variabi Count lity [%] lity [%] lity [%] lity [%] lity [%] Count lity [%] lity [%] Extended synaptotagmin-2 OS=Homo sapiens GN=ESYT2 PE=1 SV=1 - Plasma A0FGR8 13.9 10 921 102.29 9.26 421.7 1.043 12 19.8 0.758 9 15.3 0.969 11 43.5 1.080 11 27.3 0.800 10 34.7 3.281 12 74.1 1.430 9 38.6 [ESYT2_HUMAN] membrane A0MZ66 3.65 2 631 71.60 5.33 49.5 Shootin-1 OS=Homo sapiens GN=KIAA1598 PE=1 SV=4 - [SHOT1_HUMAN] Other 2.515 3 33.6 1.495 3 13.1 1.985 2 56.9 1.684 3 5.4 1.561 3 31.4 1.881 3 22.2 2.783 3 32.1 Acetolactate synthase-like protein OS=Homo sapiens GN=ILVBL PE=1 SV=2 - A1L0T0 10.13 5 632 67.82 8.15 231.2 Other 0.820 4 20.3 0.675 4 37.0 0.833 4 37.6 0.880 4 44.3 0.789 4 37.8 3.677 4 78.5 0.929 4 13.0 [ILVBL_HUMAN] Uncharacterized protein KIAA0564 OS=Homo sapiens GN=KIAA0564 PE=1 A3KMH1 1.15 2 1905 214.69 7.40 30.9 Secreted 0.934 1 0.661 1 1.650 2 28.7 1.928 2 18.0 0.949 2 38.8 1.748 2 10.7 2.450 1 SV=2 - [K0564_HUMAN] WD repeat-containing protein -

Clinical and Genetic Studies in Paediatric Mitochondrial Disease
Clinical and Genetic Studies in Paediatric Mitochondrial Disease Yehani N.G.G. Wedatilake Genetics and Genomic Medicine Programme UCL Great Ormond Street Institute of Child Health University College London January 2017 A thesis submitted for the degree of Doctor of Philosophy awarded by University College London 1 Declaration I, Yehani N.G.G Wedatilake, confirm that the work presented in this thesis is my own. Where information has been derived from other sources, I confirm that this has been indicated in the thesis. Signed ______________________________________________________________ 2 Abstract Paediatric mitochondrial disease is a clinically and genetically heterogeneous group of disorders. Prior to the advent of next generation sequencing, many patients did not receive a genetic diagnosis. Genetic diagnosis is important for prognostication and prenatal diagnosis. The aim of this thesis was to study the genetic aetiology of paediatric mitochondrial disease. Paediatric patients with suspected mitochondrial disease were grouped to facilitate studying the genetic aetiology. This included grouping patients by respiratory chain enzyme deficiency, by affected end-organ type (cardiomyopathy) or by collectively investigating patients presenting with a similar, genetically undefined clinical syndrome. Whole exome sequencing (WES) was used to investigate genetic causes in patients with suspected mitochondrial disease associated with cytochrome c oxidase (COX) deficiency. In another paediatric cohort with mitochondrial cardiomyopathy, mitochondrial DNA sequencing, candidate gene sequencing or WES were used to identify genetic causes. Two families with a unique syndrome (febrile episodes, sideroblastic anaemia and immunodeficiency) were investigated using WES or homozygosity mapping. Candidate genes were functionally evaluated including the use of animal models. Furthermore a natural history study was performed in a monogenic mitochondrial disease (SURF1 deficiency) using clinical data from 12 centres. -

Molecular Epidemiology of Mitochondrial Cardiomyopathy:A Search Among Mitochondrial and Nuclear Genes
International Journal of Molecular Sciences Review Molecular Epidemiology of Mitochondrial Cardiomyopathy: A Search Among Mitochondrial and Nuclear Genes Cristina Mazzaccara 1,2,*,† , Bruno Mirra 1,2,†, Ferdinando Barretta 1,2, Martina Caiazza 3,4 , Barbara Lombardo 1,2 , Olga Scudiero 1,2 , Nadia Tinto 1,2 , Giuseppe Limongelli 3,4 and Giulia Frisso 1,2 1 Department of Molecular Medicine and Medical Biotechnology, University of Naples Federico II, 80131 Naples, Italy; [email protected] (B.M.); [email protected] (F.B.); [email protected] (B.L.); [email protected] (O.S.); [email protected] (N.T.); [email protected] (G.F.) 2 CEINGE Advanced Biotechnologies, 80145 Naples, Italy 3 Monaldi Hospital, AO Colli, 80131 Naples, Italy; [email protected] (M.C.); [email protected] (G.L.) 4 Department of Translational Medical Sciences, University of Campania “Luigi Vanvitelli”, 80134 Naples, Italy * Correspondence: [email protected]; Tel.: +39-0817-462-422 † These authors equally contributed to the paper. Abstract: Mitochondrial Cardiomyopathy (MCM) is a common manifestation of multi-organ Mi- tochondrial Diseases (MDs), occasionally present in non-syndromic cases. Diagnosis of MCM is complex because of wide clinical and genetic heterogeneity and requires medical, laboratory, and neuroimaging investigations. Currently, the molecular screening for MCM is fundamental part of Citation: Mazzaccara, C.; Mirra, B.; MDs management and allows achieving the definitive diagnosis. In this article, we review the current Barretta, F.; Caiazza, M.; Lombardo, genetic knowledge associated with MDs, focusing on diagnosis of MCM and MDs showing cardiac B.; Scudiero, O.; Tinto, N.; Limongelli, involvement. We searched for publications on mitochondrial and nuclear genes involved in MCM, G.; Frisso, G.