Patient Assessment Definitions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Baseline Vitals &
Baseline Vitals and Sample History Company Drill Instructor Guide Session Reference: 1 Topic: Baseline Vitals and Sample History Company Drill Level of Instruction: 2 Time Required: Three Hours Materials Blood Pressure cuff & stethoscope Pen light Clock or wrist watch with second hand Writing paper Writing pencil Personal protective equipment: gloves References Brady Emergency Care, 11th Edition, The Maryland Medical Protocols for Emergency Medical Services Providers, Effective July 1, 2011, Maryland Institute for Emergency Medical Services Systems Preparation Motivation The Baseline Vitals and SAMPLE History are part of the essential information necessary to obtain and document in order to give a patient the best possible care in the field. This information can alert the provider to call for additional resources if necessary and can give those accepting care of the patient at the next level of patient care a good idea of what may be going on inside the patient’s body. Objective (SPO) 1-1: Given a live victim; blood pressure cuff; stethoscope; pencil; paper; pen light; clock or wrist watch, the student will be able to demonstrate, from memory and without assistance, the proper procedures in obtaining a set of Baseline Vitals, to include: pulse, respirations, skin color, skin temperature and condition, pupil appearance, blood pressure and be able to document the same at a practical station, as governed by The Maryland Medical Protocols for Emergency Medical Services Providers, Effective January 1, 2002 and the Brady Emergency Care, 7th Edition, EMT-Basic National Standard Curriculum. The student will also be able to score a 70% or above on a written exam. -

ABCDE Approach
The ABCDE and SAMPLE History Approach Basic Emergency Care Course Objectives • List the hazards that must be considered when approaching an ill or injured person • List the elements to approaching an ill or injured person safely • List the components of the systematic ABCDE approach to emergency patients • Assess an airway • Explain when to use airway devices • Explain when advanced airway management is needed • Assess breathing • Explain when to assist breathing • Assess fluid status (circulation) • Provide appropriate fluid resuscitation • Describe the critical ABCDE actions • List the elements of a SAMPLE history • Perform a relevant SAMPLE history. Essential skills • Assessing ABCDE • Needle-decompression for tension • Cervical spine immobilization pneumothorax • • Full spine immobilization Three-sided dressing for chest wound • • Head-tilt and chin-life/jaw thrust Intravenous (IV) line placement • • Airway suctioning IV fluid resuscitation • • Management of choking Direct pressure/ deep wound packing for haemorrhage control • Recovery position • Tourniquet for haemorrhage control • Nasopharyngeal (NPA) and oropharyngeal • airway (OPA) placement Pelvic binding • • Bag-valve-mask ventilation Wound management • • Skin pinch test Fracture immobilization • • AVPU (alert, voice, pain, unresponsive) Snake bite management assessment • Glucose administration Why the ABCDE approach? • Approach every patient in a systematic way • Recognize life-threatening conditions early • DO most critical interventions first - fix problems before moving on -

Clinical Handbook Health Care for Children Subjected to Violence Or Sexual Abuse
KINGDOM OF CAMBODIA NATION RELIGION KING MINISTRY OF HEALTH CLINICAL HANDBOOK HEALTH CARE FOR CHILDREN SUBJECTED TO VIOLENCE OR SEXUAL ABUSE 2017 PREFACE Violence against children is a serious public health concern and a human rights violation with consequences that impact their lives in various ways. Violence and sexual abuse suffered in childhood adversely affects the body as well as the mind, which can lead to a broad range of behavioral, psychological and physical problems that persist into adulthood. Healthcare practitioners play a significantly important role in prevention and response to violence against children. They are often the first or only point of reference for children who have experienced violence, detecting abuse and providing immediate and longer-term care and support to children and families. In 2015, the Ministry of Health developed “the National Guidelines for Management of Violence Against Women and Children in the Health Sector”, which provides health care centers and referral hospitals with an overview of prevention and response in the health sector to violence against women and children. This “Clinical Handbook on Health Care for Children Subjected to Violence or Sexual Abuse” elaborates on knowledge and skills required to implement the National Guidelines. It aims to serve as a guide to ensure a prompt and adequate response to child victims of violence or sexual abuse for all healthcare practitioners. It provides further guidance on first line support, medical treatment, psychosocial support, and referral to key social and legal protection services. It can be also used as a resource manual for capacity development and training. Phnom Penh, 30th January 2017 Prof. -

New Patient Medical History Form
NEW PATIENT MEDICAL HISTORY FORM Full Name: Date: Birth Date: Age: ALLERGIES o NO ALLERGIES ALLERGY ALLERGIC REACTION MEDICATIONS MEDICATIONS DOSE TIMES PER DAY (Please list ALL) (Mg., pill, etc.) If you need more room to list medications, please write them on a blank sheet of paper with the required information HEALTH MAINTENANCE SCREENING TEST HISTORY CHolesterol Date: Facility/Provider: Abnormal Result? Y N Colonoscopy/SIGMOID Date: Facility/Provider: Abnormal Result? Y N Mammogram Date: Facility/Provider: Abnormal Result? Y N PAP SMEAR Date: Facility/Provider: Abnormal Result? Y N BONE density Date: Facility/Provider: Abnormal Result? Y N VACCINATION HISTORY Last Tetanus Booster or TdaP: Last Pnuemovax (Pneumonia): Last Flu Vaccine: Last Prevnar: Last Zoster Vaccine (Shingles): PERSONAL MEDICAL HISTORY DISEASE/CONDITION CURRENT PAST COMMENTS Alcoholism/Drug Abuse Asthma Cancer (type:_________________________________) Depression/Anxiety/Bipolar/Suicidal Diabetes (type:_______________________________) Emphysema (COPD) Heart Disease High Blood Pressure (hypertension) High Cholesterol Hypothyroidism/Thyroid Disease Renal (kidney) Disease Migraine Headaches Stroke Other: Other: SURGERIES TYPE (specify left/right) Date Location/Facility WOMEN’S HEALTH HISTORY Date of Last Menstrual Cycle: Age of First Menstruation: _____ Age of Menopause: _____ Total Number of Pregnancies: Number of Live Births: Pregnancy Complications: Patient Name: DOB: family MEDICAL HISTORY o NO Significant Family History IS KNOWN 4 CHECK ALL THat apply Stroke Cancer -

Advanced Interpretation of Adult Vital Signs in Trauma William D
Advanced Interpretation of Adult Vital Signs in Trauma William D. Hampton, DO Emergency Physician 26 March 2015 Learning Objectives 1. Better understand vital signs for what they can tell you (and what they can’t) in the assessment of a trauma patient. 2. Appreciate best practices in obtaining accurate vital signs in trauma patients. 3. Learn what teaching about vital signs is evidence-based and what is not. 4. Explain the importance of vital signs to more accurately triage, diagnose, and confidently disposition our trauma patients. 5. Apply the monitoring (and manipulation of) vital signs to better resuscitate trauma patients. Disclosure Statement • Faculty/Presenters/Authors/Content Reviewers/Planners disclose no conflict of interest relative to this educational activity. Successful Completion • To successfully complete this course, participants must attend the entire event and complete/submit the evaluation at the end of the session. • Society of Trauma Nurses is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission on Accreditation. Vital Signs Vital Signs Philosophy: “View vital signs as compensatory to the illness/complaint as opposed to primary.” Crowe, Donald MD. “Vital Sign Rant.” EMRAP: Emergency Medicine Reviews and Perspectives. February, 2010. Vital Signs Truth over Accuracy: • Document the true status of the patient: sick or not? • Complete vital signs on every patient, every time, regardless of the chief complaint. • If vital signs seem misleading or inaccurate, repeat them! • Beware sending a patient home with abnormal vitals (especially tachycardia)! •Treat vital signs the same as any other diagnostics— review them carefully prior to disposition. The Mother’s Vital Sign: Temperature Case #1 - 76-y/o homeless ♂ CC: 76-y/o homeless ♂ brought to the ED by police for eval. -

Cardiovascular Assessment
Cardiovascular Assessment A Home study Course Offered by Nurses Research Publications P.O. Box 480 Hayward CA 94543-0480 Office: 510-888-9070 Fax: 510-537-3434 No unauthorized duplication photocopying of this course is permitted Editor: Nurses Research 1 HOW TO USE THIS COURSE Thank you for choosing Nurses Research Publication home study for your continuing education. This course may be completed as rapidly as you desire. However there is a one-year maximum time limit. If you have downloaded this course from our website you will need to log back on to pay and complete your test. After you submit your test for grading you will be asked to complete a course evaluation and then your certificate of completion will appear on your screen for you to print and keep for your records. Satisfactory completion of the examination requires a passing score of at least 70%. No part of this course may be copied or circulated under copyright law. Instructions: 1. Read the course objectives. 2. Read and study the course. 3. Log back onto our website to pay and take the test. If you have already paid for the course you will be asked to login using the username and password you selected when you registered for the course. 4. When you are satisfied that the answers are correct click grade test. 5. Complete the evaluation. 6. Print your certificate of completion. If you have a procedural question or “nursing” question regarding the materials, call (510) 888-9070 for assistance. Only instructors or our director may answer a nursing question about the test. -

(June 2000) I. INTRODUCTION WHAT IS DOCUMENTATION and WHY
DRAFT EVALUATION & MANAGEMENT DOCUMENTATION GUIDELINES (June 2000) I. INTRODUCTION WHAT IS DOCUMENTATION AND WHY IS IT IMPORTANT? Medical record documentation is required to record pertinent facts, findings, and observations about an individual's health history including past and present illnesses, examinations, tests, treatments, and outcomes. The medical record chronologically documents the care of the patient and is an important element contributing to high quality care. The medical record facilitates: · the ability of the physician and other health care professionals to evaluate and plan the patient's immediate treatment, and to monitor his/her health care over time. · communication and continuity of care among physicians and other health care professionals involved in the patient's care; · accurate and timely claims review and payment; · appropriate utilization review and quality of care evaluations; and · collection of data that may be useful for research and education. An appropriately documented medical record can reduce many of the "hassles" associated with claims processing and may serve as a legal document to verify the care provided, if necessary. WHAT DO PAYERS WANT AND WHY? Because payers have a contractual obligation to enrollees, they may require reasonable documentation that services are consistent with the insurance coverage provided. They may request information to validate: · the site of service; · the medical necessity and appropriateness of the diagnostic and/or therapeutic services provided; and/or · that services provided have been accurately reported. II. GENERAL PRINCIPLES OF MEDICAL RECORD DOCUMENTATION The principles of documentation listed below are applicable to all types of medical and surgical Pg. 1 services in all settings. For Evaluation and Management (E/M) services, the nature and amount of physician work and documentation varies by type of service, place of service and the patient's status. -

Wilderness First Aid Reference Cards
Pulse/Pressure Points Wilderness First Aid Reference Cards Carotid Brachial Prepared by: Andrea Andraschko, W-EMT Radial October 2006 Femoral Posterior Dorsalis Tibial Pedis Abdominal Quadrants Airway Anatomy (Looking at Patient) RIGHT UPPER: LEFT UPPER: ANTERIOR: ANTERIOR: GALL BLADDER STOMACH LIVER SPLEEN POSTERIOR: POSTERIOR: R. KIDNEY PANCREAS L. KIDNEY RIGHT LOWER: ANTERIOR: APPENDIX CENTRAL AORTA BLADDER Tenderness in a quadrant suggests potential injury to the organ indicated in the chart. Patient Assessment System SOAP Note Information (Focused Exam) Scene Size-up BLS Pt. Information Physical (head to toe) exam: DCAP-BTLS, MOI Respiratory MOI OPQRST • Major trauma • Air in and out Environmental conditions • Environmental • Adequate Position pt. found Normal Vitals • Medical Nervous Initial Px: ABCs, AVPU Pulse: 60-90 Safety/Danger • AVPU Initial Tx Respiration: 12-20, easy Skin: Pink, warm, dry • Move/rescue patient • Protect spine/C-collar SAMPLE LOC: alert and oriented • Body substance isolation Circulatory Symptoms • Remove from heat/cold exposure • Pulse Allergies Possible Px: Trauma, Environmental, Medical • Consider safety of rescuers • Check for and Stop Severe Bleeding Current Px Medications Resources Anticipated Px → Past/pertinent Hx • # Patients STOP THINK: Field Tx ast oral intake • # Trained rescuers A – Continue with detailed exam L S/Sx to monitor VPU EVAC NOW Event leading to incident • Available equipment (incl. Pt’s) – Evac level Patient Level of Consciousness (LOC) Shock Assessment Reliable Pt: AVPU Hypovolemic – Low fluid (Tank) Calm A+ Awake and Cooperative Cardiogenic – heart problem (Pump) Comment: Cooperative A- Awake and lethargic or combative Vascular – vessel problem (Hose) If a pulse drops but does not return Sober V+ Responds with sound to verbal to ‘normal’ (60-90 bpm) within 5-25 Alert stimuli Volume Shock (VS) early/compensated minutes, an elevated pulse is likely caused by VS and not ASR. -

Patient/ Family History
Patient/ Family Mankato History Location: Mankato Fairmont New Prague Springfield St. James Waseca PATIENT PROVIDED INFORMATION The information you provide us will greatly help us to provide the highest quality and comprehensive care for you. Date Gender Male Female Date of birth (Month/Day/Year) A. PAST MEDICAL HISTORY 1. Have you ever traveled or lived outside of the United States or Canada? Do not know No Yes 2. Have you ever received a blood transfusion? Do not know No Yes (If yes, check all that apply.) Before 1980 1980-1990 After 1990 3. Have you received the following immunizations and/or had the disease? Pneumococcal (For pneumonia) Do not know No Yes Mumps Do not know No Yes Hepatitis B Do not know No Yes Rubella Do not know No Yes Hepatitis A Do not know No Yes Polio Do not know No Yes Measles Do not know No Yes Varicella (For chicken pox) Do not know No Yes 4. Indicate whether you have ever had a medical problem or surgery related to each of the following. Check all that apply. Medical Problem Surgery/Year Medical Problem Surgery/Year Eyes Lungs Ears Esophagus (Food or swallowing pipe) Nose Stomach (Ulcer) Sinuses Bowel (Small or large intestine, rectum) Tonsils Appendix Thyroid or parathyroid gland Lymph nodes Heart problems: Spleen Heart attack Liver Heart valves Gallbladder Abnormal heart rhythm Pancreas Narrowed coronary arteries Hernia Other Kidneys Arteries (Head, arms, legs, aorta, etc.) Bladder Veins or blood clots in the veins Bones ©2014 Mayo Foundation for Medical Education and Research Page 1 of 4 1081MR rev10/14 (Label) Patient Name DOB Unit No. -

Medical Staff Medical Record Policy
Number: MS -012 Effective Date: September 26, 2016 BO Revised:11/28/2016; 11/27/2017; 1/22/2018; 8/27/2018 CaroMont Regional Medical Center Author: Approved: Patrick Russo, MD, Chief-of-Staff Authorized: Todd Davis, MD, EVP, GMO MEDICAL STAFF MEDICAL RECORD POLICY 1. REQUIRED COMPONENTS OF THE MEDICAL RECORD The medical record shall include information to support the patient's diagnosis and condition, justify the patient's care, treatment and services, and document the course and result of the patient's care, and services to promote continuity of care among providers. The components may consist of the following: identification data, history and physical examination, consultations, clinical laboratory findings, radiology reports, procedure and anesthesia consents, medical or surgical treatment, operative report, pathological findings, progress notes, final diagnoses, condition on discharge, autopsy report when performed, other pertinent information and discharge summary. 2. ADMISSION HISTORY AND PHYSICAL EXAMINATION FOR HOSPITAL CARE Please refer to CaroMont Regional Medical Center Medical Staff Bylaws, Section 12.E. A. The history and physical examination (H&P), when required, shall be performed and recorded by a physician, dentist, podiatrist, or privileged practitioner who has an active NC license and has been granted privileges by the hospital. The H&P is the responsibility of the attending physician or designee. Oral surgeons, dentists, and podiatrists are responsible for the history and physical examination pertinent to their area of specialty. B. If a physician has delegated the responsibility of completing or updating an H&P to a privileged practitioner who has been granted privileges to do H&Ps, the H&P and/or update must be countersigned by the supervisor physician within 30 days after discharge to complete the medi_cal record. -

Patient Assessment?
EMERGENCY MEDICAL TECHNICIAN ‐ BASIC What is Patient Assessment? Why is Patient Assessment important? MECTA EMS Learning Assistant 2 What are the phases of patient assessment? Review of Dispatch Information Scene Survey Initial Assessment Focused History and Physical Exam Detailed Physical Exam Ongoing Assessment Communication Documentation MECTA EMS Learning Assistant 3 Why is the order of Patient Assessment important? Why is it necessary to develop a method of assessment and use that method on all patients? MECTA EMS Learning Assistant 4 SCENE SIZE‐UP INITIAL ASSESSMENT Trauma FOCUSED HISTORY & FOCUSED HISTORY & PHYSICAL EXAM PHYSICAL EXAM Patient Patient DETAILED DETAILED PHYSICAL EXAM PHYSICAL EXAM Medical ON‐GOING ASSESSMENT MECTA EMS Learning Assistant 5 Begin with receipt of call Location Incident Injured/Injuries MECTA EMS Learning Assistant 6 Continue En Route Further info from dispatcher Observe ▪ Smoke? ▪ Fire? ▪ High line wires? ▪ Railroads? ▪ Water? ▪ Industry? ▪ Other Public Safety units? MECTA EMS Learning Assistant 7 Upon Arrival Observe ▪ Overall scene ▪ Location of victim(s) ▪ Possible Mechanisms of Injury MECTA EMS Learning Assistant 8 Upon Arrival Observe ▪ Hazards ▪ Crowds ▪ HazMat ▪ Electricity ▪ Gas ▪ Fire ▪ Glass ▪ Jagged metal ▪ Stability of environment ▪ Traffic ▪ Environment MECTA EMS Learning Assistant 9 Ensure Safety ▪ Yourself ▪ Partner ▪ Other rescuers/Bystanders ▪ Patient MECTA EMS Learning Assistant 10 Call for assistance ▪ Other EMS Units ▪ Law Enforcement ▪ Fire Department ▪ -
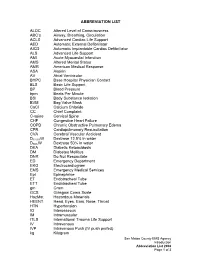
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt.