Governing Body Papers 170118
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Preston Bus Station
th July 2020 from 19 43 Preston Bus Station 43 Preston Railway Station Royal Cottom, Ancient Oak ane 44 yles L Preston Ho Hospital Cottom, Hoyles Lane e 44 Lan 43 Merrytrees Fulwood Wychnor Royal Preston Hospital mWay 44 Cotta Bampton Drive Terminus 44 Creswell Avenue L ea R oa W d oodp Plungingt l umpt o Tulk eth on R n R 44 Mill d Lane d d Preston Bus Station Ends pool R 43 Black Ingol, Cresswell Avenue Blackpool Road Cottom, Bampton Drive .co.ukLarches www.prestonbus Avenue 44 Ingol, Cresswell Avenue PrestonBusLtd Social icon Circle Only use blue and/or white. For more details check out our Preston Bus Station Brand Guidelines. @PrestonBus Preston 43 Bus Contact us: Station Preston Bus Ltd 221 Deepdale Road Preston PR1 6NY [email protected] Rotala Preston - Royal Preston Hospital 43 via Cottam Monday to Friday Ref.No.: 21P Commencing Date: 20/07/2020 Service No 43 43 43 43 43 43 43 43 43 43 43 43 Preston Bus Stn 0545 0615 0645 0715 0745 0815 0845 0915 0945 1015 1045 1115 Preston Railway Station 0550 0620 0650 0720 0750 0820 0850 0920 0950 1020 1050 1120 Cottam Ancient Oak 0600 0630 0700 0730 0800 0830 0900 0930 1000 1030 1100 1130 Cottam Hoyles Ln 0608 0638 0708 0738 0808 0838 0908 0938 1008 1038 1108 1138 Fulwood Wychnor 0613 0643 0713 0743 0813 0843 0913 0943 1013 1043 1113 1143 Royal Preston Hospital 0623 0653 0723 0753 0823 0853 0923 0953 1023 1053 1123 1153 RotalaRotala Service No 43 43 43 43 43 43 43 43 43 43 43 43 Preston Bus Stn 1145 1215 1245 1315 1345 1415 1445 1515 1545 1615 1645 1720 Preston Railway Station 1150 -

Appendix 5 Fylde
FYLDE DISTRICT - APPENDIX 5 SUBSIDISED LOCAL BUS SERVICE EVENING AND SUNDAY JOURNEYS PROPOSED TO BE WITHDRAWN FROM 18 MAY 2014 LANCASTER - GARSTANG - POULTON - BLACKPOOL 42 via Galgate - Great Eccleston MONDAY TO SATURDAY Service Number 42 42 42 $ $ $ LANCASTER Bus Station 1900 2015 2130 SCOTFORTH Boot and Shoe 1909 2024 2139 LANCASTER University Gates 1912 2027 2142 GALGATE Crossroads 1915 2030 2145 CABUS Hamilton Arms 1921 2036 2151 GARSTANG Bridge Street 1926 2041 2156 CHURCHTOWN Horns Inn 1935 2050 2205 ST MICHAELS Grapes Hotel 1939 2054 2209 GREAT ECCLESTON Square 1943 2058 2213 POULTON St Chads Church 1953 2108 2223 BLACKPOOL Layton Square 1958 2113 2228 BLACKPOOL Abingdon Street 2010 2125 2240 $ - Operated on behalf of Lancashire County Council BLACKPOOL - POULTON - GARSTANG - LANCASTER 42 via Great Eccleston - Galgate MONDAY TO SATURDAY Service Number 42 42 42 $ $ $ BLACKPOOL Abingdon Street 2015 2130 2245 BLACKPOOL Layton Square 2020 2135 2250 POULTON Teanlowe Centre 2032 2147 2302 GREAT ECCLESTON Square 2042 2157 2312 ST MICHAELS Grapes Hotel 2047 2202 2317 CHURCHTOWN Horns Inn 2051 2206 2321 GARSTANG Park Hill Road 2059 2214 2329 CABUS Hamilton Arms 2106 2221 2336 GALGATE Crossroads 2112 2227 2342 LANCASTER University Gates 2115 2230 2345 SCOTFORTH Boot and Shoe 2118 2233 2348 LANCASTER Bus Station 2127 2242 2357 $ - Operated on behalf of Lancashire County Council LIST OF ALTERNATIVE TRANSPORT SERVICES AVAILABLE – Stagecoach in Lancaster Service 2 between Lancaster and University Stagecoach in Lancaster Service 40 between Lancaster and Garstang (limited) Blackpool Transport Service 2 between Poulton and Blackpool FYLDE DISTRICT - APPENDIX 5 SUBSIDISED LOCAL BUS SERVICE EVENING AND SUNDAY JOURNEYS PROPOSED TO BE WITHDRAWN FROM 18 MAY 2014 PRESTON - LYTHAM - ST. -

Bus Travel to Myerscough College 2017/2018 Academic Year
Timetable Septemberservice 2017 80update: amended Bus Travel to Myerscough College 2017/2018 academic year Daily direct services from: • Clitheroe • Whalley • Longridge • Goosnargh • Burnley • Accrington • Blackburn • Samlesbury • Broughton • Fleetwood • Cleveleys • Blackpool • Poulton • St Annes • Lytham • Warton • Freckleton • Kirkham • Preston • Fulwood • Broughton • Ingol • Inskip • Elswick • Great Eccleston Connections from: • Lancaster & Morecambe • Fylde Coast • South Ribble & South Preston • Bolton • Horwich • Chorley • Bamber Bridge SERVICES AVAILABLE TO ALL • Including NoWcard Holders • board and alight at any recognised bus stops along routes Contact Details Finance Office Myerscough College Bilsborrow Preston PR3 ORY 01995 642218 [email protected] www.myerscough.ac.uk Preston Bus 221 Deepdale Road Preston PR1 6NY 01772 253671 [email protected] www.prestonbus.co.uk Facebook “f” Logo CMYK@PrestonBus / .eps Facebook “f” Logo CMYK / .eps PrestonBusLtd Transdev (Lancashire United) FREEPOST LUL (no stamp required) 0845 2 72 72 72 [email protected] www.lancashirebus.co.uk Services Clitheroe, Whalley, Longridge, Goosnargh to Myerscough Preston Bus service 995 Burnley, Accrington, Blackburn, Samlesbury, Broughton to Myerscough Transdev 852 Lancaster & Morecambe – Stagecoach service 40/41 alight at Barton Grange Garden Centre or Roebuck, catch Free Shuttle Bus service* 401 to Myerscough. Bolton, Horwich, Chorley, Clayton-le-Woods, Bamber Bridge, Longridge – scheme passes valid for use on any South Ribble -
Save Preston Bus Station Banner
6DYH3UHVWRQ%XV6WDWLRQ EDQQHU 7KLVEDQQHUZDVGHVLJQHGDQG PDGHE\EDQQHUPDNHU(G+DOO +HFRQWDFWHGWKH6DYH3UHVWRQ%XV 6WDWLRQJURXSDQGRIIHUHGWRPDNHD EDQQHUWRKHOSWKHFDXVHWRVDYHWKH EXLOGLQJIURPGHPROLWLRQ ,WZDVFDUULHGLQDSDUDGHRQ 6DWXUGD\1RYHPEHUZKLFK EHFDPHDFHOHEUDWLRQRIWKHEXLOGLQJ EHLQJJUDQWHG*UDGH,,OLVWHGVWDWXV )RUPDQ\RIWKHVXSSRUWHUVLWZDV WKHÀUVWWLPHWKH\KDGPHWDVPXFK RIWKHFDPSDLJQKDGEHHQFDUULHG RXWRQVRFLDOPHGLD 2QORDQIURP,Q&HUWDLQ3ODFHV %XV6WDWLRQ&RQQHFWLRQV 7KHVHFDVHVFRQWDLQLWHPVEURXJKW LQE\SHRSOHZKRUHVSRQGHGWRD FDOORXWIRUREMHFWVWKDWFRQQHFWWKHP WR3UHVWRQ%XV6WDWLRQ 7KH\RIIHUDJOLPSVHLQWRZKDWWKH EXLOGLQJKDVPHDQWWRWKHSHRSOHRI 3UHVWRQDQGIXUWKHUDÀHOGRYHUWKH ODVW\HDUV 6DUDK:DONHU 7KLVSKRWRJUDSKZDVWDNHQE\ 6DUDKҋVGDXJKWHU(PPDLQ 6KHLVQRZVWXG\LQJDUFKLWHFWXUDO GHVLJQDW/LYHUSRRO8QLYHUVLW\ 1RUPDQ3D\QH 1RUPDQ3D\QHXVHGWKLV1DWLRQDO ([SUHVVGLVFRXQWFDUGLQWKHV ZKHQKHZDVDVWXGHQWDW8&/DQ DQGWUDYHOOHGIURP3UHVWRQ%XV 6WDWLRQWR6RXWKDPSWRQ +HOHQ/LQGVD\ 7KLVFROOHFWLRQRILWHPVUHÁHFWV +HOHQҋVORQJLQWHUHVWLQ3UHVWRQ%XV 6WDWLRQ7KHFRQFUHWHIUDJPHQWDQG &KULVWPDVFDUGZHUHIURP FROOHDJXHVDW/DQFDVKLUH3RVW6KH DOVRKDVDSDUWLQWKHÀOP &KDUOHV4XLFN 7KHSRVWFDUGZDVDSUHVHQW,WLV DOZD\VNHSWLQWKHEDFNRIKLV QRWHERRNDQGLVFDUULHGDWDOOWLPHV DVUHIHUHQFH 0U/HDYHU :DVDNHHQEXVVSRWWHU7KLV EXVVSRWWLQJPDQXDOGDWHVIURPWKH VDQGPDQ\RIWKHEXVHVLQLW XVHG3UHVWRQ%XV6WDWLRQ 5LWD:KLWORFN 7KLVPXJDQGFRDVWHUXVHGWREH VROGLQ3UHVWRQ7RXULVW,QIRUPDWLRQ &HQWUHZKHUH5LWDZDV0DQDJHU 6KHSXUFKDVHGWKHPDVVKHORYHV %UXWDOLVWDUFKLWHFWXUH &KULV/RQHUJDQ &KULVLVD6HQLRU(QJLQHHUDW$583 LQ0DQFKHVWHU$OORIWKHVWDIILQWKH RIÀFHKDYHDFXEHZLWKWKHLUSLFWXUH RQ,WDOVRLQFOXGHVVRPHWKLQJ -

PRESTON - FULWOOD - WOODPLUMPTON - BROUGHTON 15 Via Wychnor - Royal Preston Hospital - ASDA - Longsands MONDAY to FRIDAY
TENDERED BUS SERVICE REVISIONS Page 1 of 6 COMMENCING 4 NOVEMBER 2019 PRESTON - FULWOOD - WOODPLUMPTON - BROUGHTON 15 via Wychnor - Royal Preston Hospital - ASDA - Longsands MONDAY TO FRIDAY Service Number 15 15 15 15 15 15 15 15 15 15 15 15 15 $ $ $ $ $ $ $ $ $ $ $ $ $ PRESTON Bus Station 0615 0715 0815 0920 1025 1125 1225 1325 1425 1525 1635 1740 1840 PRESTON Deepdale Road Depot 0621 0721 0822 0926 1031 1131 1231 1331 1431 1531 1643 1748 1846 LONGSANDS Longsands Lane 0630 0730 0831 0935 1040 1140 1240 1340 1440 1540 1654 1759 1855 FULWOOD ASDA Store 0635 0735 0836 0940 1045 1145 1245 1345 1445 1545 1659 1804 1900 FULWOOD Royal Preston Hospital 0643 0743 0845 0948 1053 1153 1253 1353 1453 1554 1708 1813 1908 FULWOOD Wychnor 0651 0751 0854 0956 1101 1201 1301 1401 1501 1603 1717 1821 1916 WOODPLUMPTON Whittle Green 0657 0757 0901 1002 1107 1207 1307 1407 1507 1609 1723 1827 1922 BROUGHTON Sunningdale ----- ----- 0905 1005 1110 1210 1310 1410 1510 1614 ----- ----- ----- $ - Operated on behalf of Lancashire County Council BROUGHTON - WOODPLUMPTON - FULWOOD - PRESTON 15 via Longsands - ASDA - Royal Preston Hospital - Wychnor MONDAY TO FRIDAY Service Number 15 15 15 15 15 15 15 15 15 15 15 15 15 $ $ $ $ $ $ $ $ $ $ $ $ $ BROUGHTON Sunningdale ----- ----- ----- 0906 1006 1111 1211 1311 1411 1511 1615 ----- ----- WOODPLUMPTON Whittle Green ----- 0659 0759 0909 1009 1114 1214 1314 1414 1514 1618 1724 1828 FULWOOD Wychnor ----- 0707 0808 0917 1017 1122 1222 1322 1422 1522 1627 1732 1835 FULWOOD Royal Preston Hospital ----- 0715 0818 0925 1025 -

S Lancs Booklet Web September 17.Pdf
ContentsContteents Page TicketsTickkeeetsts andand FaresFa 04 - 05 ServiceSerrvviccee Timetables Timetab 1 1A 06 - 16 2 2A 18 - 29 3 30 - 33 4 4C 34 - 39 8A 40 9 41 - 42 59 43 - 46 61 48 - 57 68 67 - 72 109 109A 73 - 82 111 83 - 90 113 91 - 94 125 95 - 108 721 109 X2 110 - 119 X8 120 Maps LancashireLancashire Inter-UrbanInter-Urban map 60 PrestonPreston maps 61 - 63 ChorleChorleyeyy maps 64 - 66 , We now accept contactless payments £28.00 Preston - Ribbleton - Grimsargh - Longridge 1 Mondays to Fridays, excluding Bank Holidays Codes: NSch Sch Service: 1 1 1 1 1 1 1 1 1 1 1 1 1 S1 1 1 1 1 Preston, Bus Station 0500 0523 0553 0610 0625 0635 0645 0655 0706 0716 0726 0736 0746 0746 0756 0806 0816 0826 Ribbleton, Sion Close 0514 0541 0604 0621 0638 0648 0702 0712 0723 0733 0743 0753 0803 0803 0813 0823 0829 0839 Bluebell Way, James Hall 0518 0545 0608 0625 0642 0652 0706 0716 0727 0737 0747 … … … … … … … Grimsargh, Plough Inn 0523 0550 0613 0630 0647 0657 0711 0721 0732 0742 0752 0801 0811 0811 0821 0831 0837 0847 Longridge. Kestor Lane 0530 0557 0620 0637 0654 0704 0719 0729 0740 0750 0800 0809 0819 … 0829 0839 0845 0855 Longridge, St Cecilias RCHS … … … … … … … … … … … … … 0820 … … … … 6 Longridge, opp. Post Office 0533 0600 0623 0640 0657 0707 0722 0732 0743 0753 0803 0812 0822 0825 0832 0842 0848 0858 Service: 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 Preston, Bus Station 0836 0846 0856 0906 0916 0926 0936 0946 56 06 16 26 36 46 1356 1406 Ribbleton, Sion Close 0849 0859 0909 0919 0929 0939 0949 0959 then 19 29 39 49 59 1419 at 09 1409 until Grimsargh, Plough Inn 0857 0907 0915 0925 0935 0945 0955 1005 these 15 25 35 45 55 05 1415 1425 Longridge. -

Royal Holloway University of London Aspiring Schools List for 2020 Admissions Cycle
Royal Holloway University of London aspiring schools list for 2020 admissions cycle Accrington and Rossendale College Addey and Stanhope School Alde Valley School Alder Grange School Aldercar High School Alec Reed Academy All Saints Academy Dunstable All Saints' Academy, Cheltenham All Saints Church of England Academy Alsop High School Technology & Applied Learning Specialist College Altrincham College of Arts Amersham School Appleton Academy Archbishop Tenison's School Ark Evelyn Grace Academy Ark William Parker Academy Armthorpe Academy Ash Hill Academy Ashington High School Ashton Park School Askham Bryan College Aston University Engineering Academy Astor College (A Specialist College for the Arts) Attleborough Academy Norfolk Avon Valley College Avonbourne College Aylesford School - Sports College Aylward Academy Barnet and Southgate College Barr's Hill School and Community College Baxter College Beechwood School Belfairs Academy Belle Vue Girls' Academy Bellerive FCJ Catholic College Belper School and Sixth Form Centre Benfield School Berkshire College of Agriculture Birchwood Community High School Bishop Milner Catholic College Bishop Stopford's School Blatchington Mill School and Sixth Form College Blessed William Howard Catholic School Bloxwich Academy Blythe Bridge High School Bolton College Bolton St Catherine's Academy Bolton UTC Boston High School Bourne End Academy Bradford College Bridgnorth Endowed School Brighton Aldridge Community Academy Bristnall Hall Academy Brixham College Broadgreen International School, A Technology -
Implementing the English Baccalaureate Government Consultation Response
Implementing the English Baccalaureate Government consultation response July 2017 Contents Foreword from the Secretary of State for Education 4 Introduction 6 Definition of the English Baccalaureate 6 Summary of responses received and the government’s response 8 Summary of the government response 8 Question analysis 11 Question 1: What factors do you consider should be taken into account in making decisions about which pupils should not be entered for the EBacc? 11 Government response 11 Question 2: Is there any other information that should be made available about schools’ performance in the EBacc? 13 Government response 13 Question 3: How should this policy apply to university technical colleges (UTCs), studio schools and further education colleges teaching key stage 4 pupils? 15 Government response 16 Question 4: What challenges have schools experienced in teacher recruitment to EBacc subjects? 17 Question 5: What strategies have schools found useful in attracting and retaining staff in these subjects? 17 Question 8: What additional central strategies would schools like to see in place for recruiting and training teachers in EBacc subjects? 17 Government response to questions 4, 5 and 8 18 Question 6: What approaches do schools intend to take to manage challenges relating to the teaching of EBacc subjects? 19 Question 7: Other than teacher recruitment, what other issues will schools need to consider when planning for increasing the number of pupils taking the EBacc? 20 Government response to questions 6 and 7 20 Question 9: Do you think that any of the proposals have the potential to have an impact, positive or negative, on specific pupils, in particular those with ‘relevant protected characteristics’? (The relevant protected characteristics are disability, gender reassignment, pregnancy and maternity, race, religion or belief, sex and sexual orientation). -

Comparing Strategic Management Between the United Kingdom's And
University of Wolverhampton Sami Narkia Student ID: 1126174 UG Dissertation Student ID: 1126174 23.4.2012 UNIVERSITY OF WOLVERHAMPTON Comparing Strategic Management between the United Kingdom’s and Finland’s Ice Hockey Organizations, from the Point of View of Two Same Levelled Teams. UG Dissertation 23.4.2012 Sami Narkia (1126174) Being a Dissertation presented in part requirement for the International Business Management award at the Wolverhampton University Business School. This work or any part thereof has not previously been presented in any form to the University or to any other institutional body whether for assessment or other purposes. Save for any express acknowledgements, references and/or bibliographies cited in the work, I confirm that the intellectual content is the result of my own efforts and no other person. I acknowledge and agree that the assessor of this assignment may, for the purposes of assessing this assignment: -Reproduce this assignment and provide a copy to another academic staff member; and/or -Communicate a copy of this assignment to a plagiarism-checking service. This web-based service will retain a copy of this work for subsequent plagiarism checking, but has a legal agreement with the University that it will not share or reproduce it in any form. It is acknowledged that the author of any project work shall own the copyright. However, by submitting such copyright work for assessment, the author grants to the University a perpetual royalty-free licence to do all or any of those things referred to in section 16(i) of the Copyright Designs and Patents Act 1988 (viz. -

Post 16 Online Resources for Year 11 Pupils
Post 16 Online Resources for Year 11 Pupils January 2021 Post 16 Online Resources for Year 11 Pupils Contents Page Introduction 4 School Sixth Forms 5 Accrington St Christopher's C of E High School 5 Alder Grange School 6 Bacup and Rawtenstall Grammar School 6 Clitheroe Royal Grammar School 7 Haslingden High School and Sixth Form 8 Hutton C of E Grammar School 8 Lancaster Girls' Grammar School 9 Lancaster Royal Grammar School 9 Moor Park High School and Sixth Form 10 Morecambe Bay Academy 11 Ormskirk School 11 Our Lady's Catholic College 12 Ripley St Thomas C of E Academy 13 Further Education Colleges 14 Accrington and Rossendale College 14 Blackburn College 15 Burnley College 16 Lancaster and Morecambe College 17 Myerscough College 18 Nelson and Colne College 19 Preston's College 20 Runshaw College 21 Post 16 Online Resources for Year 11 Pupils Work Based Learning/Training Providers 22 GP Strategies Training Ltd 22 Lancaster Training Services Ltd 22 North Lancs Training Group (NLTG) 23 Runshaw College 25 Training 2000 Ltd 26 Post 16 Online Resources for Year 11 Pupils Introduction This document is designed to support schools in the careers education, information, advice and guidance (CEIAG) they deliver when working with pupils in Key Stage 4/Year 11. Information has been provided by post 16 institutions across Lancashire to show their course offer, onsite facilities, support for students and how young people can apply for a place. This is intended to help support them in the decisions they are making about their futures by showing what each institution is able to provide. -

Key Stage 4 to Key Stage 5 Transition Information for Year 11 Pupils
Key stage 4 to key stage 5 transition information for Year 11 pupils June 2020 Key stage 4 to key stage 5 transition information for Year 11 pupils Contents Page Introduction 4 School Sixth Forms 5 Accrington Academy 5 Accrington St Christopher's C of E High School 6 Alder Grange School 7 Bacup and Rawtenstall Grammar School 7 Bay Leadership Academy 8 Clitheroe Royal Grammar School 8 Haslingden High School and Sixth Form 10 Hutton C of E Grammar School 11 Lancaster Girls' Grammar School 11 Lancaster Royal Grammar School 12 Ormskirk School 13 Our Lady's Catholic College 14 Ripley St Thomas C of E Academy 15 Further Education Colleges 16 Accrington and Rossendale College 16 Blackburn College 17 Blackpool and the Fylde College 18 Blackpool Sixth Form College 19 Burnley College 20 Cardinal Newman College 21 Lancaster and Morecambe College 23 Key stage 4 to key stage 5 transition information for Year 11 pupils Myerscough College 24 Nelson and Colne College 25 Preston's College 26 Runshaw College 28 St Mary's College Blackburn 29 West Lancashire College 30 Apprenticeship Providers (Lancashire Work Based Learning Forum 32 Members) Key stage 4 to key stage 5 transition information for Year 11 pupils Introduction This document is designed to provide Year 11 pupils and their parents/carers with information about individual school sixth forms and further education colleges in Lancashire. This should help to support any decisions they are making about their futures and what each institution is able to provide. Due to the Covid-19 situation, school sixth forms and colleges are not able to offer things like open days, campus tours and taster days and this may have felt like there is less support available to help young people deciding on their next steps. -
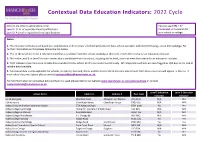
Education Indicators: 2022 Cycle
Contextual Data Education Indicators: 2022 Cycle Schools are listed in alphabetical order. You can use CTRL + F/ Level 2: GCSE or equivalent level qualifications Command + F to search for Level 3: A Level or equivalent level qualifications your school or college. Notes: 1. The education indicators are based on a combination of three years' of school performance data, where available, and combined using z-score methodology. For further information on this please follow the link below. 2. 'Yes' in the Level 2 or Level 3 column means that a candidate from this school, studying at this level, meets the criteria for an education indicator. 3. 'No' in the Level 2 or Level 3 column means that a candidate from this school, studying at this level, does not meet the criteria for an education indicator. 4. 'N/A' indicates that there is no reliable data available for this school for this particular level of study. All independent schools are also flagged as N/A due to the lack of reliable data available. 5. Contextual data is only applicable for schools in England, Scotland, Wales and Northern Ireland meaning only schools from these countries will appear in this list. If your school does not appear please contact [email protected]. For full information on contextual data and how it is used please refer to our website www.manchester.ac.uk/contextualdata or contact [email protected]. Level 2 Education Level 3 Education School Name Address 1 Address 2 Post Code Indicator Indicator 16-19 Abingdon Wootton Road Abingdon-on-Thames