Leukotriene Receptor Antagonist Therapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Leukotriene D4induced Caco2 Cell Proliferation Is Mediated By
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Diposit Digital de la Universitat de Barcelona Physiological Reports ISSN 2051-817X ORIGINAL RESEARCH Leukotriene D4-induced Caco-2 cell proliferation is mediated by prostaglandin E2 synthesis Marisol Cabral, Raquel Martın-Venegas & Juan J. Moreno Departament de Fisiologia, Facultat de Farmacia, Universitat de Barcelona, Barcelona, Spain Keywords Abstract 5-lipoxygenase, arachidonic acid cascade, cell cycle, cell growth, colon cancer. Leukotriene D4 (LTD4) is a pro-inflammatory mediator formed from arachi- donic acid through the action of 5-lipoxygenase (5-LOX). Its biological effects Correspondence are mediated by at least two G-coupled plasmatic cysteinyl LT receptors (Cys- Juan Jose Moreno, Departament de LT1-2R). It has been reported an upregulation of the 5-LOX pathway in tumor Fisiologia, Facultat de Farmacia, Universitat tissue unlike in normal colon mucosa. Colon tumors generally have an de Barcelona, Avda. Joan XXIII s/n, 08028 increased expression of CysLT1R and colon cancer patients with high expres- Barcelona, Spain. sion levels of CysLT R have poor prognosis. We previously observed that the Tel: +34 93 402 4505 1 Fax: +34 93 403 5901 cyclooxygenase pathway is involved in the control of intestinal epithelial can- E-mail: [email protected] cer cell growth through PGE2 production. The aim of this study was therefore to assess the effect of LTD4 binding with CysLT1R on Caco-2 cell growth. We Funding Information note a number of key findings from this research. We observed that at a con- This research was supported by Spanish centration similar to that found under inflammatory conditions, LTD4 was Ministry of Science and Innovation (BFU2007- able to induce Caco-2 cell proliferation and DNA synthesis. -

Cysteinyl Leukotriene Receptor 1/2 Antagonists Nonselectively Modulate Organic Anion Transport by Multidrug Resistance Proteins (MRP1-4) S
Supplemental material to this article can be found at: http://dmd.aspetjournals.org/content/suppl/2016/04/11/dmd.116.069468.DC1 1521-009X/44/6/857–866$25.00 http://dx.doi.org/10.1124/dmd.116.069468 DRUG METABOLISM AND DISPOSITION Drug Metab Dispos 44:857–866, June 2016 Copyright ª 2016 by The American Society for Pharmacology and Experimental Therapeutics Cysteinyl Leukotriene Receptor 1/2 Antagonists Nonselectively Modulate Organic Anion Transport by Multidrug Resistance Proteins (MRP1-4) s Mark A. Csandl, Gwenaëlle Conseil, and Susan P. C. Cole Departments of Biomedical and Molecular Sciences (M.A.C., S.P.C.C.), and Pathology and Molecular Medicine (G.C., S.P.C.C.), Division of Cancer Biology and Genetics, Queen’s University Cancer Research Institute, Kingston, ON, Canada Received January 13, 2016; accepted April 7, 2016 ABSTRACT Active efflux of both drugs and organic anion metabolites is class of antagonists showed any MRP selectivity. For E217bG Downloaded from mediated by the multidrug resistance proteins (MRPs). MRP1 uptake, LTM IC50s ranged from 1.2 to 26.9 mMandweremost (ABCC1), MRP2 (ABCC2), MRP3 (ABCC3), and MRP4 (ABCC4) have comparable for MRP1 and MRP4. The LTM rank order inhibitory partially overlapping substrate specificities and all transport 17b- potencies for E217bGversusLTC4 uptake by MRP1, and E217bG estradiol 17-(b-D-glucuronide) (E217bG). The cysteinyl leukotriene versus PGE2 uptake by MRP4, were also similar. Three of four receptor 1 (CysLT1R) antagonist MK-571 inhibits all four MRP CysLT1R-selective LTMs also stimulated MRP2 (but not MRP3) homologs, but little is known about the modulatory effects of newer transport and thus exerted a concentration-dependent biphasic leukotriene modifiers (LTMs). -

The 5-HT6 Receptor Antagonist SB-271046 Selectively Enhances Excitatory Neurotransmission in the Rat Frontal Cortex and Hippocampus Lee A
The 5-HT6 Receptor Antagonist SB-271046 Selectively Enhances Excitatory Neurotransmission in the Rat Frontal Cortex and Hippocampus Lee A. Dawson, Ph.D., Huy Q. Nguyen, B.S., and Ping Li, B.S. Preclinical evidence has suggested a possible role for the 5-HT6 increases in extracellular glutamate levels in both frontal receptor in the treatment of cognitive dysfunction. However, cortex and dorsal hippocampus, respectively. These effects were currently there is little neurochemical evidence suggesting the completely attenuated by infusion of tetrodotoxin but mechanism(s) which may be involved. Using the selective unaffected by the muscarinic antagonist, atropine. Here we 5-HT6 antagonist SB-271046 and in vivo microdialysis, we demonstrate for the first time the selective enhancement of have evaluated the effects of this compound on the modulation excitatory neurotransmission by SB-271046 in those brain of basal neurotransmitter release within multiple brain regions regions implicated in cognitive and memory function, and of the freely moving rat. SB-271046 produced no change in provide mechanistic evidence in support of a possible basal levels of dopamine (DA), norepinephrine (NE) or 5-HT therapeutic role for 5-HT6 receptor antagonists in the in the striatum, frontal cortex, dorsal hippocampus or nucleus treatment of cognitive and memory dysfunction. accumbens. Similarly, this compound had no effect on [Neuropsychopharmacology 25:662–668, 2001] excitatory neurotransmission in the striatum or nucleus © 2001 American College of Neuropsychopharmacology. accumbens. Conversely, SB-271046 produced 3- and 2-fold Published by Elsevier Science Inc. KEY WORDS: 5-HT6 receptor; SB-271046; Microdialysis; sma et al. 1993; Ruat et al. -

Chemical Tools for Studying Lipid-Binding Class a G Protein–Coupled Receptors
1521-0081/69/3/316–353$25.00 https://doi.org/10.1124/pr.116.013243 PHARMACOLOGICAL REVIEWS Pharmacol Rev 69:316–353, July 2017 Copyright © 2017 by The American Society for Pharmacology and Experimental Therapeutics ASSOCIATE EDITOR: STEPHEN P. H. ALEXANDER Chemical Tools for Studying Lipid-Binding Class A G Protein–Coupled Receptors Anna Cooper, Sameek Singh, Sarah Hook, Joel D. A. Tyndall, and Andrea J. Vernall School of Pharmacy, University of Otago, Dunedin, New Zealand Abstract. ....................................................................................317 I. Introduction. ..............................................................................317 A. Cannabinoid Receptor . ..................................................................317 1. Ligand Classes. ......................................................................318 B. Free Fatty Acid Receptor ................................................................320 1. Ligand Classes. ......................................................................320 C. Lysophospholipid Receptors. ............................................................321 1. Ligand Classes. ......................................................................321 D. Prostanoid Receptor . ..................................................................321 Downloaded from 1. Ligand Classes. ......................................................................322 E. Leukotriene Receptor . ..................................................................322 1. Ligand Classes. ......................................................................322 -
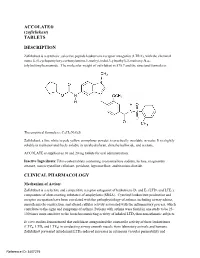
ACCOLATE® (Zafirlukast) TABLETS DESCRIPTION
ACCOLATE® (zafirlukast) TABLETS DESCRIPTION Zafirlukast is a synthetic, selective peptide leukotriene receptor antagonist (LTRA), with the chemical name 4-(5-cyclopentyloxy-carbonylamino-1-methyl-indol-3-ylmethyl)-3-methoxy-N-o tolylsulfonylbenzamide. The molecular weight of zafirlukast is 575.7 and the structural formula is: The empirical formula is: C31H33N3O6S Zafirlukast, a fine white to pale yellow amorphous powder, is practically insoluble in water. It is slightly soluble in methanol and freely soluble in tetrahydrofuran, dimethylsulfoxide, and acetone. ACCOLATE is supplied as 10 and 20 mg tablets for oral administration. Inactive Ingredients: Film-coated tablets containing croscarmellose sodium, lactose, magnesium stearate, microcrystalline cellulose, povidone, hypromellose, and titanium dioxide. CLINICAL PHARMACOLOGY Mechanism of Action: Zafirlukast is a selective and competitive receptor antagonist of leukotriene D4 and E4 (LTD4 and LTE4), components of slow-reacting substance of anaphylaxis (SRSA). Cysteinyl leukotriene production and receptor occupation have been correlated with the pathophysiology of asthma, including airway edema, smooth muscle constriction, and altered cellular activity associated with the inflammatory process, which contribute to the signs and symptoms of asthma. Patients with asthma were found in one study to be 25 100 times more sensitive to the bronchoconstricting activity of inhaled LTD4 than nonasthmatic subjects. In vitro studies demonstrated that zafirlukast antagonized the contractile activity of three leukotrienes (LTC4, LTD4 and LTE4) in conducting airway smooth muscle from laboratory animals and humans. Zafirlukast prevented intradermal LTD4-induced increases in cutaneous vascular permeability and Reference ID: 3407275 inhibited inhaled LTD4-induced influx of eosinophils into animal lungs. Inhalational challenge studies in sensitized sheep showed that zafirlukast suppressed the airway responses to antigen; this included both the early- and late-phase response and the nonspecific hyperresponsiveness. -

Receptor Antagonist (H RA) Shortages | May 25, 2020 2 2 2 GERD4,5 • Take This Opportunity to Determine If Continued Treatment Is Necessary
H2-receptor antagonist (H2RA) Shortages Background . 2 H2RA Alternatives . 2 Therapeutic Alternatives . 2 Adults . 2 GERD . 3 PUD . 3 Pediatrics . 3 GERD . 3 PUD . 4 Tables Table 1: Health Canada–Approved Indications of H2RAs . 2 Table 2: Oral Adult Doses of H2RAs and PPIs for GERD . 4 Table 3: Oral Adult Doses of H2RAs and PPIs for PUD . 5 Table 4: Oral Pediatric Doses of H2RAs and PPIs for GERD . 6 Table 5: Oral Pediatric Doses of H2RAs and PPIs for PUD . 7 References . 8 H2-receptor antagonist (H2RA) Shortages | May 25, 2020 1 H2-receptor antagonist (H2RA) Shortages BACKGROUND Health Canada recalls1 and manufacturer supply disruptions may be causing shortages of commonly used acid-reducing medications called histamine H2-receptor antagonists (H2RAs) . H2RAs include cimetidine, famotidine, nizatidine and ranitidine . 2 There are several Health Canada–approved indications of H2RAs (see Table 1); this document addresses the most common: gastroesophageal reflux disease (GERD) and peptic ulcer disease (PUD) . 2 TABLE 1: HEALTH CANADA–APPROVED INDICATIONS OF H2RAs H -Receptor Antagonists (H RAs) Health Canada–Approved Indications 2 2 Cimetidine Famotidine Nizatidine Ranitidine Duodenal ulcer, treatment ü ü ü ü Duodenal ulcer, prophylaxis — ü ü ü Benign gastric ulcer, treatment ü ü ü ü Gastric ulcer, prophylaxis — — — ü GERD, treatment ü ü ü ü GERD, maintenance of remission — ü — — Gastric hypersecretion,* treatment ü ü — ü Self-medication of acid indigestion, treatment and prophylaxis — ü† — ü† Acid aspiration syndrome, prophylaxis — — — ü Hemorrhage from stress ulceration or recurrent bleeding, — — — ü prophylaxis ü = Health Canada–approved indication; GERD = gastroesophageal reflux disease *For example, Zollinger-Ellison syndrome . -

Binding Mode Exploration of B1 Receptor Antagonists' by the Use of Molecular Dynamics and Docking Simulation—How Different T
International Journal of Molecular Sciences Article Binding Mode Exploration of B1 Receptor Antagonists’ by the Use of Molecular Dynamics and Docking Simulation—How Different Target Engagement Can Determine Different Biological Effects Marica Gemei 1,*, Carmine Talarico 1 , Laura Brandolini 1, Candida Manelfi 1, Lorena Za 2, Silvia Bovolenta 2, Chiara Liberati 2, Luigi Del Vecchio 3, Roberto Russo 4 , Carmen Cerchia 4, Marcello Allegretti 1 and Andrea Rosario Beccari 1 1 Dompé Farmaceutici SpA, via Campo di Pile, 67100 L’Aquila, Italy; [email protected] (C.T.); [email protected] (L.B.); candida.manelfi@dompe.com (C.M.); [email protected] (M.A.); [email protected] (A.R.B.) 2 Axxam, Via Meucci 3, Bresso, 20091 Milano, Italy; [email protected] (L.Z.); [email protected] (S.B.); [email protected] (C.L.) 3 Ceinge Biotecnologie Avanzate, via G. Salvatore 486, 80145 Napoli, Italy; [email protected] 4 Department of Pharmacy, University of Naples “Federico II”, via D. Montesano, 49, 80131 Napoli, Italy; [email protected] (R.R.); [email protected] (C.C.) * Correspondence: [email protected]; Tel.: +34-06-465916 Received: 26 August 2020; Accepted: 12 October 2020; Published: 16 October 2020 Abstract: The kinin B1 receptor plays a critical role in the chronic phase of pain and inflammation. The development of B1 antagonists peaked in recent years but almost all promising molecules failed in clinical trials. Little is known about these molecules’ mechanisms of action and additional information will be necessary to exploit the potential of the B1 receptor. -

Original Articles Enhancement of Leukotriene B4 Release in Stimulated Asthmatic Neutrophils by Platelet Activating Factor
1024 Thorax 1997;52:1024±1029 Thorax: first published as 10.1136/thx.52.12.1024 on 1 December 1997. Downloaded from Original articles Enhancement of leukotriene B4 release in stimulated asthmatic neutrophils by platelet activating factor Kunihiko Shindo, Kohei Koide, Motonori Fukumura Abstract of phospholipase A2 and acetyltransferase on Background ± The role of platelet ac- membrane alkylacyl phospholipids. PAF was tivating factor (PAF) in asthma remains originally described as a substance released controversial. The priming eVect of PAF from basophils sensitised with IgE.1 on leukotriene B4 (LTB4) release, 5-lip- The stimulation of neutrophils by PAF res- oxygenase activity, and intracellular cal- ults in the release of lysosomal enzymes and cium levels in asthmatic neutrophils was superoxide anions and the generation of leuko- 23 examined. triene (LT) B4. The biological eVects of Methods ±LTB4 and other lipoxygenase PAF, including airway microvascular leakage, metabolites in neutrophils obtained from bronchoconstriction, sustained increase in 17 asthmatic patients and 15 control sub- bronchial smooth muscle responsiveness, and jects were measured by reverse phase-high pulmonary vasoconstriction, mimic many clin- performance liquid chromatography (RP- ical features of asthma. Thus, PAF has been HPLC). Intracellular calcium levels were considered an important mediator in asthma monitored using the ¯uorescent probe as well as in other lung disorders.4 However, fura-2. clinical studies56 with PAF receptor antagonist Results ± The mean (SD) -

System, Method and Software for Calculation of a Cannabis Drug Efficiency Index for the Reduction of Inflammation
International Journal of Molecular Sciences Article System, Method and Software for Calculation of a Cannabis Drug Efficiency Index for the Reduction of Inflammation Nicolas Borisov 1,† , Yaroslav Ilnytskyy 2,3,†, Boseon Byeon 2,3,4,†, Olga Kovalchuk 2,3 and Igor Kovalchuk 2,3,* 1 Moscow Institute of Physics and Technology, 9 Institutsky lane, Dolgoprudny, Moscow Region 141701, Russia; [email protected] 2 Department of Biological Sciences, University of Lethbridge, Lethbridge, AB T1K 3M4, Canada; [email protected] (Y.I.); [email protected] (B.B.); [email protected] (O.K.) 3 Pathway Rx., 16 Sandstone Rd. S., Lethbridge, AB T1K 7X8, Canada 4 Biomedical and Health Informatics, Computer Science Department, State University of New York, 2 S Clinton St, Syracuse, NY 13202, USA * Correspondence: [email protected] † First three authors contributed equally to this research. Abstract: There are many varieties of Cannabis sativa that differ from each other by composition of cannabinoids, terpenes and other molecules. The medicinal properties of these cultivars are often very different, with some being more efficient than others. This report describes the development of a method and software for the analysis of the efficiency of various cannabis extracts to detect the anti-inflammatory properties of the various cannabis extracts. The method uses high-throughput gene expression profiling data but can potentially use other omics data as well. According to the signaling pathway topology, the gene expression profiles are convoluted into the signaling pathway activities using a signaling pathway impact analysis (SPIA) method. The method was tested by inducing inflammation in human 3D epithelial tissues, including intestine, oral and skin, and then exposing these tissues to various extracts and then performing transcriptome analysis. -

Montelukast, a Leukotriene Receptor Antagonist, Reduces the Concentration of Leukotrienes in the Respiratory Tract of Children with Persistent Asthma
Montelukast, a leukotriene receptor antagonist, reduces the concentration of leukotrienes in the respiratory tract of children with persistent asthma Benjamin Volovitz, MD,a,b Elvan Tabachnik, MD,c Moshe Nussinovitch, MD,b Biana Shtaif, MSc,b Hanna Blau, MD,a Irit Gil-Ad, PhD,b Abraham Weizman, MD,b and Itzhak Varsano, MDa,b Petah Tikva, Tel Aviv, and Rehovot, Israel Background: Leukotrienes are bronchoactive mediators secreted by inflammatory cells in the respiratory mucosa on Abbreviations used exposure to asthma triggers. BAL: Bronchoalveolar lavage Objective: We investigated the effect of montelukast, a CysLT1: Cysteinyl leukotriene 1 (receptor) leukotriene receptor antagonist, on the release of leukotrienes ECP: Eosinophilic cationic protein in the respiratory mucosa of children with persistent asthma. LTC4: Leukotriene C4 Method: Twenty-three children aged 6 to 11 years with moder- LTD4: Leukotriene D4 ately severe asthma were treated in a cross-over design start- LTE4: Leukotriene E4 ing, after a 2-week run in period, with either montelukast (n = 12) or cromolyn (n = 11) for 4 weeks with a 2-week washout period between treatments. Twelve of them were then treated Cysteinyl leukotrienes are potent proinflammatory with either montelukast or beclomethasone for 6 months. The mediators produced from a variety of inflammatory use of β -agonists was recorded on a diary card. The concen- 2 cells, including mast cells, eosinophils, basophils and tration of leukotriene C4 (LTC4) was measured by HPLC in nasal washes obtained before and at the end of each treatment macrophages. Leukotriene C4 (LTC4) is metabolized period. Eosinophilic cationic protein (ECP) was measured in enzymatically to leukotriene D4 (LTD4) and subsequent- the nasal washes by RIA. -

Regulation of Immune Cells by Eicosanoid Receptors
Regulation of Immune Cells by Eicosanoid Receptors The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Kim, Nancy D., and Andrew D. Luster. 2007. “Regulation of Immune Cells by Eicosanoid Receptors.” The Scientific World Journal 7 (1): 1307-1328. doi:10.1100/tsw.2007.181. http://dx.doi.org/10.1100/ tsw.2007.181. Published Version doi:10.1100/tsw.2007.181 Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:37298366 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA Review Article Special Issue: Eicosanoid Receptors and Inflammation TheScientificWorldJOURNAL (2007) 7, 1307–1328 ISSN 1537-744X; DOI 10.1100/tsw.2007.181 Regulation of Immune Cells by Eicosanoid Receptors Nancy D. Kim and Andrew D. Luster* Center for Immunology and Inflammatory Diseases, Division of Rheumatology, Allergy, and Immunology, Massachusetts General Hospital, Harvard Medical School, Boston E-mail: [email protected] Received March 13, 2007; Revised June 14, 2007; Accepted July 2, 2007; Published September 1, 2007 Eicosanoids are potent, bioactive, lipid mediators that regulate important components of the immune response, including defense against infection, ischemia, and injury, as well as instigating and perpetuating autoimmune and inflammatory conditions. Although these lipids have numerous effects on diverse cell types and organs, a greater understanding of their specific effects on key players of the immune system has been gained in recent years through the characterization of individual eicosanoid receptors, the identification and development of specific receptor agonists and inhibitors, and the generation of mice genetically deficient in various eicosanoid receptors. -

The Selective Serotonin2a Receptor Antagonist, MDL100,907, Elicits A
BRIEF REPORT The Selective Serotonin2A Receptor Antagonist, MDL100,907, Elicits a Specific Interoceptive Cue in Rats Anne Dekeyne, Ph.D., Loretta Iob, B.Sc., Patrick Hautefaye, Ph.D., and Mark J. Millan, Ph.D. Employing a two-lever, food-reinforced, Fixed Ratio 10 5-HT2B/2C antagonist, SB206,553 (0.16 and 2.5 mg/kg) and drug discrimination procedure, rats were trained to the selective 5-HT2C antagonists, SB242,084 (2.5 and recognize the highly-selective serotonin (5-HT)2A receptor 10.0 mg/kg,) and RS102221 (2.5 and 10.0 mg/kg), did not antagonist, MDL100,907 (0.16 mg/kg, i.p.). They attained significantly generalize. In conclusion, selective blockade of Ϯ Ϯ criterion after a mean S.E.M. of 70 11 sessions. 5-HT2A receptors by MDL100,907 elicits a discriminative MDL100,907 fully generalized with an Effective Dose stimulus in rats which appears to be specifically mediated (ED)50 of 0.005 mg/kg, s.c.. A further selective 5-HT2A via 5-HT2A as compared with 5-HT2B and 5-HT2C receptors. antagonist, SR46349, similarly generalized with an ED50 of [Neuropsychopharmacology 26:552–556, 2002] 0.04 mg/kg, s.c. In distinction, the selective 5-HT2B © 2002 American College of Neuropsychopharmacology antagonist, SB204,741 (0.63 and 10.0 mg/kg), the Published by Elsevier Science Inc. KEY WORDS: Drug discrimination; Interoceptive; 5-HT2A stimulus (DS) properties of several 5-HT2 agonists and receptors hallucinogens, such as mescaline (Appel and Callahan 1989), lysergic acid diethylamide (LSD) (Fiorella et al. Drug discrimination procedures have been extensively 1995) and quipazine (Friedman et al.