Guidelines for Patients® Neuroendocrine Tumors
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Adrenal Neuroblastoma Mimicking Pheochromocytoma in an Adult With
Khalayleh et al. Int Arch Endocrinol Clin Res 2017, 3:008 Volume 3 | Issue 1 International Archives of Endocrinology Clinical Research Case Report : Open Access Adrenal Neuroblastoma Mimicking Pheochromocytoma in an Adult with Neurofibromatosis Type 1 Harbi Khalayleh1, Hilla Knobler2, Vitaly Medvedovsky2, Edit Feldberg3, Judith Diment3, Lena Pinkas4, Guennadi Kouniavsky1 and Taiba Zornitzki2* 1Department of Surgery, Hebrew University Medical School of Jerusalem, Israel 2Endocrinology, Diabetes and Metabolism Institute, Kaplan Medical Center, Hebrew University Medical School of Jerusalem, Israel 3Pathology Institute, Kaplan Medical Center, Israel 4Nuclear Medicine Institute, Kaplan Medical Center, Israel *Corresponding author: Taiba Zornitzki, MD, Endocrinology, Diabetes and Metabolism Institute, Kaplan Medical Center, Hebrew University Medical School of Jerusalem, Bilu 1, 76100 Rehovot, Israel, Tel: +972-894- 41315, Fax: +972-8 944-1912, E-mail: [email protected] Context 2. This is the first reported case of an adrenal neuroblastoma occurring in an adult patient with NF1 presenting as a large Neurofibromatosis type 1 (NF1) is a genetic disorder asso- adrenal mass with increased catecholamine levels mimicking ciated with an increased risk of malignant disorders. Adrenal a pheochromocytoma. neuroblastoma is considered an extremely rare tumor in adults and was not previously described in association with NF1. 3. This case demonstrates the clinical overlap between pheo- Case description: A 42-year-old normotensive woman with chromocytoma and neuroblastoma. typical signs of NF1 underwent evaluation for abdominal pain, Keywords and a large 14 × 10 × 16 cm left adrenal mass displacing the Adrenal neuroblastoma, Neurofibromatosis type 1, Pheo- spleen, pancreas and colon was found. An initial diagnosis of chromocytoma, Neural crest-derived tumors pheochromocytoma was done based on the known strong association between pheochromocytoma, NF1 and increased catecholamine levels. -

Primary Hepatic Neuroendocrine Carcinoma: Report of Two Cases and Literature Review
The Jackson Laboratory The Mouseion at the JAXlibrary Faculty Research 2018 Faculty Research 3-1-2018 Primary hepatic neuroendocrine carcinoma: report of two cases and literature review. Zi-Ming Zhao The Jackson Laboratory, [email protected] Jin Wang Ugochukwu C Ugwuowo Liming Wang Jeffrey P Townsend Follow this and additional works at: https://mouseion.jax.org/stfb2018 Part of the Life Sciences Commons, and the Medicine and Health Sciences Commons Recommended Citation Zhao, Zi-Ming; Wang, Jin; Ugwuowo, Ugochukwu C; Wang, Liming; and Townsend, Jeffrey P, "Primary hepatic neuroendocrine carcinoma: report of two cases and literature review." (2018). Faculty Research 2018. 71. https://mouseion.jax.org/stfb2018/71 This Article is brought to you for free and open access by the Faculty Research at The ousM eion at the JAXlibrary. It has been accepted for inclusion in Faculty Research 2018 by an authorized administrator of The ousM eion at the JAXlibrary. For more information, please contact [email protected]. Zhao et al. BMC Clinical Pathology (2018) 18:3 https://doi.org/10.1186/s12907-018-0070-7 CASE REPORT Open Access Primary hepatic neuroendocrine carcinoma: report of two cases and literature review Zi-Ming Zhao1,2*† , Jin Wang3,4,5†, Ugochukwu C. Ugwuowo6, Liming Wang4,8* and Jeffrey P. Townsend2,7* Abstract Background: Primary hepatic neuroendocrine carcinoma (PHNEC) is extremely rare. The diagnosis of PHNEC remains challenging—partly due to its rarity, and partly due to its lack of unique clinical features. Available treatment options for PHNEC include surgical resection of the liver tumor(s), radiotherapy, liver transplant, transcatheter arterial chemoembolization (TACE), and administration of somatostatin analogues. -

What Is a Gastrointestinal Carcinoid Tumor?
cancer.org | 1.800.227.2345 About Gastrointestinal Carcinoid Tumors Overview and Types If you have been diagnosed with a gastrointestinal carcinoid tumor or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is a Gastrointestinal Carcinoid Tumor? Research and Statistics See the latest estimates for new cases of gastrointestinal carcinoid tumor in the US and what research is currently being done. ● Key Statistics About Gastrointestinal Carcinoid Tumors ● What’s New in Gastrointestinal Carcinoid Tumor Research? What Is a Gastrointestinal Carcinoid Tumor? Gastrointestinal carcinoid tumors are a type of cancer that forms in the lining of the gastrointestinal (GI) tract. Cancer starts when cells begin to grow out of control. To learn more about what cancer is and how it can grow and spread, see What Is Cancer?1 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 To understand gastrointestinal carcinoid tumors, it helps to know about the gastrointestinal system, as well as the neuroendocrine system. The gastrointestinal system The gastrointestinal (GI) system, also known as the digestive system, processes food for energy and rids the body of solid waste. After food is chewed and swallowed, it enters the esophagus. This tube carries food through the neck and chest to the stomach. The esophagus joins the stomachjust beneath the diaphragm (the breathing muscle under the lungs). The stomach is a sac that holds food and begins the digestive process by secreting gastric juice. The food and gastric juices are mixed into a thick fluid, which then empties into the small intestine. -
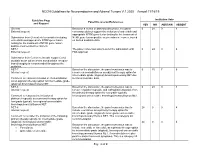
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19 Guideline Page Institution Vote Panel Discussion/References and Request YES NO ABSTAIN ABSENT General Based on a review of data and discussion, the panel 0 24 0 4 External request: consensus did not support the inclusion of entrectinib and appropriate NTRK gene fusion testing for the treatment of Submission from Genentech to consider including NTRK gene fusion-positive neuroendocrine cancer, based entrectinib and appropriate NTRK gene fusion on limited available data. testing for the treatment of NTRK gene fusion- positive neuroendocrine cancers. NET-1 The panel consensus was to defer the submission until 0 24 0 4 External request: FDA approval. Submission from Curium to include copper Cu 64 dotatate as an option where somatostatin receptor- based imaging is recommended throughout the guideline. NET-7 Based on the discussion, the panel consensus was to 0 15 7 6 Internal request: remove chemoradiation as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET due Comment to reassess inclusion of chemoradiation to limited available data. as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET. NET-8 Based on the discussion, the panel consensus was to 0 24 0 4 Internal request: remove cisplatin/etoposide and carboplatin/etoposide from the primary therapy option for low grade (typical), Comment to reassess the inclusion of locoregional unresectable bronchopulmonary/thymus NET. platinum/etoposide as a primary therapy option for low grade (typical), locoregional unresectable bronchopulmonary/thymus NET. NET-8 Based on the discussion, the panel consensus was to 24 0 0 4 Internal request: include everolimus as a primary therapy option for intermediate grade (atypical), locoregional unresectable Comment to consider the inclusion of the following bronchopulmonary/thymus NET. -

Pancreatic Insulinomas in Multiple Endocrine Neoplasia, Type I Knockout Mice Can Develop in the Absence of Chromosome Instability Or Microsatellite Instability
[CANCER RESEARCH 64, 7039–7044, October 1, 2004] Pancreatic Insulinomas in Multiple Endocrine Neoplasia, Type I Knockout Mice Can Develop in the Absence of Chromosome Instability or Microsatellite Instability Peter C. Scacheri,1 Alyssa L. Kennedy,1 Koei Chin,4 Meghan T. Miller,1 J. Graeme Hodgson,4 Joe W. Gray,4 Stephen J. Marx,2 Allen M. Spiegel,3 and Francis S. Collins1 1National Human Genome Research Institute, 2National Institute of Diabetes and Digestive and Kidney Diseases, and 3National Institute of Deafness and Communication Disorders, National Institutes of Health, Bethesda, Maryland; and 4Cancer Genetics and Breast Oncology, University of California San Francisco Comprehensive Cancer Center, San Francisco, California ABSTRACT excision repair instability. The fact that the vast majority of tumors show one of these three modes of instability, but usually not more than Multiple endocrine neoplasia, type I (MEN1) is an inherited cancer one, suggests that genetic instability may be essential for a neoplasia syndrome characterized by tumors arising primarily in endocrine tissues. to develop, although this hypothesis has been the subject of continued The responsible gene acts as a tumor suppressor, and tumors in affected heterozygous individuals occur after inactivation of the wild-type allele. debate. Previous studies have shown that Men1 knockout mice develop multiple Multiple endocrine neoplasia, type I (MEN1), is an inherited cancer pancreatic insulinomas, but this occurs many months after loss of both syndrome characterized by multiple tumors, most striking for hor- copies of the Men1 gene. These studies imply that loss of Men1 is not alone mone secretion from the parathyroid gland, pancreatic islets, and sufficient for tumor formation and that additional somatic genetic changes pituitary gland. -

An Endocrine Society Clinical Practice Guideline
SPECIAL FEATURE Clinical Practice Guideline Pheochromocytoma and Paraganglioma: An Endocrine Society Clinical Practice Guideline Jacques W. M. Lenders, Quan-Yang Duh, Graeme Eisenhofer, Anne-Paule Gimenez-Roqueplo, Stefan K. G. Grebe, Mohammad Hassan Murad, Mitsuhide Naruse, Karel Pacak, and William F. Young, Jr Radboud University Medical Center (J.W.M.L.), 6500 HB Nijmegen, The Netherlands; VA Medical Center and University of California, San Francisco (Q.-Y.D.), San Francisco, California 94121; University Hospital Dresden (G.E.), 01307 Dresden, Germany; Assistance Publique-Hôpitaux de Paris, Hôpital Européen Georges Pompidou, Service de Génétique, (A.-P.G.-R.), F-75015 Paris, France; Université Paris Descartes (A.-P.G.-R.), F-75006 Paris, France; Mayo Clinic (S.K.G.G., M.H.M.), Rochester, Minnesota 55905; National Hospital Organisation Kyoto Medical Center (M.N.), Kyoto 612-8555; Japan; Eunice Kennedy Shriver National Institute of Child Health & Human Development (K.P.), Bethesda, Maryland 20892; and Mayo Clinic (W.F.Y.), Rochester, Minnesota 55905 Objective: The aim was to formulate clinical practice guidelines for pheochromocytoma and para- ganglioma (PPGL). Participants: The Task Force included a chair selected by the Endocrine Society Clinical Guidelines Subcommittee (CGS), seven experts in the field, and a methodologist. The authors received no corporate funding or remuneration. Evidence: This evidence-based guideline was developed using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) system to describe both the strength of rec- ommendations and the quality of evidence. The Task Force reviewed primary evidence and com- missioned two additional systematic reviews. Consensus Process: One group meeting, several conference calls, and e-mail communications enabled consensus. -

Pancreatic Gangliocytic Paraganglioma Harboring Lymph
Nonaka et al. Diagnostic Pathology (2017) 12:57 DOI 10.1186/s13000-017-0648-x CASEREPORT Open Access Pancreatic gangliocytic paraganglioma harboring lymph node metastasis: a case report and literature review Keisuke Nonaka1,2, Yoko Matsuda1, Akira Okaniwa3, Atsuko Kasajima2, Hironobu Sasano2 and Tomio Arai1* Abstract Background: Gangliocytic paraganglioma (GP) is a rare neuroendocrine neoplasm, which occurs mostly in the periampullary portion of the duodenum; the majority of the reported cases of duodenal GP has been of benign nature with a low incidence of regional lymph node metastasis. GP arising from the pancreas is extremely rare. To date, only three cases have been reported and its clinical characteristics are largely unknown. Case presentation: A nodule located in the pancreatic head was incidentally detected in an asymptomatic 68-year-old woman. Computed tomography revealed 18-, 8-, and 12-mm masses in the pancreatic head, the pancreatic tail, and the left adrenal gland, respectively. Subsequent genetic examination revealed an absence of mutations in the MEN1 and VHL genes. Macroscopically, the tumor located in the pancreatic head was 22 mm in size and displayed an ill-circumscribed margin along with yellowish-white color. Microscopically, it was composed of three cell components: epithelioid cells, ganglion-like cells, and spindle cells, which led to the diagnosis of GP. The tumor was accompanied by a peripancreatic lymph node metastasis. The tumor in the pancreatic tail was histologically classified as a neuroendocrine tumor (NET) G1 (grade 1, WHO 2010), whereas the tumor in the left adrenal gland was identified as an adrenocortical adenoma. The patient was disease-free at the 12-month follow-up examination. -

Rising Incidence of Neuroendocrine Tumors
Rising Incidence of Neuroendocrine Tumors Dasari V, Yao J, et al. JAMA Oncology 2017 S L I D E 1 Overview Pancreatic Neuroendocrine Tumors • Tumors which arise from endocrine cells of the pancreas • 5.6 cases per million – 3% of pancreatic tumors • Median age at diagnosis 60 years • More indolent course compared to adenocarcinoma – 10-year overall survival 40% • Usually sporadic but can be associated with hereditary syndromes – Core genetic pathways altered in sporadic cases • DNA damage repair (MUTYH) Chromatin remodeling (MEN1) • Telomere maintenance (MEN1, DAXX, ATRX) mTOR signaling – Hereditary: 17% of patients with germline mutation Li X, Wang C, et al. Cancer Med 2018 Scarpa A, Grimond S, et al. NatureS L I2017 D E 2 Pathology Classification European American Joint World Health Organization Neuroendocrine Committee on Cancer (WHO) Tumor Society (AJCC) (ENETS) Grade Ki-67 Mitotic rt TNM TNM T1: limit to pancreas, <2 cm T1: limit to pancreas, ≦2 cm T2: limit to pancreas, 2-4 cm T2: >limit to pancreas, 2 cm T3: limit to pancreas, >4 cm, T3: beyond pancreas, no celiac or Low ≤2% <2 invades duodenum, bile duct SMA T4: beyond pancreas, invasion involvement adjacent organs or vessels T4: involves celiac or SMA N0: node negative No: node negative Intermed 3-20% 2-20 N1: node positive N1: node positive M0: no metastases M0: no metastases High >20% >20 M1: metastases M1: metastases S L I D E 3 Classification Based on Functionality • Nonfunctioning tumors – No clinical symptoms (can still produce hormone) – Accounts for 40% of tumors – 60-85% -

Pituitary Adenomas: from Diagnosis to Therapeutics
biomedicines Review Pituitary Adenomas: From Diagnosis to Therapeutics Samridhi Banskota 1 and David C. Adamson 1,2,3,* 1 School of Medicine, Emory University, Atlanta, GA 30322, USA; [email protected] 2 Department of Neurosurgery, Emory University, Atlanta, GA 30322, USA 3 Neurosurgery, Atlanta VA Healthcare System, Decatur, GA 30322, USA * Correspondence: [email protected] Abstract: Pituitary adenomas are tumors that arise in the anterior pituitary gland. They are the third most common cause of central nervous system (CNS) tumors among adults. Most adenomas are benign and exert their effect via excess hormone secretion or mass effect. Clinical presentation of pituitary adenoma varies based on their size and hormone secreted. Here, we review some of the most common types of pituitary adenomas, their clinical presentation, and current diagnostic and therapeutic strategies. Keywords: pituitary adenoma; prolactinoma; acromegaly; Cushing’s; transsphenoidal; CNS tumor 1. Introduction The pituitary gland is located at the base of the brain, coming off the inferior hy- pothalamus, and weighs no more than half a gram. The pituitary gland is often referred to as the “master gland” and is the most important endocrine gland in the body because it regulates vital hormone secretion [1]. These hormones are responsible for vital bodily Citation: Banskota, S.; Adamson, functions, such as growth, blood pressure, reproduction, and metabolism [2]. Anatomically, D.C. Pituitary Adenomas: From the pituitary gland is divided into three lobes: anterior, intermediate, and posterior. The Diagnosis to Therapeutics. anterior lobe is composed of several endocrine cells, such as lactotropes, somatotropes, and Biomedicines 2021, 9, 494. https: corticotropes, which synthesize and secrete specific hormones. -

Primary Neuroendocrine Neoplasms of the Kidney, a Distinct Entity but Classifiable- Like the Gastroenteropancreatic Neuroendocrine Neoplasms
C-60 Primary Neuroendocrine Neoplasms of the Kidney, A Distinct Entity but Classifiable- Like the Gastroenteropancreatic Neuroendocrine Neoplasms Manik Amin1; Deyali Chatterjee2 1Washington University in St Louis; 2Washington University School of Medicine BACKGROUND: Primary neuroendocrine neoplasms of the kidney are a distinct and rare entity, but classifiable-like the gastroenteropancreatic neuroendocrine neoplasms. Due to rarity of these tumors, not much is known about histopathology and behaviors of these tumors. We attempted to review pathology of primary kidney neuroendocrine tumor patients at our institution. METHODS: Retrospective chart review identified 8 primary kidney neuroendocrine tumors from Siteman Cancer Registry database from 1/1/2000 until 1/1/2018. Pathology review was done for all the patients to confirm their diagnosis and other pathological features. RESULTS: In our cohort, we identified eight cases of neuroendocrine neoplasms of the kidney. Three of the cases were poorly differentiated neuroendocrine carcinoma. All cases of well-differentiated neuroendocrine tumor (either grade 1 or grade 2) were identified in females (age range 44 – 60). All the tumors characteristically extended to the perirenal fat. These tumors showed diffuse positivity for synaptophysin, variable positivity for chromogranin, and did not stain for markers specific for renal differentiation (PAX-8). The growth pattern in well differentiated neuroendocrine tumors is predominantly trabeculated, but a diffuse plasmacytoid growth is also noted, which is unusual in gastroenteropancreatic neuroendocrine neoplasms. Two patients had Primary tumor measuring 9 cm and 14 cm respectively also presented with positive lymph nodes and lymphovascular invasion developed metastatic disease in 2 years. NANETS 2019 Symposium Abstracts | 175 CONCLUSION: Primary kidney neuroendocrine tumors are very rare. -

Solitary Duodenal Metastasis from Renal Cell Carcinoma with Metachronous Pancreatic Neuroendocrine Tumor: Review of Literature with a Case Discussion
Published online: 2021-05-24 Practitioner Section Solitary Duodenal Metastasis from Renal Cell Carcinoma with Metachronous Pancreatic Neuroendocrine Tumor: Review of Literature with a Case Discussion Abstract Saphalta Baghmar, Renal cell cancinoma (RCC) is a unique malignancy with features of late recurrences, metastasis S M Shasthry1, to any organ, and frequent association with second malignancy. It most commonly metastasizes Rajesh Singla, to the lungs, bones, liver, renal fossa, and brain although metastases can occur anywhere. RCC 2 metastatic to the duodenum is especially rare, with only few cases reported in the literature. Herein, Yashwant Patidar , 3 we review literature of all the reported cases of solitary duodenal metastasis from RCC and cases Chhagan B Bihari , of neuroendocrine tumor (NET) as synchronous/metachronous malignancy with RCC. Along with S K Sarin1 this, we have described a unique case of an 84‑year‑old man who had recurrence of RCC as solitary Departments of Medical duodenal metastasis after 37 years of radical nephrectomy and metachronous pancreatic NET. Oncology, 1Hepatology, 2Radiology and 3Pathology, Keywords: Late recurrence, pancreatic neuroendocrine tumor, renal cell carcinoma, second Institute of Liver and Biliary malignancy, solitary duodenal metastasis Sciences, New Delhi, India Introduction Case Presentation Renal cell carcinoma (RCC) is unique An 84‑year‑old man with a medical history to have many unusual features such as notable for hypertension and RCC, 37 years metastasis to almost every organ in the body, postright radical nephrectomy status, late recurrences, and frequent association presented to his primary care physician with second malignancy. The most common with fatigue. When found to be anemic, sites of metastasis are the lung, lymph he was treated with iron supplementation nodes, liver, bone, adrenal glands, kidney, and blood transfusions. -

Adrenal Teratoma: a Rare Retroperitoneal Tumor
MOJ Clinical & Medical Case Reports Case Report Open Access Adrenal teratoma: a rare retroperitoneal tumor Abstract Volume 9 Issue 6 - 2019 Introduction: A teratoma is a relatively common tumor of pediatric age group. But it rarely 1 2 presents as a retroperitoneal mass. We encountered a case of Adrenal teratoma, a rare entity. Nabila Talat Baila, Naeem Liaqat, Ammara Kanwal,3 Imran Hashim,1 Muhammad Case Presentation: An 11 years old boy presented with pain in right lumbar region. His Saleem,1 Muhammad Sarfraz1 examination was unremarkable. Work up showed a suprarenal mass that turned out to be 1Pediatric Surgery, Children hospital/ Lahore, Pakistan an adrenal teratoma. 2Pediatric Surgery Rawalpindi Medical University, Pakistan Conclusion: Adrenal teratomas may mimic adrenal cancers and should be considered a Dr. Ammara Kanwal, Rawalpindi Medical necessary differential, especially in children and adolescents. Correspondence: University, CB-138 New Lala Rukh Wah cantt, District Keywords: teratoma, germ cell tumor, retroperitoneal tumors, childhood neoplasm, rare Rawalpindi, Punjab, Pakistan, Tel +923425564478, masses Email Received: November 11, 2019 | Published: December 10, 2019 Introduction Teratoma is a germ cell tumor, usually manifesting in children and adolescents. It typically forms in gonads or in axial structures, probably, following the path of germ cells during embryonic development. Retroperitoneal teratoma is a very uncommon variety of germ cell tumors, seen in only approximately 5% of infantile cases. Whereas adrenal teratoma is extremely rare.1 In this case report, we present such a rare case of a boy with adrenal teratoma. Case presentation An 11years old boy, a known case of Down’s syndrome, presented with localized and intermittent pain in right lumbar region for one year.