Well Differentiated Grade 3 Neuroendocrine Tumors Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pro-Oxidizing Metabolic Weapons ☆ ⁎ Etelvino J.H
Comparative Biochemistry and Physiology, Part C 146 (2007) 88–110 www.elsevier.com/locate/cbpc Review The dual face of endogenous α-aminoketones: Pro-oxidizing metabolic weapons ☆ ⁎ Etelvino J.H. Bechara a, , Fernando Dutra b, Vanessa E.S. Cardoso a, Adriano Sartori a, Kelly P.K. Olympio c, Carlos A.A. Penatti d, Avishek Adhikari e, Nilson A. Assunção a a Departamento de Bioquímica, Instituto de Química, Universidade de São Paulo, Av. Prof. Lineu Prestes 748, 05508-900, São Paulo, SP, Brazil b Centro de Ciências Biológicas e da Saúde, Universidade Cruzeiro do Sul, São Paulo, SP, Brazil c Faculdade de Saúde Pública, Universidade de São Paulo, São Paulo, SP, Brazil d Department of Physiology, Dartmouth Medical School, Hanover, NH, USA e Department of Biological Sciences, Columbia University, New York, NY, USA Received 31 January 2006; received in revised form 26 June 2006; accepted 6 July 2006 Available online 14 July 2006 Abstract Amino metabolites with potential prooxidant properties, particularly α-aminocarbonyls, are the focus of this review. Among them we emphasize 5-aminolevulinic acid (a heme precursor formed from succinyl–CoA and glycine), aminoacetone (a threonine and glycine metabolite), and hexosamines and hexosimines, formed by Schiff condensation of hexoses with basic amino acid residues of proteins. All these metabolites were shown, in vitro, to undergo enolization and subsequent aerobic oxidation, yielding oxyradicals and highly cyto- and genotoxic α-oxoaldehydes. Their metabolic roles in health and disease are examined here and compared in humans and experimental animals, including rats, quail, and octopus. In the past two decades, we have concentrated on two endogenous α-aminoketones: (i) 5-aminolevulinic acid (ALA), accumulated in acquired (e.g., lead poisoning) and inborn (e.g., intermittent acute porphyria) porphyric disorders, and (ii) aminoacetone (AA), putatively overproduced in diabetes mellitus and cri-du-chat syndrome. -

Multiple Low-Dose Streptozotocin-Induced Diabetes in the Mouse
Multiple low-dose streptozotocin-induced diabetes in the mouse. Evidence for stimulation of a cytotoxic cellular immune response against an insulin-producing beta cell line. R C McEvoy, … , S Sandler, C Hellerström J Clin Invest. 1984;74(3):715-722. https://doi.org/10.1172/JCI111487. Research Article Mice were examined for the presence of splenocytes specifically cytotoxic for a rat insulinoma cell line (RIN) during the induction of diabetes by streptozotocin (SZ) in multiple low doses (Multi-Strep). Cytotoxicity was quantitated by the release of 51Cr from damaged cells. A low but statistically significant level of cytolysis (5%) by splenocytes was first detectable on day 8 after the first dose of SZ. The cytotoxicity reached a maximum of approximately 9% on day 10 and slowly decreased thereafter, becoming undetectable 42 d after SZ was first given. The time course of the in vitro cytotoxic response correlated with the degree of insulitis demonstrable in the pancreata of the Multi-Strep mice. The degree of cytotoxicity after Multi-Strep was related to the number of effector splenocytes to which the target RIN cells were exposed and was comparable to that detectable after immunization by intraperitoneal injection of RIN cells in normal mice. The cytotoxicity was specific for insulin-producing cells; syngeneic, allogeneic, and xenogeneic lymphocytes and lymphoblasts, 3T3 cells, and a human keratinocyte cell line were not specifically lysed by the splenocytes of the Multi- Strep mice. This phenomenon was limited to the Multi-Strep mice. Splenocytes from mice made diabetic by a single, high dose of SZ exhibited a very low level of cytotoxicity against the RIN cells. -

Clinicopathological Characteristics and KRAS Mutation Status of Endometrial Mucinous Metaplasia and Carcinoma JI-YOUN SUNG 1, YOON YANG JUNG 2 and HYUN-SOO KIM 3
ANTICANCER RESEARCH 38 : 2779-2786 (2018) doi:10.21873/anticanres.12521 Clinicopathological Characteristics and KRAS Mutation Status of Endometrial Mucinous Metaplasia and Carcinoma JI-YOUN SUNG 1, YOON YANG JUNG 2 and HYUN-SOO KIM 3 1Department of Pathology, Kyung Hee University School of Medicine, Seoul, Republic of Korea; 2Department of Pathology, Myongji Hospital, Goyang, Republic of Korea; 3Department of Pathology, Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea Abstract. Background/Aim: Mucinous metaplasia of the papillary mucinous metaplasia suggests that papillary endometrium occurs as a spectrum of epithelial alterations mucinous metaplasia may be a precancerous lesion of a ranging from the formation of simple, tubular glands to certain subset of mucinous carcinomas of the endometrium. architecturally complex glandular proliferation with intraglandular papillary projection and cellular tufts. Endometrial metaplasia is defined as epithelial differentiation Endometrial mucinous metaplasia often presents a diagnostic that differs from the conventional morphological appearance challenge in endometrial curettage. Materials and Methods: of the endometrial glandular epithelium (1). Endometrial We analyzed the clinicopathological characteristics and the mucinous metaplasia is particularly relevant as it is mutation status for V-Ki-ras2 Kirsten rat sarcoma viral frequently encountered in endometrial curettage specimens oncogene homolog (KRAS) of 11 cases of endometrial obtained from peri-menopausal or postmenopausal women mucinous metaplasia. Electronic medical record review and (2). Mucinous epithelial lesions of the endometrium present histopathological examination were performed. KRAS a frequent disparity between cytological atypia and mutation status was analyzed using a pyrosequencing architectural alteration, and often present significant technique. Results: Cases were classified histopathologically diagnostic challenges to pathologists. -

Primary Hepatic Neuroendocrine Carcinoma: Report of Two Cases and Literature Review
The Jackson Laboratory The Mouseion at the JAXlibrary Faculty Research 2018 Faculty Research 3-1-2018 Primary hepatic neuroendocrine carcinoma: report of two cases and literature review. Zi-Ming Zhao The Jackson Laboratory, [email protected] Jin Wang Ugochukwu C Ugwuowo Liming Wang Jeffrey P Townsend Follow this and additional works at: https://mouseion.jax.org/stfb2018 Part of the Life Sciences Commons, and the Medicine and Health Sciences Commons Recommended Citation Zhao, Zi-Ming; Wang, Jin; Ugwuowo, Ugochukwu C; Wang, Liming; and Townsend, Jeffrey P, "Primary hepatic neuroendocrine carcinoma: report of two cases and literature review." (2018). Faculty Research 2018. 71. https://mouseion.jax.org/stfb2018/71 This Article is brought to you for free and open access by the Faculty Research at The ousM eion at the JAXlibrary. It has been accepted for inclusion in Faculty Research 2018 by an authorized administrator of The ousM eion at the JAXlibrary. For more information, please contact [email protected]. Zhao et al. BMC Clinical Pathology (2018) 18:3 https://doi.org/10.1186/s12907-018-0070-7 CASE REPORT Open Access Primary hepatic neuroendocrine carcinoma: report of two cases and literature review Zi-Ming Zhao1,2*† , Jin Wang3,4,5†, Ugochukwu C. Ugwuowo6, Liming Wang4,8* and Jeffrey P. Townsend2,7* Abstract Background: Primary hepatic neuroendocrine carcinoma (PHNEC) is extremely rare. The diagnosis of PHNEC remains challenging—partly due to its rarity, and partly due to its lack of unique clinical features. Available treatment options for PHNEC include surgical resection of the liver tumor(s), radiotherapy, liver transplant, transcatheter arterial chemoembolization (TACE), and administration of somatostatin analogues. -

81196615.Pdf
Biochimie 94 (2012) 374e383 Contents lists available at ScienceDirect Biochimie journal homepage: www.elsevier.com/locate/biochi Research paper Effects of resveratrol on biomarkers of oxidative stress and on the activity of delta aminolevulinic acid dehydratase in liver and kidney of streptozotocin-induced diabetic rats Roberta Schmatz a,*, Luciane Belmonte Perreira a, Naiara Stefanello a, Cinthia Mazzanti a, Roselia Spanevello a,c, Jessié Gutierres a, Margarete Bagatini b, Caroline Curry Martins a, Fátima Husein Abdalla a, Jonas Daci da Silva Serres a, Daniela Zanini a, Juliano Marchi Vieira a, Andréia Machado Cardoso a, Maria Rosa Schetinger a, Vera Maria Morsch a,* a Programa de Pós Graduação em Bioquímica Toxicológica, Centro de Ciências Naturais e Exatas, Universidade Federal de Santa Maria, Campus Universitário, Camobi, 97105-900 Santa Maria, RS, Brazil b Colegiado do curso de Enfermagem, Universidade Federal da Fronteira Sul, Campus Chapecó, Chapecó, SC, Brazil c Universidade Federal de Pelotas, Centro de Ciências Químicas, Farmacêuticas e de Alimentos, Setor de Bioquímica, Campus Universitário Capão do Leão 96010-900 Pelotas, RS, Brazil article info abstract Article history: The present study investigated the effects of resveratrol (RV), a polyphenol with potent antioxidant Received 24 April 2011 properties, on oxidative stress parameters in liver and kidney, as well as on serum biochemical Accepted 8 August 2011 parameters of streptozotocin (STZ)-induced diabetic rats. Animals were divided into six groups (n ¼ 8): Available online 16 August 2011 control/saline; control/RV 10 mg/kg; control/RV 20 mg/kg; diabetic/saline; diabetic/RV10 mg/kg; dia- betic/RV 20 mg/kg. After 30 days of treatment with resveratrol the animals were sacrificed and the liver, Keywords: kidney and serum were used for experimental determinations. -

What Is a Gastrointestinal Carcinoid Tumor?
cancer.org | 1.800.227.2345 About Gastrointestinal Carcinoid Tumors Overview and Types If you have been diagnosed with a gastrointestinal carcinoid tumor or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is a Gastrointestinal Carcinoid Tumor? Research and Statistics See the latest estimates for new cases of gastrointestinal carcinoid tumor in the US and what research is currently being done. ● Key Statistics About Gastrointestinal Carcinoid Tumors ● What’s New in Gastrointestinal Carcinoid Tumor Research? What Is a Gastrointestinal Carcinoid Tumor? Gastrointestinal carcinoid tumors are a type of cancer that forms in the lining of the gastrointestinal (GI) tract. Cancer starts when cells begin to grow out of control. To learn more about what cancer is and how it can grow and spread, see What Is Cancer?1 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 To understand gastrointestinal carcinoid tumors, it helps to know about the gastrointestinal system, as well as the neuroendocrine system. The gastrointestinal system The gastrointestinal (GI) system, also known as the digestive system, processes food for energy and rids the body of solid waste. After food is chewed and swallowed, it enters the esophagus. This tube carries food through the neck and chest to the stomach. The esophagus joins the stomachjust beneath the diaphragm (the breathing muscle under the lungs). The stomach is a sac that holds food and begins the digestive process by secreting gastric juice. The food and gastric juices are mixed into a thick fluid, which then empties into the small intestine. -
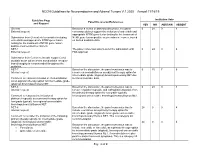
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19 Guideline Page Institution Vote Panel Discussion/References and Request YES NO ABSTAIN ABSENT General Based on a review of data and discussion, the panel 0 24 0 4 External request: consensus did not support the inclusion of entrectinib and appropriate NTRK gene fusion testing for the treatment of Submission from Genentech to consider including NTRK gene fusion-positive neuroendocrine cancer, based entrectinib and appropriate NTRK gene fusion on limited available data. testing for the treatment of NTRK gene fusion- positive neuroendocrine cancers. NET-1 The panel consensus was to defer the submission until 0 24 0 4 External request: FDA approval. Submission from Curium to include copper Cu 64 dotatate as an option where somatostatin receptor- based imaging is recommended throughout the guideline. NET-7 Based on the discussion, the panel consensus was to 0 15 7 6 Internal request: remove chemoradiation as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET due Comment to reassess inclusion of chemoradiation to limited available data. as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET. NET-8 Based on the discussion, the panel consensus was to 0 24 0 4 Internal request: remove cisplatin/etoposide and carboplatin/etoposide from the primary therapy option for low grade (typical), Comment to reassess the inclusion of locoregional unresectable bronchopulmonary/thymus NET. platinum/etoposide as a primary therapy option for low grade (typical), locoregional unresectable bronchopulmonary/thymus NET. NET-8 Based on the discussion, the panel consensus was to 24 0 0 4 Internal request: include everolimus as a primary therapy option for intermediate grade (atypical), locoregional unresectable Comment to consider the inclusion of the following bronchopulmonary/thymus NET. -

Phase III Trial of Chemotherapy Using 5-Fluorouracil and Streptozotocin
Endocrine-Related Cancer (2009) 16 1351–1361 Phase III trial of chemotherapy using 5-fluorouracil and streptozotocin compared with interferon a for advanced carcinoid tumors: FNCLCC–FFCD 9710 Laetitia Dahan1*, Frank Bonnetain2*, Philippe Rougier 3, Jean-Luc Raoul 4, Eric Gamelin5, Pierre-Luc Etienne6, Guillaume Cadiot 7, Emmanuel Mitry4, Denis Smith8, Fre´de´rique Cvitkovic9, Bruno Coudert 10, Floriane Ricard1, Laurent Bedenne1, Jean-Franc¸ois Seitz1 for the Fe´de´ration Francophone de Cance´rologie Digestive (FFCD) and the Digestive Tumors Group of the Fe´de´ration Nationale des Centres de Lutte Contre le Cancer (FNCLCC) 1Assistance Publique, Hoˆpitaux de Marseille, Hoˆpital Timone, Universite´ de la Me´diterrane´e, CHU Timone, 264 rue Saint Pierre, 13385 Marseille Cedex 5, France 2FFCD, Dijon, France 3AP-HP, Hoˆpital Ambroise Pare´, Boulogne, France 4Centre Euge`ne Marquis, Rennes, France 5Centre Paul Papin, Angers, France 6Clinique Armoricaine, Saint Brieuc, France 7Hopital Robert Debre´, Reims, France 8CHU Haut Leveque, Pessac, France 9Centre Rene´ Huguenin, Saint Cloud, France 10Centre Franc¸ois Leclerc, Dijon, France (Correspondence should be addressed to L Dahan; Email: [email protected]) *(L Dahan and F Bonnetain contributed equally to this work) Abstract The aim of this randomized multicenter phase III trial was to compare chemotherapy and interferon (IFN) in patients with metastatic carcinoid tumors. Patients with documented progressive, unresectable, metastatic carcinoid tumors were randomized between 5-fluorouracil plus streptozotocin (day 1–5) and recombinant IFN-a-2a (3 MU!3 per week). Primary endpoint was progression-free survival (PFS). From February 1998 to June 2004, 64 patients were included. -

Rising Incidence of Neuroendocrine Tumors
Rising Incidence of Neuroendocrine Tumors Dasari V, Yao J, et al. JAMA Oncology 2017 S L I D E 1 Overview Pancreatic Neuroendocrine Tumors • Tumors which arise from endocrine cells of the pancreas • 5.6 cases per million – 3% of pancreatic tumors • Median age at diagnosis 60 years • More indolent course compared to adenocarcinoma – 10-year overall survival 40% • Usually sporadic but can be associated with hereditary syndromes – Core genetic pathways altered in sporadic cases • DNA damage repair (MUTYH) Chromatin remodeling (MEN1) • Telomere maintenance (MEN1, DAXX, ATRX) mTOR signaling – Hereditary: 17% of patients with germline mutation Li X, Wang C, et al. Cancer Med 2018 Scarpa A, Grimond S, et al. NatureS L I2017 D E 2 Pathology Classification European American Joint World Health Organization Neuroendocrine Committee on Cancer (WHO) Tumor Society (AJCC) (ENETS) Grade Ki-67 Mitotic rt TNM TNM T1: limit to pancreas, <2 cm T1: limit to pancreas, ≦2 cm T2: limit to pancreas, 2-4 cm T2: >limit to pancreas, 2 cm T3: limit to pancreas, >4 cm, T3: beyond pancreas, no celiac or Low ≤2% <2 invades duodenum, bile duct SMA T4: beyond pancreas, invasion involvement adjacent organs or vessels T4: involves celiac or SMA N0: node negative No: node negative Intermed 3-20% 2-20 N1: node positive N1: node positive M0: no metastases M0: no metastases High >20% >20 M1: metastases M1: metastases S L I D E 3 Classification Based on Functionality • Nonfunctioning tumors – No clinical symptoms (can still produce hormone) – Accounts for 40% of tumors – 60-85% -

Notch Signaling Affects Oral Neoplasm Cell Differentiation And
International Journal of Molecular Sciences Review Notch Signaling Affects Oral Neoplasm Cell Differentiation and Acquisition of Tumor-Specific Characteristics Keisuke Nakano 1,*, Kiyofumi Takabatake 1, Hotaka Kawai 1, Saori Yoshida 1, Hatsuhiko Maeda 2, Toshiyuki Kawakami 3 and Hitoshi Nagatsuka 1 1 Department of Oral Pathology and Medicine, Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama University, Okayama 700-8558, Japan; [email protected] (K.T.); [email protected] (H.K.); [email protected] (S.Y.); [email protected] (H.N.) 2 Department of Oral Pathology, School of Dentistry, Aichi Gakuin University, Nagoya 464-8650, Japan; [email protected] 3 Hard Tissue Pathology Unit, Matsumoto Dental University Graduate School of Oral Medicine, Shiojiri 399-0781, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-086-235-6651 Received: 19 March 2019; Accepted: 21 April 2019; Published: 23 April 2019 Abstract: Histopathological findings of oral neoplasm cell differentiation and metaplasia suggest that tumor cells induce their own dedifferentiation and re-differentiation and may lead to the formation of tumor-specific histological features. Notch signaling is involved in the maintenance of tissue stem cell nature and regulation of differentiation and is responsible for the cytological regulation of cell fate, morphogenesis, and/or development. In our previous study, immunohistochemistry was used to examine Notch expression using cases of odontogenic tumors and pleomorphic adenoma as oral neoplasms. According to our results, Notch signaling was specifically associated with tumor cell differentiation and metaplastic cells of developmental tissues. -

The Pathology of Cancer
University of Massachusetts Medical School eScholarship@UMMS Cancer Concepts: A Guidebook for the Non- Oncologist Radiation Oncology 2018-08-03 The Pathology of Cancer Chi Young Ok The University of Texas MD Anderson Cancer Center Et al. Let us know how access to this document benefits ou.y Follow this and additional works at: https://escholarship.umassmed.edu/cancer_concepts Part of the Cancer Biology Commons, Medical Education Commons, Neoplasms Commons, Oncology Commons, Pathological Conditions, Signs and Symptoms Commons, and the Pathology Commons Repository Citation Ok CY, Woda BA, Kurian E. (2018). The Pathology of Cancer. Cancer Concepts: A Guidebook for the Non- Oncologist. https://doi.org/10.7191/cancer_concepts.1023. Retrieved from https://escholarship.umassmed.edu/cancer_concepts/26 Creative Commons License This work is licensed under a Creative Commons Attribution-Noncommercial-Share Alike 4.0 License. This material is brought to you by eScholarship@UMMS. It has been accepted for inclusion in Cancer Concepts: A Guidebook for the Non-Oncologist by an authorized administrator of eScholarship@UMMS. For more information, please contact [email protected]. The Pathology of Cancer Citation: Ok CY, Woda B, Kurian E. The Pathology of Cancer. In: Pieters RS, Liebmann J, eds. Chi Young Ok, MD Cancer Concepts: A Guidebook for the Non-Oncologist. Worcester, MA: University of Massachusetts Bruce Woda, MD Medical School; 2017. doi: 10.7191/cancer_concepts.1023. Elizabeth Kurian, MD This project has been funded in whole or in part with federal funds from the National Library of Medicine, National Institutes of Health, under Contract No. HHSN276201100010C with the University of Massachusetts, Worcester. -
Fungal Endophytes As Efficient Sources of Plant-Derived Bioactive
microorganisms Review Fungal Endophytes as Efficient Sources of Plant-Derived Bioactive Compounds and Their Prospective Applications in Natural Product Drug Discovery: Insights, Avenues, and Challenges Archana Singh 1,2, Dheeraj K. Singh 3,* , Ravindra N. Kharwar 2,* , James F. White 4,* and Surendra K. Gond 1,* 1 Department of Botany, MMV, Banaras Hindu University, Varanasi 221005, India; [email protected] 2 Department of Botany, Institute of Science, Banaras Hindu University, Varanasi 221005, India 3 Department of Botany, Harish Chandra Post Graduate College, Varanasi 221001, India 4 Department of Plant Biology, Rutgers University, New Brunswick, NJ 08901, USA * Correspondence: [email protected] (D.K.S.); [email protected] (R.N.K.); [email protected] (J.F.W.); [email protected] (S.K.G.) Abstract: Fungal endophytes are well-established sources of biologically active natural compounds with many producing pharmacologically valuable specific plant-derived products. This review details typical plant-derived medicinal compounds of several classes, including alkaloids, coumarins, flavonoids, glycosides, lignans, phenylpropanoids, quinones, saponins, terpenoids, and xanthones that are produced by endophytic fungi. This review covers the studies carried out since the first report of taxol biosynthesis by endophytic Taxomyces andreanae in 1993 up to mid-2020. The article also highlights the prospects of endophyte-dependent biosynthesis of such plant-derived pharma- cologically active compounds and the bottlenecks in the commercialization of this novel approach Citation: Singh, A.; Singh, D.K.; Kharwar, R.N.; White, J.F.; Gond, S.K. in the area of drug discovery. After recent updates in the field of ‘omics’ and ‘one strain many Fungal Endophytes as Efficient compounds’ (OSMAC) approach, fungal endophytes have emerged as strong unconventional source Sources of Plant-Derived Bioactive of such prized products.