Primary Hepatic Neuroendocrine Carcinoma: Report of Two Cases and Literature Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

What You Should Know About Familial Adenomatous Polyposis (FAP)
What you should know about Familial Adenomatous Polyposis (FAP) FAP is a very rare condition that accounts for about 1% of new cases of colorectal cancer. People with FAP typically develop hundreds to thousands of polyps (adenomas) in their colon and rectum by age 30-40. Polyps may also develop in the stomach and small intestine. Individuals with FAP can develop non-cancerous cysts on the skin (epidermoid cysts), especially on the scalp. Besides having an increased risk for colon polyps and cysts, individuals with FAP are also more likely to develop sebaceous cysts, osetomas (benign bone tumors) of the jaw, impacted teeth, extra teeth, CHRPE (multiple areas of pigmentation in the retina in the eye) and desmoid disease. Some individuals have milder form of FAP, called attenuated FAP (AFAP), and develop an average of 20 polyps at a later age. The risk for cancer associated with FAP If left untreated, the polyps in the colon and rectum will develop in to cancer, usually before age 50. Individuals with FAP also have an increased risk for stomach cancer, papillary thyroid cancer, periampullary carcinoma, hepatoblastoma (in childhood), and brain tumors. The risks to family members FAP is caused by mutations in the Adenomatous Polyposis Coli (APC) gene. Approximately 1/3 of people with FAP do not have family history of the disease, and thus have a new mutation. FAP is inherited in a dominant fashion. Children of a person with an APC mutation have a 50% risk to inherit the mutation. Brothers, sisters, and parents of individuals with FAP should also be checked to see if they have an APC mutation. -

Cholangiocarcinoma 2020: the Next Horizon in Mechanisms and Management
CONSENSUS STATEMENT Cholangiocarcinoma 2020: the next horizon in mechanisms and management Jesus M. Banales 1,2,3 ✉ , Jose J. G. Marin 2,4, Angela Lamarca 5,6, Pedro M. Rodrigues 1, Shahid A. Khan7, Lewis R. Roberts 8, Vincenzo Cardinale9, Guido Carpino 10, Jesper B. Andersen 11, Chiara Braconi 12, Diego F. Calvisi13, Maria J. Perugorria1,2, Luca Fabris 14,15, Luke Boulter 16, Rocio I. R. Macias 2,4, Eugenio Gaudio17, Domenico Alvaro18, Sergio A. Gradilone19, Mario Strazzabosco 14,15, Marco Marzioni20, Cédric Coulouarn21, Laura Fouassier 22, Chiara Raggi23, Pietro Invernizzi 24, Joachim C. Mertens25, Anja Moncsek25, Sumera Rizvi8, Julie Heimbach26, Bas Groot Koerkamp 27, Jordi Bruix2,28, Alejandro Forner 2,28, John Bridgewater 29, Juan W. Valle 5,6 and Gregory J. Gores 8 Abstract | Cholangiocarcinoma (CCA) includes a cluster of highly heterogeneous biliary malignant tumours that can arise at any point of the biliary tree. Their incidence is increasing globally, currently accounting for ~15% of all primary liver cancers and ~3% of gastrointestinal malignancies. The silent presentation of these tumours combined with their highly aggressive nature and refractoriness to chemotherapy contribute to their alarming mortality, representing ~2% of all cancer-related deaths worldwide yearly. The current diagnosis of CCA by non-invasive approaches is not accurate enough, and histological confirmation is necessary. Furthermore, the high heterogeneity of CCAs at the genomic, epigenetic and molecular levels severely compromises the efficacy of the available therapies. In the past decade, increasing efforts have been made to understand the complexity of these tumours and to develop new diagnostic tools and therapies that might help to improve patient outcomes. -

Treatment Strategies for Hepatocellular Carcinoma—A Multidisciplinary Approach
International Journal of Molecular Sciences Review Treatment Strategies for Hepatocellular Carcinoma—A Multidisciplinary Approach Isabella Lurje 1,† , Zoltan Czigany 1,† , Jan Bednarsch 1, Christoph Roderburg 2,3, Peter Isfort 4, Ulf Peter Neumann 1,5 and Georg Lurje 1,* 1 Department of Surgery and Transplantation, University Hospital RWTH Aachen, 52074 Aachen, Germany; [email protected] (I.L.); [email protected] (Z.C.); [email protected] (J.B.); [email protected] (U.P.N.) 2 Department of Internal Medicine III, University Hospital RWTH Aachen, 52074 Aachen, Germany; [email protected] 3 Department of Gastroenterology/Hepatology, Campus Virchow Klinikum and Charité Mitte, Charité University Medicine Berlin, 13353 Berlin, Germany 4 Department for Diagnostic and Interventional Radiology, University Hospital RWTH Aachen, 52074 Aachen, Germany; [email protected] 5 Department of Surgery, Maastricht University Medical Centre (MUMC), 6229 ET Maastricht, The Netherlands * Correspondence: [email protected] † Both authors contributed equally to this work. Received: 9 March 2019; Accepted: 21 March 2019; Published: 22 March 2019 Abstract: Hepatocellular carcinoma (HCC) is the most common primary tumor of the liver and its mortality is third among all solid tumors, behind carcinomas of the lung and the colon. Despite continuous advancements in the management of this disease, the prognosis for HCC remains inferior compared to other tumor entities. While orthotopic liver transplantation (OLT) and surgical resection are the only two curative treatment options, OLT remains the best treatment strategy as it not only removes the tumor but cures the underlying liver disease. As the applicability of OLT is nowadays limited by organ shortage, major liver resections—even in patients with underlying chronic liver disease—are adopted increasingly into clinical practice. -
Case Report Metastasis of Pancreatic Cancer Within Primary Colon Cancer by Overtaking the Stromal Microenvironment
Int J Clin Exp Pathol 2018;11(6):3141-3146 www.ijcep.com /ISSN:1936-2625/IJCEP0075771 Case Report Metastasis of pancreatic cancer within primary colon cancer by overtaking the stromal microenvironment Takeo Nakaya1, Hisashi Oshiro1, Takumi Saito2, Yasunaru Sakuma2, Hisanaga Horie2, Naohiro Sata2, Akira Tanaka1 Departments of 1Pathology, 2Surgery, Jichi Medical University, Shimotsuke, Tochigi, Japan Received March 10, 2018; Accepted April 15, 2018; Epub June 1, 2018; Published June 15, 2018 Abstract: We report a unique case of a 74-old man, who presented with double cancers, showing metastasis of pancreatic cancer to colon cancer. Histopathological examination after surgery revealed that the patient had as- cending colon cancer, which metastasized to the liver (pT4N0M1), as well as pancreatic cancer (pT2N1M1) that metastasized to the most invasive portion of the colon cancer, namely the serosal to subserosal layers. Although the mechanisms for this scenario have yet to be elucidated, we speculate that the metastatic pancreatic carcinoma overtook the stromal microenvironment of the colon cancer. Namely, the cancer microenvironment enriched by can- cer-associated fibroblasts, which supported the colon cancer, might be suitable for the invasion and engraftment by pancreatic carcinoma. The similarity of histological appearance might make it difficult to distinguish metastatic pancreatic carcinoma within colon cancer. Furthermore, the metastasis of pancreatic carcinoma in colon carcinoma might be more common, despite it not having been previously reported. Keywords: Cancer metastasis, metastatic pancreatic cancer, colon cancer, double cancer, tumor microenviron- ment Introduction Case report Prevention and control of cancer metastasis is Clinical history one of the most important problems in cancer care [1-4]. -

Pecoma—A Rare Liver Tumor
Journal of Clinical Medicine Article PEComa—A Rare Liver Tumor Marek Krawczyk 1, Bogna Ziarkiewicz-Wróblewska 2, Tadeusz Wróblewski 1, Joanna Podgórska 3, Jakub Grzybowski 2, Beata Gierej 2, Piotr Krawczyk 1, Paweł Nyckowski 4, Oskar Kornasiewicz 1, Waldemar Patkowski 1, Piotr Remiszewski 1, Krzysztof Zaj ˛ac 1 and Michał Gr ˛at 1,* 1 Department of General, Transplant and Liver Surgery, Medical University Warsaw, 02-097 Warsaw, Poland; [email protected] (M.K.); [email protected] (T.W.); [email protected] (P.K.); [email protected] (O.K.); [email protected] (W.P.); [email protected] (P.R.); [email protected] (K.Z.) 2 Department of Pathology, Medical University of Warsaw, 02-097 Warsaw, Poland; [email protected] (B.Z.-W.); [email protected] (J.G.); [email protected] (B.G.) 3 2nd Department of Clinical Radiology, Medical University of Warsaw, 02-097 Warsaw, Poland; [email protected] 4 Department of General, Gastroenterological and Oncological Surgery, Medical University Warsaw, 02-097 Warsaw, Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-22-599-2545 Abstract: PEComa (perivascular epithelioid cell tumor) is a rare liver tumor. Decisions regarding patient management are currently based on a few small case series. The aim of this study was to report the clinicopathological features of PEComa in order to provide guidance for management, complemented by our own experience. This retrospective observational study included all patients with PEComa who underwent surgical treatment in two departments between 2002 and 2020. -

Familial Adenomatous Polyposis FAP Booklet 10/18/2001 2:35 PM Page Iv
FAP Booklet 10/18/2001 2:35 PM Page ii The Johns Hopkins Guide for Patients and Families: Familial Adenomatous Polyposis FAP Booklet 10/18/2001 2:35 PM Page iv The Johns Hopkins Guide for Patients and Families: Familial Adenomatous Polyposis © 2000 The Johns Hopkins University FAP Booklet 10/18/2001 2:35 PM Page vi THE JOHNS HOPKINS GUIDE FOR PATIENTS AND FAMILIES: FAMILIAL ADENOMATOUS POLYPOSIS TABLE OF CONTENTS Introduction ……………………………………………………………………………1 What are Polyps ………………………………………………………………………2 What is Familial Adenomatous Polyposis (FAP)? …………………………………2 What is Attenuated FAP (AFAP)?……………………………………………………2 What is the Gastrointestinal Tract? …………………………………………………3 How is FAP Inherited? ………………………………………………………………4 DNA Test for FAP ……………………………………………………………………4 Why is Early Diagnosis Important? …………………………………………………6 Exam Guidelines for People At Risk ………………………………………………6 What are the Symptoms of FAP?.……………………………………………………7 Other Tumors Associated with FAP…………………………………………………7 How is FAP Diagnosed?………………………………………………………………8 What is the Treatment? ………………………………………………………………9 Sexual Function and Childbirth After Surgery ……………………………………9 Guidelines for Follow Up Care for People with FAP ……………………………0 Support Groups for Individuals and Families ……………………………………11 Resources ……………………………………………………………………………12 Publications …………………………………………………………………………14 Glossary ………………………………………………………………………………15 Appendix ……………………………………………………………………………18 FAP Booklet 10/18/2001 2:35 PM Page vii FAP Booklet 10/18/2001 2:35 PM Page 1 INTRODUCTION This booklet is written for individuals with familial adenomatous polyposis (FAP) and their families. The information provided is intended to add to, and is not a substi- tute for, discussions with doctors, genetic counselors, nurses, and other members of the health care team. We encourage you to read the entire booklet in the order in which it is written since each section is built on information in preceding sections. -

What Is a Gastrointestinal Carcinoid Tumor?
cancer.org | 1.800.227.2345 About Gastrointestinal Carcinoid Tumors Overview and Types If you have been diagnosed with a gastrointestinal carcinoid tumor or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is a Gastrointestinal Carcinoid Tumor? Research and Statistics See the latest estimates for new cases of gastrointestinal carcinoid tumor in the US and what research is currently being done. ● Key Statistics About Gastrointestinal Carcinoid Tumors ● What’s New in Gastrointestinal Carcinoid Tumor Research? What Is a Gastrointestinal Carcinoid Tumor? Gastrointestinal carcinoid tumors are a type of cancer that forms in the lining of the gastrointestinal (GI) tract. Cancer starts when cells begin to grow out of control. To learn more about what cancer is and how it can grow and spread, see What Is Cancer?1 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 To understand gastrointestinal carcinoid tumors, it helps to know about the gastrointestinal system, as well as the neuroendocrine system. The gastrointestinal system The gastrointestinal (GI) system, also known as the digestive system, processes food for energy and rids the body of solid waste. After food is chewed and swallowed, it enters the esophagus. This tube carries food through the neck and chest to the stomach. The esophagus joins the stomachjust beneath the diaphragm (the breathing muscle under the lungs). The stomach is a sac that holds food and begins the digestive process by secreting gastric juice. The food and gastric juices are mixed into a thick fluid, which then empties into the small intestine. -

Primary Hepatic Carcinoid Tumor with Poor Outcome Om Parkash Aga Khan University, [email protected]
eCommons@AKU Section of Gastroenterology Department of Medicine March 2016 Primary Hepatic Carcinoid Tumor with Poor Outcome Om Parkash Aga Khan University, [email protected] Adil Ayub Buria Naeem Sehrish Najam Zubair Ahmed Aga Khan University See next page for additional authors Follow this and additional works at: https://ecommons.aku.edu/ pakistan_fhs_mc_med_gastroenterol Part of the Gastroenterology Commons Recommended Citation Parkash, O., Ayub, A., Naeem, B., Najam, S., Ahmed, Z., Jafri, W., Hamid, S. (2016). Primary Hepatic Carcinoid Tumor with Poor Outcome. Journal of the College of Physicians and Surgeons Pakistan, 26(3), 227-229. Available at: https://ecommons.aku.edu/pakistan_fhs_mc_med_gastroenterol/220 Authors Om Parkash, Adil Ayub, Buria Naeem, Sehrish Najam, Zubair Ahmed, Wasim Jafri, and Saeed Hamid This report is available at eCommons@AKU: https://ecommons.aku.edu/pakistan_fhs_mc_med_gastroenterol/220 CASE REPORT Primary Hepatic Carcinoid Tumor with Poor Outcome Om Parkash1, Adil Ayub2, Buria Naeem2, Sehrish Najam2, Zubair Ahmed, Wasim Jafri1 and Saeed Hamid1 ABSTRACT Primary Hepatic Carcinoid Tumor (PHCT) represents an extremely rare clinical entity with only a few cases reported to date. These tumors are rarely associated with metastasis and surgical resection is usually curative. Herein, we report two cases of PHCT associated with poor outcomes due to late diagnosis. Both cases presented late with non-specific symptoms. One patient presented after a 2-week history of symptoms and the second case had a longstanding two years symptomatic interval during which he remained undiagnosed and not properly worked up. Both these cases were diagnosed with hepatic carcinoid tumor, which originates from neuroendocrine cells. Case 1 opted for palliative care and expired in one month’s time. -

A Case of Adult Hepatoblastoma
DOI: https://doi.org/10.22516/25007440.339 Case report A case of adult hepatoblastoma Rafael Pila-Pérez, MD,1 Jaider Luis Saurith-Monterrosa, MD,1* Pedro Rosales-Torres, MD,1 Rafael Pila-Peláez, MD,1 Javier Alberto Artola-González, MD.1 1. Manuel Ascunce Domenech Hospital in Abstract Camaguey, Cuba Background: In contrast to childhood hepatoblastoma, adult hepatoblastoma (HBA) is a rare and not-fully- understood liver tumor with a poor prognosis. To date, about 50 cases have been adequately reported in the *Correspondence: Jaider Luis Saurith-Monterrosa, MD, medical literature. Objective: We present the case of a patient who was discharged from our hospital with a [email protected] diagnosis of hepatocellular carcinoma approximately 3 months before returning. Clinical case: A 60-year-old male patient with a history of alcoholism and heavy smoking was admitted to our hospital for abdominal pain. ......................................... Received: 13/01/19 Physical examination revealed a palpable tumor in the right hypochondrium region. This patient had been Accepted: 18/02/19 discharged approximately 3 months previously with a diagnosis of hepatocellular carcinoma in the course of liver cirrhosis. The patient died, and the autopsy revealed an HBA. Conclusions: Adult hepatoblastoma is an infrequent tumor with a severe prognosis. Many cases are asymptomatic until the time of diagnosis, and the tumor is usually very large. Liver enzymes, alpha-fetus protein, and imaging studies lead to a diagnosis of hepatocellular carcinoma which is a common tumor in adults. Histological study confirms the diagnosis. Due to the poor prognosis for HBA in contrast to better prospects for treatment of hepatoblastoma in children, it is logical to use pediatric treatment in adults. -
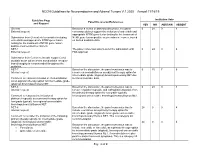
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19 Guideline Page Institution Vote Panel Discussion/References and Request YES NO ABSTAIN ABSENT General Based on a review of data and discussion, the panel 0 24 0 4 External request: consensus did not support the inclusion of entrectinib and appropriate NTRK gene fusion testing for the treatment of Submission from Genentech to consider including NTRK gene fusion-positive neuroendocrine cancer, based entrectinib and appropriate NTRK gene fusion on limited available data. testing for the treatment of NTRK gene fusion- positive neuroendocrine cancers. NET-1 The panel consensus was to defer the submission until 0 24 0 4 External request: FDA approval. Submission from Curium to include copper Cu 64 dotatate as an option where somatostatin receptor- based imaging is recommended throughout the guideline. NET-7 Based on the discussion, the panel consensus was to 0 15 7 6 Internal request: remove chemoradiation as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET due Comment to reassess inclusion of chemoradiation to limited available data. as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET. NET-8 Based on the discussion, the panel consensus was to 0 24 0 4 Internal request: remove cisplatin/etoposide and carboplatin/etoposide from the primary therapy option for low grade (typical), Comment to reassess the inclusion of locoregional unresectable bronchopulmonary/thymus NET. platinum/etoposide as a primary therapy option for low grade (typical), locoregional unresectable bronchopulmonary/thymus NET. NET-8 Based on the discussion, the panel consensus was to 24 0 0 4 Internal request: include everolimus as a primary therapy option for intermediate grade (atypical), locoregional unresectable Comment to consider the inclusion of the following bronchopulmonary/thymus NET. -

Handbook for Children with Liver Tumors
Handbook for Children with TM Liver Tumors Updated Spring 2018 from the Cancer Committee of the American Pediatric Surgical Association ©2018, American Pediatric Surgical Association CONTRIBUTORS Max R. Langham, Jr., MD Vice Chairman, Department of Surgery University of Tennessee Health Science Center Memphis, TN Sanjeev A. Vasudevan, MD Assistant Professor, Division of Pediatric Surgery Director, Pediatric Surgical Oncology Laboratory Texas Children’s Hospital Surgical Oncology Program M.E. DeBakey Department of Surgery, Baylor College of Medicine Houston, TX Rebecka L. Meyers, MD Professor of Surgery Primary Children's Hospital, Dept. of Pediatric Surgery Salt Lake City, UT Gregory M. Tiao, MD Professor of Surgery Frederick Ryckman Chair in Pediatric Surgery Division Chief of Pediatric and Thoracic Surgery Surgical Director, Liver Transplantation Cincinnati Children's Hospital Medical Center Cincinnati, OH Christopher Weldon, MD, PhD Assistant Professor, Pediatric Surgery Dana-Farber/Harvard Cancer Center Children's Hospital Boston, Harvard Medical School Boston, MA TABLE OF CONTENTS 1. Introduction 2. One-Minute Review 3. Staging 4. Radiographic Imaging and Interventional Techniques 5. Biopsy Guidelines 6. Surgical Resection Guidelines 7. Surgical Management of Pulmonary Metastases 8. Guidelines for Liver Transplant and Extreme Resection 9. Surgeon Responsibilities NOTICE The authors, editors, and APSA disclaim any liability, loss, injury or damage incurred as a consequence, directly or indirectly, of the use or application of any of the contents of this volume. While authors and editors have made every effort to create guidelines that should be helpful, it is impossible to create a text that covers every clinical situation that may arise in regards to either diagnosis and/or treatment. -

Rising Incidence of Neuroendocrine Tumors
Rising Incidence of Neuroendocrine Tumors Dasari V, Yao J, et al. JAMA Oncology 2017 S L I D E 1 Overview Pancreatic Neuroendocrine Tumors • Tumors which arise from endocrine cells of the pancreas • 5.6 cases per million – 3% of pancreatic tumors • Median age at diagnosis 60 years • More indolent course compared to adenocarcinoma – 10-year overall survival 40% • Usually sporadic but can be associated with hereditary syndromes – Core genetic pathways altered in sporadic cases • DNA damage repair (MUTYH) Chromatin remodeling (MEN1) • Telomere maintenance (MEN1, DAXX, ATRX) mTOR signaling – Hereditary: 17% of patients with germline mutation Li X, Wang C, et al. Cancer Med 2018 Scarpa A, Grimond S, et al. NatureS L I2017 D E 2 Pathology Classification European American Joint World Health Organization Neuroendocrine Committee on Cancer (WHO) Tumor Society (AJCC) (ENETS) Grade Ki-67 Mitotic rt TNM TNM T1: limit to pancreas, <2 cm T1: limit to pancreas, ≦2 cm T2: limit to pancreas, 2-4 cm T2: >limit to pancreas, 2 cm T3: limit to pancreas, >4 cm, T3: beyond pancreas, no celiac or Low ≤2% <2 invades duodenum, bile duct SMA T4: beyond pancreas, invasion involvement adjacent organs or vessels T4: involves celiac or SMA N0: node negative No: node negative Intermed 3-20% 2-20 N1: node positive N1: node positive M0: no metastases M0: no metastases High >20% >20 M1: metastases M1: metastases S L I D E 3 Classification Based on Functionality • Nonfunctioning tumors – No clinical symptoms (can still produce hormone) – Accounts for 40% of tumors – 60-85%