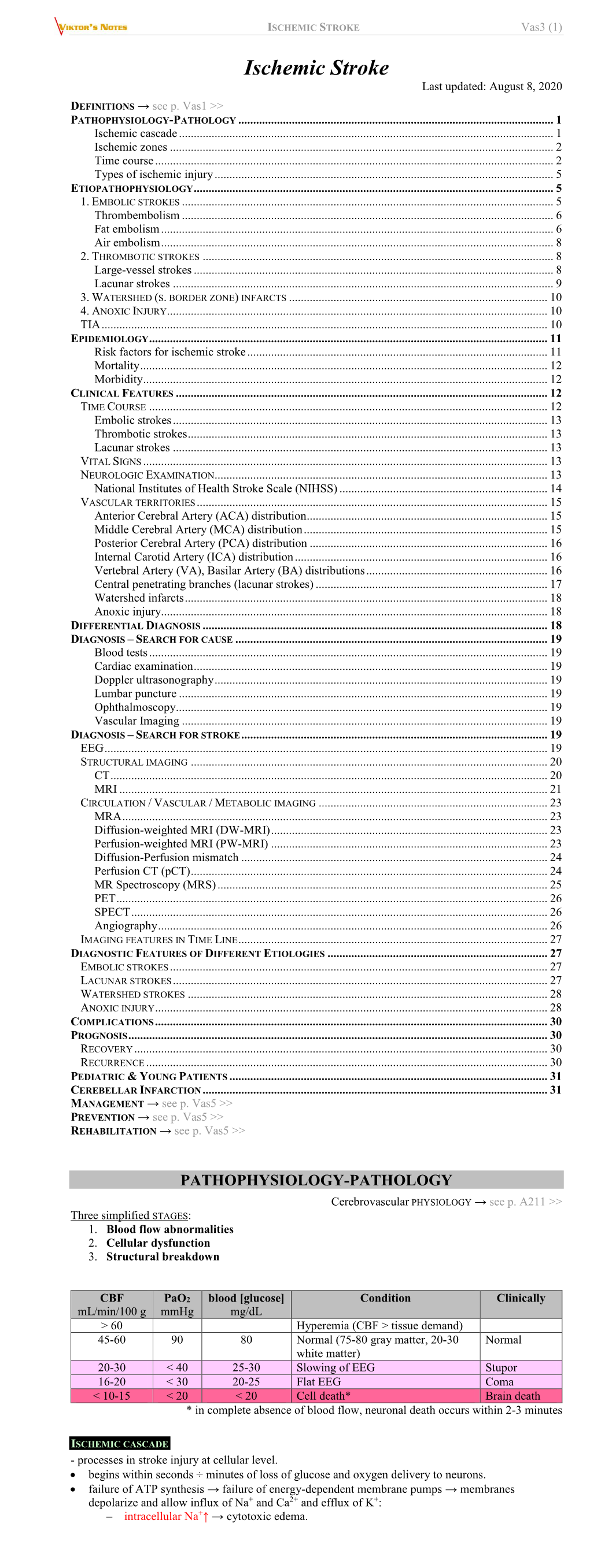
ISCHEMIC STROKE Vas3 (1)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Brain Death and the Cervical Spinal Cord: a Confounding Factor for the Clinical Examination
Spinal Cord (2010) 48, 2–9 & 2010 International Spinal Cord Society All rights reserved 1362-4393/10 $32.00 www.nature.com/sc REVIEW Brain death and the cervical spinal cord: a confounding factor for the clinical examination AR Joffe, N Anton and J Blackwood Department of Pediatrics, Stollery Children’s Hospital, University of Alberta, Edmonton, Alberta, Canada Study design: This study is a systematic review. Objectives: Brain death (BD) is a clinical diagnosis, made by documenting absent brainstem functions, including unresponsive coma and apnea. Cervical spinal cord dysfunction would confound clinical diagnosis of BD. Our objective was to determine whether cervical spinal cord dysfunction is common in BD. Methods: A case of BD showing cervical cord compression on magnetic resonance imaging prompted a literature review from 1965 to 2008 for any reports of cervical spinal cord injury associated with brain herniation or BD. Results: A total of 12 cases of brain herniation in meningitis occurred shortly after a lumbar puncture with acute respiratory arrest and quadriplegia. In total, nine cases of acute brain herniation from various non-meningitis causes resulted in acute quadriplegia. The cases suggest that direct compression of the cervical spinal cord, or the anterior spinal arteries during cerebellar tonsillar herniation cause ischemic injury to the cord. No case series of brain herniation specifically mentioned spinal cord injury, but many survivors had severe disability including spastic limbs. Only two pathological series of BD examined the spinal cord; 56–100% of cases had upper cervical spinal cord damage, suggesting infarction from direct compression of the cord or its arterial blood supply. -

Stroke and Transient Ischaemic Attacks
53454ournal ofNeurology, Neurosurgery, and Psychiatry 1994;57:534-543 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.57.5.534 on 1 May 1994. Downloaded from NEUROLOGICAL MANAGEMENT Stroke and transient ischaemic attacks Peter Humphrey The management of stroke is expensive and ANATOMY accounts for about 5% of NHS hospital costs. Carotid v vertebrobasilar arterial territory Stroke is the commonest cause of severe Carotid-Classifying whether a stroke is in the physical disability. About 100 000 people territory of the carotid or vertebrobasilar suffer a first stroke each year in England and arteries is important, especially if the patient Wales. It is important to emphasise that makes a good recovery. Carotid endarterec- around 20-25% of all strokes affects people tomy is of proven value in those with carotid under 65 years of age. The annual incidence symptoms. Carotid stroke usually produces of stroke is two per 1000.' About 10% of all hemiparesis, hemisensory loss, or dysphasia. patients suffer a recurrent stroke within one Apraxia and visuospatial problems may also year. The prevalence of stroke shows that occur. If there is a severe deficit, there may there are 250 000 in England and Wales. also be an homonymous hemianopia and gaze Each year approximately 60 000 people are palsy. Episodes of amaurosis fugax or central reported to die of stroke; this represents retinal artery occlusion are also carotid about 12% of all deaths. Only ischaemic events. heart disease and cancer account for more Homer's syndrome can occur because of deaths. This means that in an "average" dis- damage to the sympathetic fibres in the trict health authority of 250 000 people, there carotid sheath. -

Cognitive Emotional Sequelae Post Stroke
11/26/2019 The Neuropsychology of Objectives 1. Identify various cognitive sequelae that may result from stroke Stroke: Cognitive & 2. Explain how stroke may impact emotional functioning, both acutely and long-term Emotional Sequelae COX HEALTH STROKE CONFERENCE BRITTANY ALLEN, PHD, ABPP, MBA 12/13/2019 Epidemiology of Stroke Stroke Statistics • > 795,000 people in the United States have a stroke • 5th leading cause of death for Americans • ~610,000 are first or new strokes • Risk of having a first stroke is nearly twice as high for blacks as whites • ~1/4 occur in people with a history of prior stroke • Blacks have the highest rate of death due to stroke • ~140,000 Americans die every year due to stroke • Death rates have declined for all races/ethnicities for decades except that Hispanics have seen • Approximately 87% of all strokes are ischemic an increase in death rates since 2013 • Costs the United States an estimated $34 billion annually • Risk for stroke increases with age, but 34% of people hospitalized for stroke were < 65 years of • Health care services age • Medicines to treat stroke • Women have a lower stroke risk until late in life when the association reverses • Missed days of work • Approximately 15% of strokes are heralded by a TIA • Leading cause of long-term disability • Reduces mobility in > 50% of stroke survivors > 65 years of age Source: Centers for Disease Control Stroke Death Rates Neuropsychological Assessment • Task Engagement • Memory • Language • Visuospatial Functioning • Attention/Concentration • Executive -

Joint Contractures and Acquired Deforming Hypertonia in Older People
Annals of Physical and Rehabilitation Medicine 62 (2019) 435–441 Available online at ScienceDirect www.sciencedirect.com Review Joint contractures and acquired deforming hypertonia in older people: Which determinants? a,b, c d,e a Patrick Dehail *, Nathaly Gaudreault , Haodong Zhou , Ve´ronique Cressot , a,f g h Anne Martineau , Julie Kirouac-Laplante , Guy Trudel a Service de me´decine physique et re´adaptation, poˆle de neurosciences cliniques, CHU de Bordeaux, 33000 Bordeaux, France b Universite´ de Bordeaux, EA 4136, 33000 Bordeaux, France c E´cole de re´adaptation, faculte´ de me´decine et des sciences de la sante´, universite´ de Sherbrooke, Sherbrooke, Canada d Department of Biology, Faculty of Science, University of Ottawa, Ottawa, ON, Canada e Bone and Joint Research Laboratory, Faculty of Medicine, University of Ottawa, Ottawa, ON, Canada f De´partement de me´decine, division de physiatrie, universite´ Laval, Que´bec, QC, Canada g De´partement de me´decine, division de ge´riatrie, universite´ Laval, Que´bec, QC, Canada h Department of Medicine, Division of Physical Medicine and Rehabilitation, University of Ottawa, Bone and Joint Research Laboratory, The Ottawa Hospital Research Institute, Ottawa, ON, Canada A R T I C L E I N F O A B S T R A C T Article history: Joint contractures and acquired deforming hypertonia are frequent in dependent older people. The Received 29 March 2018 consequences of these conditions can be significant for activities of daily living as well as comfort and Accepted 29 October 2018 quality of life. They can also negatively affect the burden of care and care costs. -

Clinicalguidelines
Postgrad MedJ7 1995; 71: 577-584 © The Fellowship of Postgraduate Medicine, 1995 Clinical guidelines Postgrad Med J: first published as 10.1136/pgmj.71.840.577 on 1 October 1995. Downloaded from Management of transient ischaemic attacks and stroke PRD Humphrey Summary The management of stroke and transient ischaemic attacks (TIAs) consumes The management of stroke and about 500 of NHS hospital costs. Stroke is the commonest cause of severe transient ischaemic attacks physical disability with an annual incidence of two per 1000.1 In an 'average' (TIAs) has changed greatly in the district general hospital of 250 000 people there will be 500 first strokes in one last two decades. The importance year with a prevalence of about 1500. TIAs are defined as acute, focal of good blood pressure control is neurological symptoms, resulting from vascular disease which resolve in less the hallmark of stroke preven- than 24 hours. The incidence of a TIA is 0.5 per 1000. tion. Large multicentre trials Stroke is not a diagnosis. It is merely a description of a symptom complex have proven beyond doubt the thought to have a vascular aetiology. It is important to classify stroke according value of aspirin in TIAs, warfarin to the anatomy ofthe lesion, its timing, aetiology and pathogenesis. This will help in patients with atrial fibrillation to decide the most appropriate management. and embolic cerebrovascular symptoms, and carotid endarter- Classification of stroke ectomy in patients with carotid TIAs. There seems little doubt Many neurologists have described erudite vascular syndromes in the past. Most that patients managed in acute ofthese are oflittle practical use. -

Cerebellar Ataxia
CEREBELLAR ATAXIA Dr. Waqar Saeed Ziauddin Medical University, Karachi, Pakistan What is Ataxia? ■ Derived from a Greek word, ‘A’ : not, ‘Taxis’ : orderly Ataxia is defined as an inability to maintain normal posture and smoothness of movement. Types of Ataxia ■ Cerebellar Ataxia ■ Sensory Ataxia ■ Vestibular Ataxia Cerebellar Ataxia Cerebrocerebellum Spinocerebellum Vestibulocerebellum Vermis Planning and Equilibrium balance Posture, limb and initiating and posture eye movements movements Limb position, touch and pressure sensation Limb ataxia, Eye movement dysdiadochokinesia, disorders, Truncal and gait Dysmetria dysarthria nystagmus, VOR, ataxia hypotonia postural and gait. Gait ataxia Types of Cerebellar Ataxia • Vascular Acute Ataxia • Medications and toxins • Infectious etiologies • Atypical Infectious agents • Autoimmune disorders • Primary or metastatic tumors Subacute Ataxia • Paraneoplastic cerebellar degeneration • Alcohol abuse and Vitamin deficiencies • Systemic disorders • Autosomal Dominant Chronic • Autosomal recessive Progressive • X linked ataxias • Mitochondrial • Sporadic neurodegenerative diseases Vascular Ataxia ▪ Benedikt Syndrome It is a rare form of posterior circulation stroke of the brain. A lesion within the tegmentum of the midbrain can produce Benedikt Syndrome. Disease is characterized by ipsilateral third nerve palsy with contralateral hemitremor. Superior cerebellar peduncle and/or red nucleus damage in Benedikt Syndrome can further lead in to contralateral cerebellar hemiataxia. ▪ Wallenberg Syndrome In -

Prosopagnosia by B
J. Neurol. Neurosurg. Psychiat., 1959, 22, 124. PROSOPAGNOSIA BY B. BORNSTEIN and D. P. KIDRON From the Department of Neurology, Beilinson Hospital, Petah Tiqva, Israel "And what is the nature of this knowledge or recollection? I mean to ask, Whether a person, who having seen or heard or in any way perceived anything, knows not only that, but has a conception of something else which is the subject, not of the same but of some other kind of knowledge, may not be fairly said to recollect that of which he has the conception?" "And when the recollection is derived from like things, then another consideration is sure to arise, which is, Whether the likeness in any degree falls short or not of that which is recollected?" "The Philosophy of Plato " Phaedo (the Jowett translation). Does visual agnosia exist in a partial or isolated bances in sensation time, in adaptation time, in form, in which certain qualities only are affected, visual acuity, and in brightness discrimination. as opposed to generalized visual agnosia? Many Ettlinger (1956) rejected Bay's contentions. After workers cast doubt on this concept, maintaining analysing 30 cases of head injury, he showed that that partial visual agnosia is no more than a com- some patients had neither field nor perceptual bination of defects in vision, memory, and orienta- defects, others had field but not perceptual defects, tion, appearing together. and only in eight of the 30 patients were field and The clinical elucidation of partial visual agnosia perceptual defects found together. It is true that is likely to be affected by the patient's intellectual visual agnosia is frequently associated with homony- capacity, his mental state at the time of examination, mous hemianopsia, but despite this there are cases and his ability to cooperate without being influenced of hemianopsia without gnostic defects. -

Neurovascular Anatomy (1): Anterior Circulation Anatomy
Neurovascular Anatomy (1): Anterior Circulation Anatomy Natthapon Rattanathamsakul, MD. December 14th, 2017 Contents: Neurovascular Anatomy Arterial supply of the brain . Anterior circulation . Posterior circulation Arterial supply of the spinal cord Venous system of the brain Neurovascular Anatomy (1): Anatomy of the Anterior Circulation Carotid artery system Ophthalmic artery Arterial circle of Willis Arterial territories of the cerebrum Cerebral Vasculature • Anterior circulation: Internal carotid artery • Posterior circulation: Vertebrobasilar system • All originates at the arch of aorta Flemming KD, Jones LK. Mayo Clinic neurology board review: Basic science and psychiatry for initial certification. 2015 Common Carotid Artery • Carotid bifurcation at the level of C3-4 vertebra or superior border of thyroid cartilage External carotid artery Supply the head & neck, except for the brain the eyes Internal carotid artery • Supply the brain the eyes • Enter the skull via the carotid canal Netter FH. Atlas of human anatomy, 6th ed. 2014 Angiographic Correlation Uflacker R. Atlas of vascular anatomy: an angiographic approach, 2007 External Carotid Artery External carotid artery • Superior thyroid artery • Lingual artery • Facial artery • Ascending pharyngeal artery • Posterior auricular artery • Occipital artery • Maxillary artery • Superficial temporal artery • Middle meningeal artery – epidural hemorrhage Netter FH. Atlas of human anatomy, 6th ed. 2014 Middle meningeal artery Epidural hematoma http://www.jrlawfirm.com/library/subdural-epidural-hematoma -
Noninvasive Evaluation of Myocardial Ischemia and Left Ventricular Function
Linköping University Medical Dissertations No. 1109 Noninvasive Evaluation of Myocardial Ischemia and Left Ventricular Function Eva Maret Division of Cardiovascular Medicine Department of Medical and Health Sciences Linköping University, Sweden Linköping 2009 Eva Maret, 2009 Cover picture/illustration: William Björklund Published articles have been reprinted with the permission of the copyright holder. Printed in Sweden by LiU-Tryck, Linköping, Sweden, 2009 ISBN 978-91-7393-675-0 ISSN 0345-0082 To Martin and John! Somewhere over the rainbow Way up high, There's a land that I heard of Once in a lullaby. Somewhere over the rainbow Skies are blue, And the dreams that you dare to dream Really do come true. From “The Wizard of OZ”, music by Harold Arlen and lyrics by E.Y. Harburg CONTENTS POPULÄRVETENSKAPLIG SAMMANFATTNING ................................................................ 7 LIST OF PUBLICATIONS .......................................................................................................... 9 INTRODUCTION ....................................................................................................................... 13 Coronary Artery Disease ........................................................................................................ 13 Coronary flow, resistance and flow reserve ........................................................................... 14 Coronary atherosclerosis and myocardial infarction .............................................................. 15 Left ventricular function -

Supranuclear and Internuclear Ocular Motility Disorders
CHAPTER 19 Supranuclear and Internuclear Ocular Motility Disorders David S. Zee and David Newman-Toker OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN OCULAR MOTOR SYNDROMES CAUSED BY LESIONS OF THE MEDULLA THE SUPERIOR COLLICULUS Wallenberg’s Syndrome (Lateral Medullary Infarction) OCULAR MOTOR SYNDROMES CAUSED BY LESIONS OF Syndrome of the Anterior Inferior Cerebellar Artery THE THALAMUS Skew Deviation and the Ocular Tilt Reaction OCULAR MOTOR ABNORMALITIES AND DISEASES OF THE OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN BASAL GANGLIA THE CEREBELLUM Parkinson’s Disease Location of Lesions and Their Manifestations Huntington’s Disease Etiologies Other Diseases of Basal Ganglia OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN THE PONS THE CEREBRAL HEMISPHERES Lesions of the Internuclear System: Internuclear Acute Lesions Ophthalmoplegia Persistent Deficits Caused by Large Unilateral Lesions Lesions of the Abducens Nucleus Focal Lesions Lesions of the Paramedian Pontine Reticular Formation Ocular Motor Apraxia Combined Unilateral Conjugate Gaze Palsy and Internuclear Abnormal Eye Movements and Dementia Ophthalmoplegia (One-and-a-Half Syndrome) Ocular Motor Manifestations of Seizures Slow Saccades from Pontine Lesions Eye Movements in Stupor and Coma Saccadic Oscillations from Pontine Lesions OCULAR MOTOR DYSFUNCTION AND MULTIPLE OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN SCLEROSIS THE MESENCEPHALON OCULAR MOTOR MANIFESTATIONS OF SOME METABOLIC Sites and Manifestations of Lesions DISORDERS Neurologic Disorders that Primarily Affect the Mesencephalon EFFECTS OF DRUGS ON EYE MOVEMENTS In this chapter, we survey clinicopathologic correlations proach, although we also discuss certain metabolic, infec- for supranuclear ocular motor disorders. The presentation tious, degenerative, and inflammatory diseases in which su- follows the schema of the 1999 text by Leigh and Zee (1), pranuclear and internuclear disorders of eye movements are and the material in this chapter is intended to complement prominent. -

Diagnosing Dementia: Signs, Symptoms and Meaning
Université de Montréal Diagnosing Dementia: Signs, Symptoms and Meaning Pa= Janice Elizabeth Graham Département d'anthropologie Faculté des arts et des sciences Thèse présentée à la Faculté des études supérieures en vue de l'obtention du grade de Philosophia Doctor 0h.D.) en anthropologie Janice E.Graharn, 1996 National Library Bibliothèque nationale I*I of Canada du Canada Acquisitions and Acquisitions et Bibtiographic Services services bibliographiques 395 Wellington Street 395, rue Wellington Ottawa ON K1A ON4 Ottawa ON KIA ON4 Canada Canada Vour fik Vorre réference Our file Notre refdrence The author has granted a non- L'auteur a accordé une licence non exclusive licence dowing the exdusive permettant à la National Library of Canada to Bibliothèque nationde du Canada de reproduce, loan, distribute or sell reproduire, prêter, distribuer ou copies of this thesis in microform, vendre des copies de cette thèse sous paper or electronic formats. la fome de microfiche/nlm, de reproduction sur papier ou sur format électroniq2e. The author retains ownership of the L'auteur conserve la propriété du copyright in this thesis. Neither the droit d'auteur qui protège cette thèse. thesis nor substantial extracts f?om it Ni la thèse ni des extraits substantiels may be printed or othenvise de celle-ci ne doivent être imprimés reproduced without the author's ou autrement reproduits sans son permission. autorisation. Université de Montréal Faculte des Btudes superieures Cette thèse ultitulee: Diagnosing Dementia: Signs, Symptoms and Meaning presentée -

Chapter 1: Stroke and Neuroprotection 1 – 21
DEVELOPMENT OF NOVEL THERAPEUTICS FOR STROKE: PRECLINICAL INVESTIGATIONS OF OSTEOPONTIN AND 3-IODOTHYRONAMINE By Kristian Paul Doyle A DISSERTATION Presented to the Department of Molecular Microbiology & Immunology at the Oregon Health & Science University in partial fulfillment of the requirements for the degree of Doctor of Philosophy 1 CONTENTS List of Figures v List of Tables ix Acknowledgements x Preface xi Abstract xii List of Abbreviations xv Chapter 1: Stroke and Neuroprotection 1 – 21 1.1 Introduction 2 1.2 Brief History of Stroke 2 1.3 Stroke Pathophysiology 4 1.4 Neuroprotection 17 1.5 Ischemic Preconditioning 19 1.6 Research Goal 21 Chapter 2: Osteopontin 22-86 2.1 An Introduction to OPN 23 2.2 The Structure of OPN 23 2.3 OPN, Integrins and Survival Signaling 25 2.4 OPN and Ischemic Injury 27 2.5 Preclinical Development of OPN 33 2.6 Optimizing Delivery 33 2 2.7 Improving the Potency of OPN 36 2.8 Identifying the Regions of OPN required for Neuroprotection 36 2.9 Hypothesis 37 2.10 Research Design 38 2.11 OPN has neuroprotective capability in vivo and in vitro 40 2.12 The mechanism of neuroprotection by OPN 51 2.13 OPN can be delivered to the brain by intranasal administration 56 2.14 Enhancing the neuroprotective capability of OPN 60 2.15 Peptides based on the N and C terminal fragment of thrombin cleaved OPN are neuroprotective 65 2.16 The C terminal peptide requires phosphorylation to be neuroprotective while the N terminal peptide does not require phosphorylation 70 2.17 Dose response and time window of NT 124-153 71 2.18