Chapter 1: Stroke and Neuroprotection 1 – 21
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

WO 2017/145013 Al 31 August 2017 (31.08.2017) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2017/145013 Al 31 August 2017 (31.08.2017) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C07D 498/04 (2006.01) A61K 31/5365 (2006.01) kind of national protection available): AE, AG, AL, AM, C07D 519/00 (2006.01) A61P 25/00 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, (21) Number: International Application DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/IB20 17/050844 HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KH, KN, (22) International Filing Date: KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, 15 February 2017 (15.02.2017) MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, (25) Filing Language: English RU, RW, SA, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, (26) Publication Language: English TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 62/298,657 23 February 2016 (23.02.2016) US (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant: PFIZER INC. [US/US]; 235 East 42nd Street, GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, New York, New York 10017 (US). -
Noninvasive Evaluation of Myocardial Ischemia and Left Ventricular Function
Linköping University Medical Dissertations No. 1109 Noninvasive Evaluation of Myocardial Ischemia and Left Ventricular Function Eva Maret Division of Cardiovascular Medicine Department of Medical and Health Sciences Linköping University, Sweden Linköping 2009 Eva Maret, 2009 Cover picture/illustration: William Björklund Published articles have been reprinted with the permission of the copyright holder. Printed in Sweden by LiU-Tryck, Linköping, Sweden, 2009 ISBN 978-91-7393-675-0 ISSN 0345-0082 To Martin and John! Somewhere over the rainbow Way up high, There's a land that I heard of Once in a lullaby. Somewhere over the rainbow Skies are blue, And the dreams that you dare to dream Really do come true. From “The Wizard of OZ”, music by Harold Arlen and lyrics by E.Y. Harburg CONTENTS POPULÄRVETENSKAPLIG SAMMANFATTNING ................................................................ 7 LIST OF PUBLICATIONS .......................................................................................................... 9 INTRODUCTION ....................................................................................................................... 13 Coronary Artery Disease ........................................................................................................ 13 Coronary flow, resistance and flow reserve ........................................................................... 14 Coronary atherosclerosis and myocardial infarction .............................................................. 15 Left ventricular function -

(12) United States Patent (10) Patent N0.: US 7,964,607 B2 Verhoest Et A1
US007964607B2 (12) United States Patent (10) Patent N0.: US 7,964,607 B2 Verhoest et a1. (45) Date of Patent: Jun. 21, 2011 (54) PYRAZOLO[3,4-D]PYRIMIDINE FOREIGN PATENT DOCUMENTS COMPOUNDS EP 1460077 9/2004 WO 02085904 10/2002 (75) Inventors: Patrick Robert Verhoest, Old Lyme, CT WO 2004037176 5/2004 (US); Caroline ProulX-Lafrance, Ledyard, CT (US) OTHER PUBLICATIONS Wunder et a1, M01. PharmacoL, v01. 28, N0. 6, (2005), pp. 1776 (73) Assignee: P?zer Inc., New York, NY (U S) 1781. van der Staay et a1, Neuropharmacology, v01. 55 (2008), pp. 908 ( * ) Notice: Subject to any disclaimer, the term of this 918. patent is extended or adjusted under 35 USC 154(b) by 562 days. Primary Examiner * Susanna Moore (74) Attorney, Agent, or Firm * Jennifer A. Kispert; (21) Appl.No.: 12/118,062 Michael Herman (22) Filed: May 9, 2008 (57) ABSTRACT (65) Prior Publication Data The invention provides PDE9-inhibiting compounds of For US 2009/0030003 A1 Jan. 29, 2009 mula (I), Related US. Application Data (60) Provisional application No. 60/917,333, ?led on May 11, 2007. (51) Int. Cl. C07D 48 7/04 (2006.01) A61K 31/519 (2006.01) A61P 25/28 (2006.01) (52) US. Cl. ................................... .. 514/262.1; 544/262 (58) Field of Classi?cation Search ................ .. 544/262; 5 1 4/2 62 .1 See application ?le for complete search history. and pharmaceutically acceptable salts thereof, Wherein R, R1, (56) References Cited R2 and R3 are as de?ned herein. Pharmaceutical compositions containing the compounds of Formula I, and uses thereof in U.S. -

Impact of Open Channel Blockers on the Surface Dynamics and Organization of NMDA Receptors Alexandra Fernandes
Impact of open channel blockers on the surface dynamics and organization of NMDA receptors Alexandra Fernandes To cite this version: Alexandra Fernandes. Impact of open channel blockers on the surface dynamics and organization of NMDA receptors. Neurons and Cognition [q-bio.NC]. Université de Bordeaux, 2020. English. NNT : 2020BORD0181. tel-03177416 HAL Id: tel-03177416 https://tel.archives-ouvertes.fr/tel-03177416 Submitted on 23 Mar 2021 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. THÈSE PRÉSENTÉE POUR OBTENIR LE GRADE DE DOCTEUR DE L’UNIVERSITÉ DE BORDEAUX ÉCOLE DOCTORALE Sciences de la Vie et de la Santé SPÉCIALITÉ Neurosciences Par Alexandra FERNANDES Impact of open channel blockers on the surface dynamics and organization of NMDA receptors Sous la direction de Julien DUPUIS Soutenue le 10 Novembre 2020 Membres du jury : Mme SANS, Nathalie Directeur de recherche INSERM Président M. DE KONINCK, Paul Professeur, University of Laval Rapporteur Mme LÉVI, Sabine Directeur de recherche CNRS Rapporteur Mme CARVALHO, Ana Luísa Professeur, University of Coimbra Examinateur M. DUPUIS, Julien Chargé de recherche INSERM Directeur THÈSE PRÉSENTÉE POUR OBTENIR LE GRADE DE DOCTEUR DE L’UNIVERSITÉ DE BORDEAUX ÉCOLE DOCTORALE Sciences de la Vie et de la Santé SPÉCIALITÉ Neurosciences Par Alexandra FERNANDES Impact des bloqueurs de canal ouvert sur la dynamique et l’organisation de surface des récepteurs NMDA Sous la direction de Julien DUPUIS Soutenue le 10 Novembre 2020 Membres du jury : Mme SANS, Nathalie Directeur de recherche INSERM Président M. -

College Catalog 2011–2012
1 College Catalog 2011–2012 - BOSTON | WORCESTER | MANCHESTER, NH This catalog is intended to provide working guidelines and descriptions of the general and academic policies of the College applicable to students. It is not intended and cannot be Massachusetts College of Pharmacy and Health Sciences construed as a contract or guaranty of any kind, express or implied, and the College may 179 Longwood Avenue, Boston, Massachusetts 02115 change, delete or add to these guidelines unilaterally in its sole discretion and without notice. The College also reserves the right to determine the applicability of any policy to a particular Telephone 617.732.2800; students outside Massachusetts and within the continental United situation or set of circumstances and to depart from the guidelines contained herein in States may call toll free 1.800.225.5506. Non-Discrimination Policy a given case. This catalog supersedes any previous catalog, policies or practices relating It is the policy and commitment of Massachusetts College of Pharmacy and Health Sciences 2 to students. It is the responsibility of the students to know and understand the College’s 3 not to discriminate on the basis of race, religion, color, age, sexual orientation, sex, sexual policies. The College may from time to time acquire or develop new programs, or expand its identity, disability, veteran status, marital status or national origin in its educational pro- offerings in other locations, including distance learning programs, and the guidelines in this grams, activities, admissions or employment policies and to actively comply with the require- ments of Federal Executive Orders 11246 and 11375 as amended; the Civil Rights Act of catalog shall apply to all such programs and locations. -
Ischemia and Reperfusion Injury: When Cells Almost Die
Peer Reviewed CE Article #1 Ischemia and Reperfusion Injury: When Cells Almost Die Amy N. Breton, CVT, VTS (ECC) Veterinary Emergency and Specialty Center of New England Waltham, Massachusetts schemia is defined as inadequate blood supply to a part ing energy for metabolism within cells.3 One of the fastest of the body, usually caused by partial or total block- ways that ATP is produced is by oxidative phosphorylation, age of an artery. Reperfusion injury occurs when tissue which, as the name implies, requires oxygen.3 Despite the I 3 perfusion and oxygenation are restored to an area that has importance of ATP, cells do not stockpile ATP. They only been affected by an ischemic event. make what they need for a particular time. When ischemia Ischemia/reperfusion (I/R) injury is a complex cascade occurs, oxygenation of cells ceases, resulting in anaerobic of events resulting in devastating effects on the body, ATP production, which is less efficient.3 sometimes including death. Despite more than 70 years of When oxygen becomes unavailable, cells begin anaero- research, I/R injury is not fully understood. Events such as bic glycolysis. This process can be a lifesaving way for cells gastric dilatation–volvulus (GDV), mesenteric torsion, or to obtain energy; however, it is extremely wasteful. During strangulation of a limb can lead to I/R injury. It is important anaerobic glycolysis, pyruvic acid and hydrogen atoms for all veterinary personnel to understand I/R injury so that combine with nicotinamide adenine dinucleotide (NAD) treatment and prevention can begin as early as possible. to form NADH and H+.3 If the buildup of NADH and H+ within cells becomes too great, the anaerobic process stops, The Ischemic Cascade terminating energy production.3 However, NADH and H+ The chain of events involved in I/R injury can be broken combine to form lactic acid, which diffuses from cells rap- down into the ischemic cascade (BOX 1) and reperfusion idly so that the process can continue.3 Although this is not injury (BOX 2). -

Neu2000, an NR2B-Selective, Moderate NMDA Receptor
Drug News & Perspectives 2010, 23(9): 549-556 THOMSON REUTERS LOOKING AHEAD Targeting both NMDA receptors and free NEU2000, AN NR2B-SELECTIVE, radicals may provide MODERATE NMDA RECEPTOR enhanced ANTAGONIST AND POTENT SPIN neuroprotection against TRAPPING MOLECULE FOR hypoxic-ischemic injury. STROKE confer substantial neuroprotection in ani- by Sung Ig Cho, Ui Jin Park, mal models of stroke have failed to show SUMMARY Jun-Mo Chung and Byoung Joo Gwag beneficial effects in clinical trials for stroke. Excess activation of ionotropic gluta- Free radicals mediate an additional route of mate receptors, primarily N-methyl-D- Stroke is a cerebrovascular injury caused by neuronal cell death after ischemia and aspartate (NMDA) receptors and free the interruption of blood flow to the brain reperfusion. Several antioxidants have radicals, evoke nerve cell death follow- due to thrombosis, embolic particles or advanced to clinical trials including edar- ing hypoxic-ischemic brain injury in var- blood vessel bursts. Stroke is the leading avone, a hydroxyl radical scavenger that has ious animal models. However, clinical cause of serious, long-term disability in shown beneficial effects in patients with trials in stroke patients using NMDA adults and the second leading cause of transient ischemia and which was approved receptor antagonists have failed to death in the U.S. and Europe (1). Rates of as a neuroprotective drug in Japan and show efficacy primarily due to the limit- stroke mortality and burden are more China. ed therapeutic time window for neuro- affected in low-income countries including protection and a narrow therapeutic NMDA receptor antagonists and antioxi- eastern Europe, northern Asia and central index. -

Ep 2932971 A1
(19) TZZ ¥ __T (11) EP 2 932 971 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 21.10.2015 Bulletin 2015/43 A61K 31/54 (2006.01) A61K 31/445 (2006.01) A61K 9/08 (2006.01) A61K 9/51 (2006.01) (2006.01) (21) Application number: 15000954.6 A61L 31/00 (22) Date of filing: 06.03.2006 (84) Designated Contracting States: • MCCORMACK, Stephen, Joseph AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Claremont, CA 91711 (US) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI • SCHLOSS, John, Vinton SK TR Valencia, CA 91350 (US) • NAGY, Anna Imola (30) Priority: 04.03.2005 US 658207 P Saugus, CA 91350 (US) • PANANEN, Jacob, E. (62) Document number(s) of the earlier application(s) in 306 Los Angeles, CA 90042 (US) accordance with Art. 76 EPC: 06736872.0 / 1 861 104 (74) Representative: Ali, Suleman et al Avidity IP Limited (71) Applicant: Otonomy, Inc. Broers Building, Hauser Forum San Diego, CA 92121 (US) 21 JJ Thomson Avenue Cambridge CB3 0FA (GB) (72) Inventors: • LOBL, Thomas, Jay Remarks: Valencia, This application was filed on 09-04-2015 as a CA 91355-1995 (US) divisional application to the application mentioned under INID code 62. (54) KETAMINE FORMULATIONS (57) Formulations of ketamine for administration to the inner or middle ear. EP 2 932 971 A1 Printed by Jouve, 75001 PARIS (FR) EP 2 932 971 A1 Description [0001] This application claims the benefit of Serial No. 60/658,207 filed March 4, 2005. -

Possible Protective Effect Or Harmful of Ketamine on Isquemia-Induced Acute Kidney Injury in a Pediatric Murine Model
Open Access Austin Journal of Anesthesia and Analgesia Special Article - Pediatric Anesthesiology Possible Protective Effect or Harmful of Ketamine on Isquemia-Induced Acute Kidney Injury in a Pediatric Murine Model Acosta-Murillo NR and Dueñas Gómez Z* Department of Physiological Sciences, National Abstract University of Colombia, Colombia The association between Ketamine and renal function begins in animal *Corresponding author: Dueñas Gómez Z, models, since the 1970s, particularly in relation to the effects on renal blood Department of Physiological Sciences, Division of flow [1,2]. Factors on renal hemodynamics such as decreased cardiac output Physiology, National University of Colombia, Bogotá, and blood pressure, sympathetic nerve stimulation and catecholamine release Colombia and, increased renin, angiotensin and vasopressin were involved [3]. From this century, the presence of N-Methyl-D-Aspartate Receptors (NMDA-R) outside Received: April 26, 2016; Accepted: June 01, 2016; the Central Nervous System (CNS) [4] where they had been initially identified Published: June 06, 2016 has been proposed, whereby the existence of the NMDA-R in the kidney and its functional role becomes important [5,6] in this way, the possible effects of NMDA-R antagonists, such as ketamine. Keywords: L-Glutamate; NMDA receptors; Renal function, Ketamine; Acute kidney injury; Ischemia/Reperfusion Abbreviations Α-Amino-3-Hydroxy-5-Methyl-4-Isoxazole Propionic Acid (AMPA) receptor [8,9]. NMDA-R is large heterotetrameric membrane protein L-Glu: L-Glutamate; NMDA-R: N-Methyl-D-Aspartate complexes with a high permeability to calcium, which triggers a series Receptors; iGluRs: Ionotropic Glutamate Receptors; mGluRs: of calcium mediated intracellular events that have an outstanding Metabotropic Glutamate Receptors; AMPA: Α-Amino-3-Hydroxy- role in many physiological and pathological processes. -

( 12 ) United States Patent
US009737531B2 (12 ) United States Patent ( 10 ) Patent No. : US 9 , 737 ,531 B2 Javitt ( 45) Date of Patent : Aug . 22 , 2017 ( 54 ) COMPOSITION AND METHOD FOR 2008 /0194698 A1 * 8 / 2008 Hermanussen et al. .. .. 514 /662 TREATMENT OF DEPRESSION AND 2011/ 0207776 A18 / 2011 Buntinx 2011 /0306586 Al 12 / 2011 Khan PSYCHOSIS IN HUMANS 2012 /0041026 A12 / 2012 Waizumi (71 ) Applicant : Daniel C Javitt , Bardonia , NY (US ) FOREIGN PATENT DOCUMENTS ( 72 ) Inventor: Daniel C Javitt, Bardonia , NY (US ) CN 101090721 12 / 2007 KR 2007 0017136 A 2 / 2007 ( 73 ) Assignee : GLYTECH , LLC , Ft. Lee, NJ (US ) WO WO 2005 /000216 A2 1 / 2005 WO WO 2005 /065308 A2 7 / 2005 ( * ) Notice : Subject to any disclaimer , the term of this WO WO 2005 /079756 9 / 2005 patent is extended or adjusted under 35 WO 2011044089 4 / 2011 U . S . C . 154 ( b ) by 0 days . wo WO 2012 / 104852 Al 8 / 2012 ( 21 ) Appl. No. : 13 /936 , 198 OTHER PUBLICATIONS Ceglia et al. , “ The 5 -HT2A receptor antagonist M100 , 907 prevents ( 22 ) Filed : Jul. 7 , 2013 extracellular glutamate rising in response to NMDA receptor block ade in the mPFC ,” Journal of Neurochemistry , 2004 , 91 , 189 - 199 . * ((65 65 ) Prior Publication Data Mony et al. , “ Identification of a novel NR2B -selective NMDA US 2014 / 0018348 A1 Jan . 16 , 2014 receptor antagonist using a virtual screening approach , ” Bioorganic & Medicinal Chemistry Letters 20 ( 2010 ) 5552 - 5558 . * Ceglia et al ., “ The 5HT2A receptor antagonist M100 , 907 prevents Related U . S . Application Data extracellular glutamate rising in response to NMDA receptor block ( 60 ) Provisional application No . -
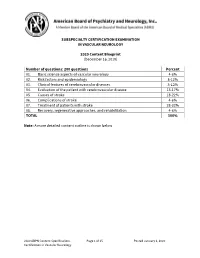
2020 Vascular Neurology CERT Content Specifications
SUBSPECIALTY CERTIFICATION EXAMINATION IN VASCULAR NEUROLOGY 2020 Content Blueprint (December 16, 2019) Number of questions: 200 questions Percent 01. Basic science aspects of vascular neurology 4-6% 02. Risk factors and epidemiology 8-12% 03. Clinical features of cerebrovascular diseases 8-12% 04. Evaluation of the patient with cerebrovascular disease 13-17% 05. Causes of stroke 18-22% 06. Complications of stroke 4-6% 07. Treatment of patients with stroke 28-32% 08. Recovery, regenerative approaches, and rehabilitation 4-6% TOTAL 100% Note: A more detailed content outline is shown below 2020 ABPN Content Specifications Page 1 of 15 Posted January 6, 2020 Certification in Vascular Neurology SUBSPECIALTY CERTIFICATION EXAMINATION IN VASCULAR NEUROLOGY 2020 Content Outline Content Areas 01. Basic science aspects of vascular neurology A. Vascular neuroanatomy 1. Extracranial arterial anatomy 2. Intracranial arterial anatomy 3. Collaterals 4. Alterations of vascular anatomy 5. Venous anatomy 6. Spinal cord vascular anatomy 7. Specific vascular-brain anatomic correlations 8. End vessel syndromes B. Stroke pathophysiology 1. Cerebral blood flow a. Vascular smooth muscle control b. Vasodilation and vasoconstriction c. Autoregulation d. Vasospasm e. Rheology f. Blood flow in stroke 2. Blood-brain barrier in stroke 3. Coagulation cascade a. Clotting factors b. Platelet function c. Endothelium function d. Biochemical factors 4. Metabolic and cellular consequences of ischemia a. Ischemic cascade b. Reperfusion changes c. Electrophysiology d. Gene regulation 5. Inflammation and stroke 6. Brain edema and increased ICP a. Secondary effects 2020 ABPN Content Specifications Page 2 of 15 Posted January 6, 2020 Certification in Vascular Neurology 7. Restoration and recovery following stroke 8. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data.