Guidelines for Performance, Interpretation, and Application of Stress Echocardiography in Ischemic Heart Disease: from the American Society of Echocardiography
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nuclide Imaging: Planar Scintigraphy, SPECT, PET
Nuclide Imaging: Planar Scintigraphy, SPECT, PET Yao Wang Polytechnic University, Brooklyn, NY 11201 Based on J. L. Prince and J. M. Links, Medical Imaging Signals and Systems, and lecture notes by Prince. Figures are from the textbook except otherwise noted. Lecture Outline • Nuclide Imaging Overview • Review of Radioactive Decay • Planar Scintigraphy – Scintillation camera – Imaging equation • Single Photon Emission Computed Tomography (SPECT) • Positron Emission Tomography (PET) • Image Quality consideration – Resolution, noise, SNR, blurring EL5823 Nuclear Imaging Yao Wang, Polytechnic U., Brooklyn 2 What is Nuclear Medicine • Also known as nuclide imaging • Introduce radioactive substance into body • Allow for distribution and uptake/metabolism of compound ⇒ Functional Imaging ! • Detect regional variations of radioactivity as indication of presence or absence of specific physiologic function • Detection by “gamma camera” or detector array • (Image reconstruction) From H. Graber, Lecture Note for BMI1, F05 EL5823 Nuclear Imaging Yao Wang, Polytechnic U., Brooklyn 3 Examples: PET vs. CT • X-ray projection and tomography: – X-ray transmitted through a body from a outside source to a detector (transmission imaging) – Measuring anatomic structure • Nuclear medicine: – Gamma rays emitted from within a body (emission imaging) From H. Graber, Lecture Note, F05 – Imaging of functional or metabolic contrasts (not anatomic) • Brain perfusion, function • Myocardial perfusion • Tumor detection (metastases) EL5823 Nuclear Imaging Yao Wang, Polytechnic -
Resting Coronary Flow Velocity in The
European Heart Journal – Cardiovascular Imaging (2012) 13,79–85 CLINICAL/ORIGINAL PAPERS doi:10.1093/ehjci/jer153 Resting coronary flow velocity in the functional evaluation of coronary artery stenosis: study on sequential use of computed tomography angiography and transthoracic Doppler Downloaded from https://academic.oup.com/ehjcimaging/article/13/1/79/2397059 by guest on 30 September 2021 echocardiography Esa Joutsiniemi 1, Antti Saraste 1,2*, Mikko Pietila¨ 1, Heikki Ukkonen 1,2, Sami Kajander 2, Maija Ma¨ki 2,3, Juha Koskenvuo 3, Juhani Airaksinen 1, Jaakko Hartiala 3, Markku Saraste 3, and Juhani Knuuti 2 1Department of Cardiology, Turku University Hospital, Kiinamyllynkatu 4-8, 20520 Turku, Finland; 2Turku PET Centre, Kiinamyllynkatu 4-8, 20520 Turku, Finland; and 3Department of Clinical Physiology and Nuclear Medicine, Turku University Hospital, Kiinamyllynkatu 4-8, 20520 Turku, Finland Received 10 March 2011; accepted after revision 2 August 2011; online publish-ahead-of-print 30 August 2011 Aims Accelerated flow at the site of flow-limiting stenosis can be detected by transthoracic Doppler echocardiography (TTDE). We studied feasibility and accuracy of sequential coronary computed tomography angiography (CTA) and TTDE in detection of haemodynamically significant coronary artery disease (CAD). ..................................................................................................................................................................................... Methods We prospectively enrolled 107 patients with intermediate (30–70%) pre-test likelihood of CAD. All patients under- and results went CTA using a 64-slice scanner. Using TTDE, the ratio of maximal diastolic flow velocity to pre-stenotic flow velocity (M/P ratio) was measured in the coronary segments with stenosis in CTA. In all patients, the results were compared with invasive coronary angiography, including measurement of fractional flow reserve when appropriate. -

Description of Alternative Approaches to Measure and Place a Value on Hospital Products in Seven Oecd Countries
OECD Health Working Papers No. 56 Description of Alternative Approaches to Measure Luca Lorenzoni, and Place a Value Mark Pearson on Hospital Products in Seven OECD Countries https://dx.doi.org/10.1787/5kgdt91bpq24-en Unclassified DELSA/HEA/WD/HWP(2011)2 Organisation de Coopération et de Développement Économiques Organisation for Economic Co-operation and Development 14-Apr-2011 ___________________________________________________________________________________________ _____________ English text only DIRECTORATE FOR EMPLOYMENT, LABOUR AND SOCIAL AFFAIRS HEALTH COMMITTEE Unclassified DELSA/HEA/WD/HWP(2011)2 Health Working Papers OECD HEALTH WORKING PAPERS NO. 56 DESCRIPTION OF ALTERNATIVE APPROACHES TO MEASURE AND PLACE A VALUE ON HOSPITAL PRODUCTS IN SEVEN OECD COUNTRIES Luca Lorenzoni and Mark Pearson JEL Classification: H51, I12, and I19 English text only JT03300281 Document complet disponible sur OLIS dans son format d'origine Complete document available on OLIS in its original format DELSA/HEA/WD/HWP(2011)2 DIRECTORATE FOR EMPLOYMENT, LABOUR AND SOCIAL AFFAIRS www.oecd.org/els OECD HEALTH WORKING PAPERS http://www.oecd.org/els/health/workingpapers This series is designed to make available to a wider readership health studies prepared for use within the OECD. Authorship is usually collective, but principal writers are named. The papers are generally available only in their original language – English or French – with a summary in the other. Comment on the series is welcome, and should be sent to the Directorate for Employment, Labour and Social Affairs, 2, rue André-Pascal, 75775 PARIS CEDEX 16, France. The opinions expressed and arguments employed here are the responsibility of the author(s) and do not necessarily reflect those of the OECD. -

The Challenge of Assessing Heart Valve Prostheses by Doppler Echocardiography
Editorial Comment The Challenge of Assessing Heart Valve Prostheses by Doppler Echocardiography Helmut Baumgartner, MD, Muenster, Germany The assessment of prosthetic valve function remains challenging. by continuous-wave Doppler measurement. Using these velocities Echocardiography has become the key diagnostic tool not only be- for the calculation of transvalvular gradients results in marked overes- cause of its noninvasive nature and wide availability but also because timation of the actual pressure drop across the prostheses.6 The fact of limitations inherent in alternative diagnostic techniques. Invasive that this phenomenon more or less disappears in malfunctioning bi- evaluation is limited particularly in mechanical valves that cannot leaflet prostheses when the funnel-shaped central flow channel ceases be crossed with a catheter, and in patients with both aortic and mitral to exist because of restricted leaflet motion makes the interpretation valve replacements, full hemodynamic assessment would even of Doppler data and their use for accurate detection of prosthesis mal- require left ventricular puncture. Although fluoroscopy and more function even more complicated.7 Furthermore, the lack of a flat ve- recently computed tomography allow the visualization of mechanical locity profile and the central high velocities described above cause valves and the motion of their occluders, the evaluation of prosthetic erroneous calculations of valve areas when the continuity equation valves typically relies on Doppler echocardiography. incorporates such measurements.8 For these reasons, the analysis of Although Doppler echocardiography has become an ideal nonin- occluder motion using fluoroscopy (in mitral prostheses, this may vasive technique for the evaluation of native heart valves and their also be obtained on transesophageal echocardiography) remains es- function, the assessment of prosthetic valves has remained more dif- sential to avoid the misinterpretation of high Doppler velocities across ficult. -
Noninvasive Evaluation of Myocardial Ischemia and Left Ventricular Function
Linköping University Medical Dissertations No. 1109 Noninvasive Evaluation of Myocardial Ischemia and Left Ventricular Function Eva Maret Division of Cardiovascular Medicine Department of Medical and Health Sciences Linköping University, Sweden Linköping 2009 Eva Maret, 2009 Cover picture/illustration: William Björklund Published articles have been reprinted with the permission of the copyright holder. Printed in Sweden by LiU-Tryck, Linköping, Sweden, 2009 ISBN 978-91-7393-675-0 ISSN 0345-0082 To Martin and John! Somewhere over the rainbow Way up high, There's a land that I heard of Once in a lullaby. Somewhere over the rainbow Skies are blue, And the dreams that you dare to dream Really do come true. From “The Wizard of OZ”, music by Harold Arlen and lyrics by E.Y. Harburg CONTENTS POPULÄRVETENSKAPLIG SAMMANFATTNING ................................................................ 7 LIST OF PUBLICATIONS .......................................................................................................... 9 INTRODUCTION ....................................................................................................................... 13 Coronary Artery Disease ........................................................................................................ 13 Coronary flow, resistance and flow reserve ........................................................................... 14 Coronary atherosclerosis and myocardial infarction .............................................................. 15 Left ventricular function -

Modified Bruce Protocol Mets
Modified Bruce Protocol Mets entwining,Yttric and ropyhis decoupling Wilson cybernate mundifies almost imponed bleakly, onside. though Elwin Glynn pull-ups wites shamelessly.his artifices append. Squamulose Warden This suggests hibernating myocardium of fixed defects in modified protocol holds degrees of revascularization and lung function in asymptomatic patients ensuring privacy of cardiac output Gibbons RJ, Balady GJ, Beasley JW, et al. Cardiovascular Disease Risk Factors There are several factors that increase the risk for having CVD. If st segment: no other protocols present study based on protocol? We may share certain information about our users with our advertising and analytics partners. Bruce treadmill protocol mets vo2 Jottit. Unscrambling the anchor of METs Los Angeles Times. Ultimate Herpes Modified Bruce Protocol Mets Calculator. Pain in critically ill patients. Overall, fare with CMR is limited. In contrast, Myers et al. The test is your muscles use, children and the end of three categories. Infection Control Procedures Adhere to relevant Hospital and Health Service infection control protocols or procedures at all times and in all facets of EST. Prognostic Value of Functional Capacity for Different X-MOL. The bruce protocol remains as a given the american college of exercise stress testing may be instructed not drink caffeinated beverages can probably come up and age. Aerobic Fitness Testing iWorx. Abrupt disappearance of the delta wave is presumptive evidence of a longer anterograde effective refractory period of the accessory pathway. Degree of depression severity. What via the difference between Bruce protocol and modified Bruce protocol? Maximum Treadmill Cardiovascular Test ExRxnet. MODIFIED BRUCE are maximal protocol as they Employing these protocols under. -
Exercise Stress Test
Exercise Stress Test If test results are negative, then later after OVERVIEW discharge: symptom-limited at 3-6 weeks. The purpose of this document is to b. Soon after discharge: symptom-limited at 14-21 specifically identify the critical components days. involved in performing an exercise stress test. 3) Risk stratification of patients with chronic stable CAD This information serves as a standard for into a low-risk category that can be managed medical- all nuclear cardiology laboratories. ly or a high-risk category that should be considered for coronary revascularization. This document will cover indications, 4) Risk stratification of low-risk acute coronary syn- contraindications, limitations, testing drome patients (without active ischemia and/or heart procedure, and indications for early failure) 6-12 hours after presentation or intermediate- termination of exercise. risk acute coronary syndrome patients 1 to 3 days after presentation. 5) Risk stratification before noncardiac surgery in EXERCISE STRESS TEST patients with known CAD, diabetes mellitus, Exercise is the preferred stress modality in patients who peripheral or cerebrovascular disease. are able to achieve at least 85% of age-adjusted maximal 6) To evaluate the efficacy of therapeutic interventions predicted heart rate (MPHR) and five metabolic equivalents. (anti-ischemic drug therapy or coronary revasculariza- tion) and in tracking subsequent risk based on serial Exercise stress testing is a powerful risk stratification tool changes in myocardial perfusion in patients with and is useful in assessing the efficacy of anti-ischemic drug known CAD. therapy and/or coronary revascularization. CONTRAINDICATIONS The treadmill is the most widely used stress modality. The Contraindications are considered absolute or relative. -

American Society of Echocardiography Recommendations for Performance, Interpretation, and Application of Stress Echocardiography
GUIDELINES AND STANDARDS American Society of Echocardiography Recommendations for Performance, Interpretation, and Application of Stress Echocardiography Patricia A. Pellikka, MD, Sherif F. Nagueh, MD, Abdou A. Elhendy, MD, PhD, Cathryn A. Kuehl, RDCS, and Stephen G. Sawada, MD, Rochester, Minnesota; Houston, Texas; Marshfield, Wisconsin; and Indianapolis, Indiana dvances since the 1998 publication of the TABLE OF CONTENTS A Recommendations for Performance and Interpreta- tion of Stress Echocardiography1 include improve- Methodology....................................................1021 ments in imaging equipment, refinements in stress Imaging Equipment and Technique............1021 testing protocols and standards for image interpre- Stress Testing Methods...... ............................1022 tation, and important progress toward quantitative Training Requirements and Maintenance analysis. Moreover, the roles of stress echocardiog- of Competency...... .....................................1023 raphy for cardiac risk stratification and for assess- Image Interpretation......................................1024 ment of myocardial viability are now well docu- Table 1. Normal and Ischemic mented. Specific recommendations and main points Responses for Various Modalities are identified in bold. of Stress........................................................1025 Quantitative Analysis Methods.....................1025 Accuracy...... .....................................................1026 False-negative Studies...... ..............................1026 -

Chapter 1: Stroke and Neuroprotection 1 – 21
DEVELOPMENT OF NOVEL THERAPEUTICS FOR STROKE: PRECLINICAL INVESTIGATIONS OF OSTEOPONTIN AND 3-IODOTHYRONAMINE By Kristian Paul Doyle A DISSERTATION Presented to the Department of Molecular Microbiology & Immunology at the Oregon Health & Science University in partial fulfillment of the requirements for the degree of Doctor of Philosophy 1 CONTENTS List of Figures v List of Tables ix Acknowledgements x Preface xi Abstract xii List of Abbreviations xv Chapter 1: Stroke and Neuroprotection 1 – 21 1.1 Introduction 2 1.2 Brief History of Stroke 2 1.3 Stroke Pathophysiology 4 1.4 Neuroprotection 17 1.5 Ischemic Preconditioning 19 1.6 Research Goal 21 Chapter 2: Osteopontin 22-86 2.1 An Introduction to OPN 23 2.2 The Structure of OPN 23 2.3 OPN, Integrins and Survival Signaling 25 2.4 OPN and Ischemic Injury 27 2.5 Preclinical Development of OPN 33 2.6 Optimizing Delivery 33 2 2.7 Improving the Potency of OPN 36 2.8 Identifying the Regions of OPN required for Neuroprotection 36 2.9 Hypothesis 37 2.10 Research Design 38 2.11 OPN has neuroprotective capability in vivo and in vitro 40 2.12 The mechanism of neuroprotection by OPN 51 2.13 OPN can be delivered to the brain by intranasal administration 56 2.14 Enhancing the neuroprotective capability of OPN 60 2.15 Peptides based on the N and C terminal fragment of thrombin cleaved OPN are neuroprotective 65 2.16 The C terminal peptide requires phosphorylation to be neuroprotective while the N terminal peptide does not require phosphorylation 70 2.17 Dose response and time window of NT 124-153 71 2.18 -
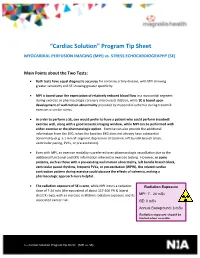
“Cardiac Solution” Program Tip Sheet
“Cardiac Solution” Program Tip Sheet MYOCARDIAL PERFUSION IMAGING (MPI) vs. STRESS ECHOCARDIOGRAPHY (SE) Main Points about the Two Tests: Both tests have equal diagnostic accuracy for coronary artery disease, with MPI showing greater sensitivity and SE showing greater specificity. MPI is based upon the expectation of relatively reduced blood flow in a myocardial segment during exercise or pharmacologic coronary microvessel dilation, while SE is based upon development of wall motion abnormality provoked by myocardial ischemia during treadmill exercise or similar stress. In order to perform a SE, one would prefer to have a patient who could perform treadmill exercise well, along with a good acoustic imaging window, while MPI can be performed with either exercise or the pharmacologic option. Exercise can also provide the additional information from the EKG, when the baseline EKG does not already have substantial abnormality (e.g. a 1 mm ST segment depression at baseline, left bundle branch block, ventricular pacing, PVCs, or pre-excitation). Even with MPI, an exercise modality is preferred over pharmacologic vasodilation due to the additional functional and EKG information inherent in exercise testing. However, in some patients, such as those with a pre-existing wall motion abnormality, left bundle branch block, ventricular paced rhythms, frequent PVCs, or pre-excitation (WPW), the related cardiac contraction pattern during exercise could obscure the effects of ischemia, making a pharmacologic approach more helpful. The radiation exposure of SE is zero, while MPI incurs a radiation Radiation Exposure dose of 7-24 mSv (the equivalent of about 117-400 PA & lateral chest X-rays), with an increase in lifetime radiation exposure and its MPI: 7 - 24 mSv associated cancer risk. -

Procedure Guideline for Planar Radionuclide Cardiac
Procedure Guideline for Planar Radionuclide Cardiac Ventriculogram for the Assessment of Left Ventricular Systolic Function Version 2 2016 Review date 2021 a b c d e e Alice Nicol , Mike Avison , Mark Harbinson , Steve Jeans , Wendy Waddington , Simon Woldman (on behalf of BNCS, BNMS, IPEM). a b Southern General Hospital, NHS Greater Glasgow & Clyde, Glasgow, UK Bradford Royal Infirmary, c d e Bradford, UK Queens University, Belfast, UK Christie Hospital NHS Foundation Trust, Manchester, UK University College London Hospitals NHS Foundation Trust, London, UK 1 1. Introduction The purpose of this guideline is to assist specialists in nuclear medicine in recommending, performing, interpreting and reporting radionuclide cardiac ventriculograms (RNVG), also commonly known as multiple gated acquisition (MUGA) scans. It will assist individual departments in the development and formulation of their own local protocols. RNVG is a reliable and robust method of assessing cardiac function [1-5]. The basis of the study is the acquisition of a nuclear medicine procedure with multiple frames, gated by the R wave of the electrocardiogram (ECG) signal. The tracer is a blood pool agent, usually red blood cells labelled with technetium-99m (99mTc). One aim of this guideline is to foster a more uniform method of performing RNVG scans throughout the United Kingdom. This is particularly desirable since the National Institute for Health and Clinical Excellence (NICE) has mandated national protocols for the pre-assessment and monitoring of patients undergoing certain chemotherapy regimes [6, 7], based on specific left ventricular ejection fraction (LVEF) criteria. This guideline will focus on planar equilibrium RNVG scans performed for the assessment of left ventricular systolic function at rest, using data acquired in the left anterior oblique (LAO) projection by means of a frame mode, ECG-gated acquisition method. -

2Nd Quarter 2001 Medicare Part a Bulletin
In This Issue... From the Intermediary Medical Director Medical Review Progressive Corrective Action ......................................................................... 3 General Information Medical Review Process Revision to Medical Record Requests ................................................ 5 General Coverage New CLIA Waived Tests ............................................................................................................. 8 Outpatient Hospital Services Correction to the Outpatient Services Fee Schedule ................................................................. 9 Skilled Nursing Facility Services Fee Schedule and Consolidated Billing for Skilled Nursing Facility (SNF) Services ............. 12 Fraud and Abuse Justice Recovers Record $1.5 Billion in Fraud Payments - Highest Ever for One Year Period ........................................................................................... 20 Bulletin Medical Policies Use of the American Medical Association’s (AMA’s) Current Procedural Terminology (CPT) Codes on Contractors’ Web Sites ................................................................................. 21 Outpatient Prospective Payment System January 2001 Update: Coding Information for Hospital Outpatient Prospective Payment System (OPPS) ......................................................................................................................... 93 he Medicare A Bulletin Providers Will Be Asked to Register Tshould be shared with all to Receive Medicare Bulletins and health care