Glutathione S‑Transferase Ω 1 Promotes the Proliferation, Migration and Invasion, and Inhibits the Apoptosis of Non‑Small C
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bioinformatics Identification of Potential Genes and Pathways in Preeclampsia Based on Functional Gene Set Enrichment Analyses
EXPERIMENTAL AND THERAPEUTIC MEDICINE 18: 1837-1844, 2019 Bioinformatics identification of potential genes and pathways in preeclampsia based on functional gene set enrichment analyses XUE LI and YANNING FANG Department of Obstetrics, The First People's Hospital of Jining, Jining, Shandong 272000, P.R. China Received October 24, 2018; Accepted May 2, 2019 DOI: 10.3892/etm.2019.7749 Abstract. Preeclampsia is a complication of pregnancy the sample into four distinct groups based on different incu- characterized by new-onset hypertension and proteinuria of bation time. The top 3 candidates were Toll-like receptor 2 gestation, with serious consequences for mother and infant. (TLR2), glutathione S-transferase omega 1 (GSTO1) and Although a vast amount of research has been performed on mitogen-activated protein kinase 13 (MAPK13). TLR2 and the pathogenesis of preeclampsia, the underlying mechanisms associated pathways are known to be closely associated with of this multisystemic disease have remained to be fully eluci- preeclampsia, indirectly demonstrating the applicability of dated. Data were retrieved from Gene Expression Omnibus the analytic process applied. However, the role of GSTO1 and database GSE40182 dataset. After data preprocessing, differ- MAPK13 in preeclampsia has remained poorly investigated, entially expressed genes of placental cells cultured in vitro and elucidation thereof may be a worthwhile endeavor. The from preeclampsia and normal pregnancy were determined present study may provide a basis for exploring potential novel and subjected to Kyoto Encyclopedia of Genes and Genomes genes and pathways as therapeutic targets for preeclampsia. (KEGG) enrichment analysis to identify the associated path- ways. Furthermore, functional principal component analysis Introduction (FPCA) was used to calculate the corresponding F-value of each gene. -

Chuanxiong Rhizoma Compound on HIF-VEGF Pathway and Cerebral Ischemia-Reperfusion Injury’S Biological Network Based on Systematic Pharmacology
ORIGINAL RESEARCH published: 25 June 2021 doi: 10.3389/fphar.2021.601846 Exploring the Regulatory Mechanism of Hedysarum Multijugum Maxim.-Chuanxiong Rhizoma Compound on HIF-VEGF Pathway and Cerebral Ischemia-Reperfusion Injury’s Biological Network Based on Systematic Pharmacology Kailin Yang 1†, Liuting Zeng 1†, Anqi Ge 2†, Yi Chen 1†, Shanshan Wang 1†, Xiaofei Zhu 1,3† and Jinwen Ge 1,4* Edited by: 1 Takashi Sato, Key Laboratory of Hunan Province for Integrated Traditional Chinese and Western Medicine on Prevention and Treatment of 2 Tokyo University of Pharmacy and Life Cardio-Cerebral Diseases, Hunan University of Chinese Medicine, Changsha, China, Galactophore Department, The First 3 Sciences, Japan Hospital of Hunan University of Chinese Medicine, Changsha, China, School of Graduate, Central South University, Changsha, China, 4Shaoyang University, Shaoyang, China Reviewed by: Hui Zhao, Capital Medical University, China Background: Clinical research found that Hedysarum Multijugum Maxim.-Chuanxiong Maria Luisa Del Moral, fi University of Jaén, Spain Rhizoma Compound (HCC) has de nite curative effect on cerebral ischemic diseases, *Correspondence: such as ischemic stroke and cerebral ischemia-reperfusion injury (CIR). However, its Jinwen Ge mechanism for treating cerebral ischemia is still not fully explained. [email protected] †These authors share first authorship Methods: The traditional Chinese medicine related database were utilized to obtain the components of HCC. The Pharmmapper were used to predict HCC’s potential targets. Specialty section: The CIR genes were obtained from Genecards and OMIM and the protein-protein This article was submitted to interaction (PPI) data of HCC’s targets and IS genes were obtained from String Ethnopharmacology, a section of the journal database. -

Genomic Profiling of Short- and Long-Term Caloric Restriction Effects in the Liver of Aging Mice
Genomic profiling of short- and long-term caloric restriction effects in the liver of aging mice Shelley X. Cao, Joseph M. Dhahbi, Patricia L. Mote, and Stephen R. Spindler* Department of Biochemistry, University of California, Riverside, CA 92521 Edited by Bruce N. Ames, University of California, Berkeley, CA, and approved July 11, 2001 (received for review June 19, 2001) We present genome-wide microarray expression analysis of 11,000 aging and CR on gene expression. Control young (7-month-old; n ϭ genes in an aging potentially mitotic tissue, the liver. This organ has 3) and old (27-month-old; n ϭ 3) mice were fed 95 kcal of a a major impact on health and homeostasis during aging. The effects semipurified control diet (Harlan Teklad, Madison, WI; no. of life- and health-span-extending caloric restriction (CR) on gene TD94145) per week after weaning. Long-term CR (LT-CR) young expression among young and old mice and between long-term CR (7-month-old; n ϭ 3) and old (27-month-old; n ϭ 3) mice were fed (LT-CR) and short-term CR (ST-CR) were examined. This experimental 53 kcal of a semipurified CR diet (Harlan Teklad; no. TD94146) per design allowed us to accurately distinguish the effects of aging from week after weaning. Short-term CR (ST-CR) mice were 34-month- those of CR on gene expression. Aging was accompanied by changes old control mice that were switched to 80 kcal of CR diet for 2 in gene expression associated with increased inflammation, cellular weeks, followed by 53 kcal for 2 weeks (n ϭ 3). -

Deletion of Glutathione S-Transferase Omega 1 Activates Type I Interferon Genes and Downregulates Tissue Factor
Published OnlineFirst June 22, 2020; DOI: 10.1158/0008-5472.CAN-20-0530 CANCER RESEARCH | TUMOR BIOLOGY AND IMMUNOLOGY Deletion of Glutathione S-Transferase Omega 1 Activates Type I Interferon Genes and Downregulates Tissue Factor A C Yibin Xu1,2, Armand Bankhead III2,3, Xiaoli Tian1,2, Jianming Tang1,2, Mats Ljungman2,4,5, and Nouri Neamati1,2 ABSTRACT ◥ GST omega 1 (GSTO1) is an atypical GST isoform that is tion of GSTO1. Transcription and protein expression of tissue overexpressed in several cancers and has been implicated in drug factor (gene name, F3) were downregulated in response to resistance. Currently, no small-molecule drug targeting GSTO1 is GSTO1 KO. F3 is associated with poor patient survival and under clinical development. Here we have validated GSTO1 as an promotion of tumor progression in multiple cancers and is a impactful target in oncology. Transcriptional profiling coupled known risk factor for metastasis. Transcription of F3 was reg- with proteomics uncovered novel pharmacodynamic markers ulated by IL1b, whose secretion decreased upon inhibition of and cellular pathways regulated by GSTO1. CRISPR/Cas9 GSTO1, suggesting that IL1b links GSTO1 expression and F3 GSTO1 knockout (KO) cell lines failed to form tumors or transcription. In summary, our results implicate GSTO1 as a displayed growth delay in vivo; they also formed smaller 3D potential therapeutic target in cancer and offer new mechanistic spheroids in vitro. Multiomics analysis in GSTO1 KO cells found insights into its significant role in cancer progression. a strong positive correlation with cell adhesion molecules and IFN response pathways and a strong negative correlation with Significance: These findings validate GSTO1 as a therapeutic Myc transcriptional signature. -

Downloaded Per Proteome Cohort Via the Web- Site Links of Table 1, Also Providing Information on the Deposited Spectral Datasets
www.nature.com/scientificreports OPEN Assessment of a complete and classifed platelet proteome from genome‑wide transcripts of human platelets and megakaryocytes covering platelet functions Jingnan Huang1,2*, Frauke Swieringa1,2,9, Fiorella A. Solari2,9, Isabella Provenzale1, Luigi Grassi3, Ilaria De Simone1, Constance C. F. M. J. Baaten1,4, Rachel Cavill5, Albert Sickmann2,6,7,9, Mattia Frontini3,8,9 & Johan W. M. Heemskerk1,9* Novel platelet and megakaryocyte transcriptome analysis allows prediction of the full or theoretical proteome of a representative human platelet. Here, we integrated the established platelet proteomes from six cohorts of healthy subjects, encompassing 5.2 k proteins, with two novel genome‑wide transcriptomes (57.8 k mRNAs). For 14.8 k protein‑coding transcripts, we assigned the proteins to 21 UniProt‑based classes, based on their preferential intracellular localization and presumed function. This classifed transcriptome‑proteome profle of platelets revealed: (i) Absence of 37.2 k genome‑ wide transcripts. (ii) High quantitative similarity of platelet and megakaryocyte transcriptomes (R = 0.75) for 14.8 k protein‑coding genes, but not for 3.8 k RNA genes or 1.9 k pseudogenes (R = 0.43–0.54), suggesting redistribution of mRNAs upon platelet shedding from megakaryocytes. (iii) Copy numbers of 3.5 k proteins that were restricted in size by the corresponding transcript levels (iv) Near complete coverage of identifed proteins in the relevant transcriptome (log2fpkm > 0.20) except for plasma‑derived secretory proteins, pointing to adhesion and uptake of such proteins. (v) Underrepresentation in the identifed proteome of nuclear‑related, membrane and signaling proteins, as well proteins with low‑level transcripts. -

Common Marker Genes Identified from Various Sample Types for Systemic Lupus Erythematosus
RESEARCH ARTICLE Common Marker Genes Identified from Various Sample Types for Systemic Lupus Erythematosus Peng-Fei Bing1,2☯, Wei Xia1,2☯, Lan Wang1,2, Yong-Hong Zhang2, Shu-Feng Lei1,2, Fei- Yan Deng1,2* 1 Center for Genetic Epidemiology and Genomics, School of Public Health, Soochow University, Suzhou, Jiangsu 215123, P. R. China, 2 Jiangsu Key Laboratory of Preventive and Translational Medicine for Geriatric Diseases, School of Public Health, Soochow University, Suzhou, Jiangsu 215123, P. R. China a11111 ☯ These authors contributed equally to this work. * [email protected] Abstract OPEN ACCESS Citation: Bing P-F, Xia W, Wang L, Zhang Y-H, Lei S- F, Deng F-Y (2016) Common Marker Genes Objective Identified from Various Sample Types for Systemic Systemic lupus erythematosus (SLE) is a complex auto-immune disease. Gene expression Lupus Erythematosus. PLoS ONE 11(6): e0156234. doi:10.1371/journal.pone.0156234 studies have been conducted to identify SLE-related genes in various types of samples. It is unknown whether there are common marker genes significant for SLE but independent of Editor: Jagadeesh Bayry, Institut National de la Santé et de la Recherche Médicale (INSERM), sample types, which may have potentials for follow-up translational research. The aim of FRANCE this study is to identify common marker genes across various sample types for SLE. Received: December 11, 2015 Accepted: May 11, 2016 Methods Published: June 3, 2016 Based on four public microarray gene expression datasets for SLE covering three represen- Copyright: © 2016 Bing et al. This is an open access tative types of blood-born samples (monocyte; peripheral blood mononuclear cell, PBMC; article distributed under the terms of the Creative whole blood), we utilized three statistics (fold-change, FC; t-test p value; false discovery Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any rate adjusted p value) to scrutinize genes simultaneously regulated with SLE across various medium, provided the original author and source are sample types. -
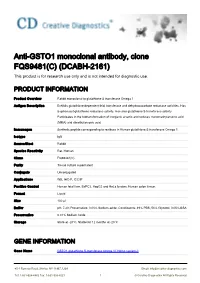
Anti-GSTO1 Monoclonal Antibody, Clone FQS9481(C) (DCABH-2161) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-GSTO1 monoclonal antibody, clone FQS9481(C) (DCABH-2161) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Rabbit monoclonal to glutathione S transferase Omega 1 Antigen Description Exhibits glutathione-dependent thiol transferase and dehydroascorbate reductase activities. Has S-(phenacyl)glutathione reductase activity. Has also glutathione S-transferase activity. Participates in the biotransformation of inorganic arsenic and reduces monomethylarsonic acid (MMA) and dimethylarsonic acid. Immunogen Synthetic peptide corresponding to residues in Human glutathione S transferase Omega 1. Isotype IgG Source/Host Rabbit Species Reactivity Rat, Human Clone FQS9481(C) Purity Tissue culture supernatant Conjugate Unconjugated Applications WB, IHC-P, ICC/IF Positive Control Human fetal liver, BxPC3, HepG2 and HeLa lysates; Human colon tissue. Format Liquid Size 100 μl Buffer pH: 7.20; Preservative: 0.01% Sodium azide; Constituents: 49% PBS, 50% Glycerol, 0.05% BSA Preservative 0.01% Sodium Azide Storage Store at -20°C. Stable for 12 months at -20°C GENE INFORMATION Gene Name GSTO1 glutathione S-transferase omega 1 [ Homo sapiens ] 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved Official Symbol GSTO1 Synonyms GSTO1; glutathione S-transferase omega 1; glutathione S-transferase omega-1; GSTTLp28; P28; GSTO-1; MMA(V) reductase; glutathione-S-transferase like; monomethylarsonic -

Glutathione S-Transferase Omega Genes in Alzheimer and Parkinson
Allen et al. Molecular Neurodegeneration 2012, 7:13 http://www.molecularneurodegeneration.com/content/7/1/13 RESEARCHARTICLE Open Access Glutathione S-transferase omega genes in Alzheimer and Parkinson disease risk, age-at- diagnosis and brain gene expression: an association study with mechanistic implications Mariet Allen1, Fanggeng Zou1, High Seng Chai2, Curtis S Younkin1, Richard Miles1, Asha A Nair2, Julia E Crook3, V Shane Pankratz2, Minerva M Carrasquillo1, Christopher N Rowley1, Thuy Nguyen1,LiMa1, Kimberly G Malphrus1, Gina Bisceglio1, Alexandra I Ortolaza1, Ryan Palusak1, Sumit Middha2, Sooraj Maharjan2, Constantin Georgescu1, Debra Schultz4, Fariborz Rakhshan4, Christopher P Kolbert4, Jin Jen4, Sigrid B Sando5,6, Jan O Aasly5,6, Maria Barcikowska7, Ryan J Uitti8, Zbigniew K Wszolek8, Owen A Ross1, Ronald C Petersen9, Neill R Graff-Radford8, Dennis W Dickson1, Steven G Younkin1 and Nilüfer Ertekin-Taner1,8* Abstract Background: Glutathione S-transferase omega-1 and 2 genes (GSTO1, GSTO2), residing within an Alzheimer and Parkinson disease (AD and PD) linkage region, have diverse functions including mitigation of oxidative stress and may underlie the pathophysiology of both diseases. GSTO polymorphisms were previously reported to associate with risk and age-at-onset of these diseases, although inconsistent follow-up study designs make interpretation of results difficult. We assessed two previously reported SNPs, GSTO1 rs4925 and GSTO2 rs156697, in AD (3,493 ADs vs. 4,617 controls) and PD (678 PDs vs. 712 controls) for association with disease risk (case-controls), age-at-diagnosis (cases) and brain gene expression levels (autopsied subjects). Results: We found that rs156697 minor allele associates with significantly increased risk (odds ratio = 1.14, p = 0.038) in the older ADs with age-at-diagnosis > 80 years. -

Genetic Variation and Gene Expression in Antioxidant Related
Chronic obstructive pulmonary disease Genetic variation and gene expression in antioxidant Thorax: first published as 10.1136/thx.2007.086199 on 19 June 2008. Downloaded from related enzymes and risk of COPD: a systematic review A R Bentley, P Emrani, P A Cassano c Additional Methods and ABSTRACT interindividual differences in the response to Results data are published Background: Observational epidemiological studies of cigarette smoke. online only at http://thorax.bmj. com/content/vol63/issue11 dietary antioxidant intake, serum antioxidant concentra- This review focuses on genes related to anti- tion and lung outcomes suggest that lower levels of oxidant activity, as oxidant-rich cigarette smoke Division of Nutritional Sciences, antioxidant defences are associated with decreased lung Cornell University, Ithaca, New strains the antioxidant defences of the lungs, York, USA function. Another approach to understanding the role of leading to direct tissue damage and contributing oxidant/antioxidant imbalance in the risk of chronic to the inflammation and antiprotease inactivation Correspondence to: obstructive pulmonary disease (COPD) is to investigate seen in COPD. This hypothesis is supported by Dr P A Cassano, Division of the role of genetic variation in antioxidant enzymes, and Nutritional Sciences, 209 epidemiological studies associating low dietary Savage Hall, Cornell University, indeed family based studies suggest a heritable antioxidant intake and serum antioxidant concen- Ithaca, NY 14853, USA; pac6@ component to lung disease. Many studies of the genes tration with decreased lung function4–9 and cornell.edu encoding antioxidant enzymes have considered COPD or increased COPD mortality risk.10 COPD related outcomes, and a systematic review is Many genetic association studies and compara- Received 25 June 2007 needed to summarise the evidence to date, and to Accepted 22 May 2008 tive expression studies investigated the relation Published Online First provide insights for further research. -

Glutathione S Transferases
ooggeenneessii iinn ss && rrcc aa MM CC uu tt ff aa Journal ofJournal of oo gg ll ee aa nn nn ee rr ss uu ii Nissar et al., J Carcinog Mutagen 2017, 8:2 ss oo JJ ISSN: 2157-2518 CarCarcinogenesiscinogenesis & Mutagenesis DOI: 10.4172/2157-2518.1000287 Review Article Open Access Glutathione S Transferases: Biochemistry, Polymorphism and Role in Colorectal Carcinogenesis Saniya Nissar1,2,3, Aga Syed Sameer4*, Roohi Rasool2, Nissar A Chowdri5 and Fouzia Rashid3 1Department of Biochemistry, University of Kashmir, India 2Department of Immunology and Molecular Medicine, Sher-I-Kashmir Institute of Medical Sciences, India 3Department of Clinical Biochemistry, University of Kashmir, India 4Department of Basic Medical Sciences, College of Medicine, King Saud Bin Abdulaziz University for Health Sciences. Jeddah, KSA 5Department of General Surgery, Sher-I-Kashmir Institute of Medical Sciences, India *Corresponding author: Aga Syed Sameer, Department of Basic Medical Sciences, College of Medicine, King Saud Bin Abdulaziz University for Health Sciences. Jeddah, KSA, Tel: +966542035086; E-mail: [email protected] Received date: February 19, 2017; Accepted date: March 10, 2017; Published date: March 15, 2017 Copyright: © 2017 Nissar S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Glutathione S-transferases (GSTs) are enzymes detoxifying a wide range of hazardous substances both of endogenous or exogenous origin, such as reactive oxygen species (ROS) or xenobiotics and environmental carcinogens; thereby imparting protection to DNA against oxidative damage. -

Table S1. 103 Ferroptosis-Related Genes Retrieved from the Genecards
Table S1. 103 ferroptosis-related genes retrieved from the GeneCards. Gene Symbol Description Category GPX4 Glutathione Peroxidase 4 Protein Coding AIFM2 Apoptosis Inducing Factor Mitochondria Associated 2 Protein Coding TP53 Tumor Protein P53 Protein Coding ACSL4 Acyl-CoA Synthetase Long Chain Family Member 4 Protein Coding SLC7A11 Solute Carrier Family 7 Member 11 Protein Coding VDAC2 Voltage Dependent Anion Channel 2 Protein Coding VDAC3 Voltage Dependent Anion Channel 3 Protein Coding ATG5 Autophagy Related 5 Protein Coding ATG7 Autophagy Related 7 Protein Coding NCOA4 Nuclear Receptor Coactivator 4 Protein Coding HMOX1 Heme Oxygenase 1 Protein Coding SLC3A2 Solute Carrier Family 3 Member 2 Protein Coding ALOX15 Arachidonate 15-Lipoxygenase Protein Coding BECN1 Beclin 1 Protein Coding PRKAA1 Protein Kinase AMP-Activated Catalytic Subunit Alpha 1 Protein Coding SAT1 Spermidine/Spermine N1-Acetyltransferase 1 Protein Coding NF2 Neurofibromin 2 Protein Coding YAP1 Yes1 Associated Transcriptional Regulator Protein Coding FTH1 Ferritin Heavy Chain 1 Protein Coding TF Transferrin Protein Coding TFRC Transferrin Receptor Protein Coding FTL Ferritin Light Chain Protein Coding CYBB Cytochrome B-245 Beta Chain Protein Coding GSS Glutathione Synthetase Protein Coding CP Ceruloplasmin Protein Coding PRNP Prion Protein Protein Coding SLC11A2 Solute Carrier Family 11 Member 2 Protein Coding SLC40A1 Solute Carrier Family 40 Member 1 Protein Coding STEAP3 STEAP3 Metalloreductase Protein Coding ACSL1 Acyl-CoA Synthetase Long Chain Family Member 1 Protein -

GSTO1 Purified Maxpab Rabbit Polyclonal Antibody (D01P)
GSTO1 purified MaxPab rabbit polyclonal antibody (D01P) Catalog # : H00009446-D01P 規格 : [ 100 ug ] List All Specification Application Image Product Rabbit polyclonal antibody raised against a full-length human GSTO1 Western Blot (Tissue lysate) Description: protein. Immunogen: GSTO1 (NP_004823.1, 1 a.a. ~ 241 a.a) full-length human protein. Sequence: MSGESARSLGKGSAPPGPVPEGSIRIYSMRFCPFAERTRLVLKAKGIRHE VININLKNKPEWFFKKNPFGLVPVLENSQGQLIYESAITCEYLDEAYPGKKL enlarge LPDDPYEKACQKMILELFSKVPSLVGSFIRSQNKEDYAGLKEEFRKEFTK LEEVLTNKKTTFFGGNSISMIDYLIWPWFERLEAMKLNECVDHTPKLKLW Western Blot (Tissue lysate) MAAMKEDPTVSALLTSEKDWQGFLELYLQNSPEACDYGL Host: Rabbit Reactivity: Human, Mouse Quality Control Antibody reactive against mammalian transfected lysate. enlarge Testing: Western Blot (Tissue lysate) Storage Buffer: In 1x PBS, pH 7.4 Storage Store at -20°C or lower. Aliquot to avoid repeated freezing and thawing. Instruction: MSDS: Download enlarge Datasheet: Download Western Blot (Cell lysate) Applications Western Blot (Tissue lysate) enlarge Western Blot (Transfected lysate) enlarge GSTO1 MaxPab rabbit polyclonal antibody. Western Blot analysis of GSTO1 expression in human liver. Protocol Download Western Blot (Tissue lysate) Page 1 of 3 2016/5/22 GSTO1 MaxPab rabbit polyclonal antibody. Western Blot analysis of GSTO1 expression in human placenta. Protocol Download Western Blot (Tissue lysate) GSTO1 MaxPab rabbit polyclonal antibody. Western Blot analysis of GSTO1 expression in mouse stomach. Protocol Download Western Blot (Cell lysate) GSTO1 MaxPab rabbit