3073.Full.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Set7 Lysine Methyltransferase Regulates Plasticity in Oxidative Phosphorylation Necessary for Trained Immunity Induced by Β-Glucan
University of Southern Denmark The Set7 Lysine Methyltransferase Regulates Plasticity in Oxidative Phosphorylation Necessary for Trained Immunity Induced by β-Glucan Keating, Samuel T.; Groh, Laszlo; van der Heijden, Charlotte D.C.C.; Rodriguez, Hanah; dos Santos, Jéssica C.; Fanucchi, Stephanie; Okabe, Jun; Kaipananickal, Harikrishnan; van Puffelen, Jelmer H.; Helder, Leonie; Noz, Marlies P.; Matzaraki, Vasiliki; Li, Yang; de Bree, L. Charlotte J.; Koeken, Valerie A.C.M.; Moorlag, Simone J.C.F.M.; Mourits, Vera P.; Domínguez-Andrés, Jorge; Oosting, Marije; Bulthuis, Elianne P.; Koopman, Werner J.H.; Mhlanga, Musa; El-Osta, Assam; Joosten, Leo A.B.; Netea, Mihai G.; Riksen, Niels P. Published in: Cell Reports DOI: 10.1016/j.celrep.2020.107548 Publication date: 2020 Document version: Final published version Document license: CC BY-NC-ND Citation for pulished version (APA): Keating, S. T., Groh, L., van der Heijden, C. D. C. C., Rodriguez, H., dos Santos, J. C., Fanucchi, S., Okabe, J., Kaipananickal, H., van Puffelen, J. H., Helder, L., Noz, M. P., Matzaraki, V., Li, Y., de Bree, L. C. J., Koeken, V. A. C. M., Moorlag, S. J. C. F. M., Mourits, V. P., Domínguez-Andrés, J., Oosting, M., ... Riksen, N. P. (2020). The Set7 Lysine Methyltransferase Regulates Plasticity in Oxidative Phosphorylation Necessary for Trained Immunity Induced by β-Glucan. Cell Reports, 31(3), [107548]. https://doi.org/10.1016/j.celrep.2020.107548 Go to publication entry in University of Southern Denmark's Research Portal Terms of use This work is brought to you by the University of Southern Denmark. Unless otherwise specified it has been shared according to the terms for self-archiving. -

Recurrent Inversion Toggling and Great Ape Genome Evolution
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Nat Genet Manuscript Author . Author manuscript; Manuscript Author available in PMC 2020 December 15. Published in final edited form as: Nat Genet. 2020 August ; 52(8): 849–858. doi:10.1038/s41588-020-0646-x. Recurrent inversion toggling and great ape genome evolution David Porubsky1,2,9, Ashley D. Sanders3,9, Wolfram Höps3, PingHsun Hsieh1, Arvis Sulovari1, Ruiyang Li1, Ludovica Mercuri4, Melanie Sorensen1, Shwetha C. Murali1,5, David Gordon1,5, Stuart Cantsilieris1,6, Alex A. Pollen7, Mario Ventura4, Francesca Antonacci4, Tobias Marschall8, Jan O. Korbel3, Evan E. Eichler1,5,* 1Department of Genome Sciences, University of Washington School of Medicine, Seattle, Washington, USA. 2Max Planck Institute for Informatics, Saarland Informatics Campus E1.4, Saarbrücken, Germany. 3European Molecular Biology Laboratory (EMBL), Genome Biology Unit, Heidelberg, Germany. 4Dipartimento di Biologia, Università degli Studi di Bari “Aldo Moro”, Bari, Italy. 5Howard Hughes Medical Institute, University of Washington, Seattle, Washington, USA. 6Centre for Eye Research Australia, Department of Surgery (Ophthalmology), University of Melbourne, Royal Victorian Eye and Ear Hospital, East Melbourne, Victoria, Australia. 7Department of Neurology, University of California, San Francisco (UCSF), San Francisco, California, USA. 8Institute for Medical Biometry and Bioinformatics, Medical Faculty, Heinrich Heine University Düsseldorf, Germany. 9These authors contributed equally to this work. Abstract Inversions play an important role in disease and evolution but are difficult to characterize because their breakpoints map to large repeats. We increased by six-fold the number (n = 1,069) of previously reported great ape inversions using Strand-seq and long-read sequencing. We find that the X chromosome is most enriched (2.5-fold) for inversions based on its size and duplication content. -

SETD7 Is Promising Druggable Target for Treating
Sequence and Pathway analysis SETD7 is promising druggable target for treating Lung Neoplasms that controls activity of CTCF, NR3C1 and TCF7L2 transcription factor on promoters of genes encoding enzymes metabolizing given metabolites Demo User geneXplain GmbH [email protected] Data received on 06/09/2019 ; Run on 31/10/2020 ; Report generated on 31/10/2020 Genome Enhancer release 2.2 (TRANSFAC®, TRANSPATH® and HumanPSD™ release 2020.3) Abstract In the present study we applied the software package "Genome Enhancer" to a data set that contains metabolomics data. The study is done in the context of Lung Neoplasms. The goal of this pipeline is to identify potential drug targets in the molecular network that governs the studied pathological process. In the first step of analysis pipeline discovers transcription factors (TFs) that regulate genes activities in the pathological state. The activities of these TFs are controlled by so- called master regulators, which are identified in the second step of analysis. After a subsequent druggability checkup, the most promising master regulators are chosen as potential drug targets for the analyzed pathology. At the end the pipeline comes up with (a) a list of known drugs and (b) investigational active chemical compounds with the potential to interact with selected drug targets. From the data set analyzed in this study, we found the following TFs to be potentially involved in the regulation of the genes encoding enzymes metabolizing given metabolites: CTCF, NR3C1 and TCF7L2. The subsequent network analysis suggested setd7 SUV39H1 as the most promising molecular targets for further research, drug development and drug repurposing initiatives on the basis of identified molecular mechanism of the studied pathology. -
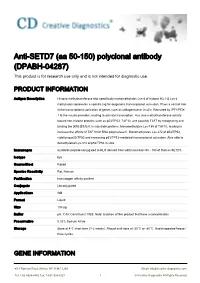
Anti-SETD7 (Aa 50-150) Polyclonal Antibody (DPABH-04287) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-SETD7 (aa 50-150) polyclonal antibody (DPABH-04287) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description Histone methyltransferase that specifically monomethylates Lys-4 of histone H3. H3 Lys-4 methylation represents a specific tag for epigenetic transcriptional activation. Plays a central role in the transcriptional activation of genes such as collagenase or insulin. Recruited by IPF1/PDX- 1 to the insulin promoter, leading to activate transcription. Has also methyltransferase activity toward non-histone proteins such as p53/TP53, TAF10, and possibly TAF7 by recognizing and binding the [KR]-[STA]-K in substrate proteins. Monomethylates Lys-189 of TAF10, leading to increase the affinity of TAF10 for RNA polymerase II. Monomethylates Lys-372 of p53/TP53, stabilizing p53/TP53 and increasing p53/TP53-mediated transcriptional activation. Also able to demethylated Lys-372 of p53/TP53 in vitro. Immunogen Synthetic peptide conjugated to KLH derived from within residues 50 - 150 of Human SETD7. Isotype IgG Source/Host Rabbit Species Reactivity Rat, Human Purification Immunogen affinity purified Conjugate Unconjugated Applications WB Format Liquid Size 100 μg Buffer pH: 7.40; Constituent: PBS. Note: Batches of this product that have a concentration Preservative 0.02% Sodium Azide Storage Store at 4°C short term (1-2 weeks). Aliquot and store at -20°C or -80°C. Avoid repeated freeze / thaw cycles. GENE INFORMATION 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] -

The Histone Methyltransferase Setd7 Promotes Pancreatic Progenitor Identity Julia Kofent, Juan Zhang and Francesca M
© 2016. Published by The Company of Biologists Ltd | Development (2016) 143, 3573-3581 doi:10.1242/dev.136226 RESEARCH ARTICLE The histone methyltransferase Setd7 promotes pancreatic progenitor identity Julia Kofent, Juan Zhang and Francesca M. Spagnoli* ABSTRACT molecular mechanisms underlying such interplay in vertebrate Cell fate specification depends on transcriptional activation driven by embryos. Establishment of the pancreatic lineage is orchestrated by lineage-specific transcription factors as well as changes in chromatin a network of TFs, including Pdx1, Ptf1a and Sox9 (Pan and Wright, organization. To date, the interplay between transcription factors and 2011; Stanger and Hebrok, 2013). Chromatin states at lineage- chromatin modifiers during development is not well understood. We specific regulatory regions in embryonic endoderm progenitors and focus here on the initiation of the pancreatic program from multipotent in different stages of their descendants to pancreatic fate have been endodermal progenitors. Transcription factors that play key roles in recently mapped (Avrahami and Kaestner, 2012; Wang et al., 2015; regulating pancreatic progenitor state have been identified, but the Xie et al., 2013; Xu et al., 2011). These studies also enabled the chromatin regulators that help to establish and maintain pancreatic identification of some relevant histone-modifying enzymes that fate are less well known. Using a comparative approach, we identify a establish chromatin states and control cell fate choices within the crucial role for the histone methyltransferase Setd7 in establishing endoderm (Avrahami and Kaestner, 2012; Xu et al., 2011). For pancreatic cell identity. We show that Setd7 is expressed in the instance, the histone acetyltransferase P300 and histone prospective pancreatic endoderm of Xenopus and mouse embryos methyltransferase EZH2 enzymes have been reported to play a prior to Pdx1 induction. -
Winners Sorted by Institute-Center
FARE2020WINNERS Sorted By Institute Ji Chen Postdoctoral Fellow CC Neuroscience - General Toward a Wearable Pediatric Robotic Knee Exoskeleton for Real World Overground Gait Rehabilitation in Ambulatory Individuals Crouch gait, or excessive knee flexion, is a debilitating gait pathology in children with cerebral palsy (CP). Surgery, bracing and therapy provide only short term correction of crouch and more sustainable solutions remain a significant challenge in children with CP. One major hurdle is achieving the required dosage and intensity of gait training necessary to produce meaningful long term improvements in walking ability. Rather than replace lost or absent function, gait training in CP population aims to improve the participant’s baseline walking pattern by encouraging longer bouts of training and exercise, which is different than in those with paralysis. Wearable robotic exoskeletons, as a potential strategy, can assist individuals with CP to gradually regain knee extension over time and help maintain it for longer periods through intense task-specific gait training. We previously tested our initial prototype which produced significant improvement in knee extension comparable in magnitude to reported results from orthopedic surgery. Children continued to exert voluntary knee extensor muscle when walking with the exoskeleton which indicated the device was assisting but not controlling their gait. These positive initial results motivated us to design second prototype to expand the user population, and to enable its effective use outside of the laboratory environment. The current version has individualized control capability and device portability for home use as it implemented a multi-layered closed loop control system and a microcontroller based data acquisition system. -
EHMT2 Epigenetically Suppresses Wnt Signaling and Is a Potential
RESEARCH ARTICLE EHMT2 epigenetically suppresses Wnt signaling and is a potential target in embryonal rhabdomyosarcoma Ananya Pal1, Jia Yu Leung1,2, Gareth Chin Khye Ang1,2, Vinay Kumar Rao1, Luca Pignata2,3, Huey Jin Lim4, Maxime Hebrard2, Kenneth TE Chang5, Victor KM Lee4, Ernesto Guccione2,3, Reshma Taneja1* 1Department of Physiology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore; 2Institute of Molecular and Cell Biology (IMCB), Agency for Science, Technology and Research (A*STAR), Singapore, Singapore; 3Department of Biochemistry, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore; 4Department of Pathology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore; 5Department of Pathology, KK Women and Children’s Hospital, Singapore, Singapore Abstract Wnt signaling is downregulated in embryonal rhabdomyosarcoma (ERMS) and contributes to the block of differentiation. Epigenetic mechanisms leading to its suppression are unknown and could pave the way toward novel therapeutic modalities. We demonstrate that EHMT2 suppresses canonical Wnt signaling by activating expression of the Wnt antagonist DKK1. Inhibition of EHMT2 expression or activity in human ERMS cell lines reduced DKK1 expression and elevated canonical Wnt signaling resulting in myogenic differentiation in vitro and in mouse xenograft models in vivo. Mechanistically, EHMT2 impacted Sp1 and p300 enrichment at the DKK1 promoter. The reduced tumor growth upon EHMT2 deficiency was reversed by recombinant DKK1 or LGK974, which also inhibits Wnt signaling. Consistently, among 13 drugs targeting chromatin *For correspondence: modifiers, EHMT2 inhibitors were highly effective in reducing ERMS cell viability. Our study [email protected] demonstrates that ERMS cells are vulnerable to EHMT2 inhibitors and suggest that targeting the Competing interests: The EHMT2-DKK1-b-catenin node holds promise for differentiation therapy. -

Inhibition of Methyltransferase Setd7 Allows the in Vitro Expansion of Myogenic Stem Cells with Improved Therapeutic Potential
Article Inhibition of Methyltransferase Setd7 Allows the In Vitro Expansion of Myogenic Stem Cells with Improved Therapeutic Potential Graphical Abstract Authors Robert N. Judson, Marco Quarta, Menno J. Oudhoff, ..., Mohammad M. Karimi, Thomas A. Rando, Fabio M. Rossi Correspondence [email protected] In Brief Judson et al. show that lysine- methyltransferase Setd7 acts cytoplasmically to regulate the differentiation of skeletal muscle stem cells (MuSCs) by priming b-catenin for nuclear import. Pharmacological inhibition of Setd7 can provide a strategy to enhance the in vitro expansion and transplantation potential of murine and human MuSCs. Highlights d Deletion of Setd7 impairs myogenic differentiation and skeletal muscle regeneration d Setd7 is localized to the cytoplasm of MuSCs and primes b-catenin for nuclear entry d Small-molecule targeting of Setd7 enhances expansion of transplantable MuSCs d Inhibition of Setd7 improves therapeutic potential of cultured mouse and human MuSCs Judson et al., 2018, Cell Stem Cell 22, 177–190 February 1, 2018 ª 2017 Elsevier Inc. https://doi.org/10.1016/j.stem.2017.12.010 Cell Stem Cell Article Inhibition of Methyltransferase Setd7 Allows the In Vitro Expansion of Myogenic Stem Cells with Improved Therapeutic Potential Robert N. Judson,1,2 Marco Quarta,3,4,5,10 Menno J. Oudhoff,1,6,10 Hesham Soliman,1 Lin Yi,1 Chih Kai Chang,1 Gloria Loi,1 Ryan Vander Werff,1 Alissa Cait,1 Mark Hamer,3,4,5 Justin Blonigan,3,4,5 Patrick Paine,3,4,5 Linda T.N. Doan,3,4,5 Elena Groppa,1 WenJun He,1 Le Su,1,8 Regan H. -

SETD7 Is a Prognosis Predicting Factor of Breast Cancer and Regulates Redox Homeostasis
www.impactjournals.com/oncotarget/ Oncotarget, 2017, Vol. 8, (No. 55), pp: 94080-94090 Research Paper SETD7 is a prognosis predicting factor of breast cancer and regulates redox homeostasis Run Huang1,*, Xiaolin Li1,*, Yang Yu2,*, Lisi Ma1, Sixuan Liu1, Xiangyun Zong1 and Qi Zheng3 1Department of Breast Surgery, Shanghai Jiao Tong University Affiliated Shanghai Sixth People’s Hospital, Shanghai 200233, China 2Department of Breast Surgery, Zhejiang Cancer Hospital, Hangzhou 310022, China 3Department of General Surgery, Shanghai Jiao Tong University Affiliated Shanghai Sixth People’s Hospital, Shanghai 200233, China *These authors have contributed equally to this work Correspondence to: Xiangyun Zong, email: [email protected] Keywords: SETD7, breast cancer, redox homeostasis, reactive oxygen species, oxidative stress Received: June 30, 2017 Accepted: September 21, 2017 Published: October 06, 2017 Copyright: Huang et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License 3.0 (CC BY 3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. ABSTRACT SETD7 is a methyltransferase that specifically catalyzes the monomethylation of lysine 4 on histone H3. A variety of studies has revealed the role of SETD7 in posttranslational modifications of non-histone proteins. However, the prognostic value of SETD7 on breast cancer and the ability of SETD7 of regulating intrinsic redox homeostasis has never been investigated. In this study, using The Cancer Genome Atlas (TCGA) database, we revealed that SETD7 was a potential prognostic marker of breast cancer. Median survival time of patients with low SETD7 expression (18.1 years) was twice than that of SETD7 low-expressed patients (9.5 years). -

Human SETD7 / SET9 - Purified
OriGene Technologies, Inc. OriGene Technologies GmbH 9620 Medical Center Drive, Ste 200 Schillerstr. 5 Rockville, MD 20850 32052 Herford UNITED STATES GERMANY Phone: +1-888-267-4436 Phone: +49-5221-34606-0 Fax: +1-301-340-8606 Fax: +49-5221-34606-11 [email protected] [email protected] SA6049X Human SETD7 / SET9 - Purified Alternate names: H3-K4-HMTase SETD7, Histone H3-K4 methyltransferase SETD7, Histone-lysine N- methyltransferase SETD7, KIAA1717, KMT7, Lysine N-methyltransferase 7, SET domain- containing protein 7, SET7, SET7/9 Quantity: 0.5 mg Concentration: 1.0 mg/ml (determined by Bradford assay) Background: SET 7/9 is a histone methyltransferase (HMTase) that transfers methyl groups to Lys4 of histone H3, in complex with S-adenosyl-L-methionine (AdoMet). The methylation of lysine residues of histones plays a critical role in the regulation of chromatin structure and gene expression. Acetylation, phosphorylation and methylation of the amino- terminal tails of histone are thought to be involved in the regulation of chromatin structure and function. The enzymes identified in the methylation of specific lysine residue on histones belong to the SET family with just one exception. SET 7/9, unlike most other SET proteins, is exclusively a mono-methylase. Uniprot ID: Q8WTS6 NCBI: NP_085151.1 GeneID: 80854 Species: Human Source: E. coli Format: State: Liquid Purity: >95% by SDS-PAGE Buffer System: 50 mM Tris-HCl buffer (pH7.5) 0.2M NaCl, 5mM DTT, 20% glycerol Description: Recombinant human SET7/9, was cloned into an E. coli expression vector and was purified to apparent homogeneity by using conventional column chromatography techniques. -

SETD7-Mediated Monomethylation Is Enriched on Soluble Tau in Alzheimer's Disease
Bichmann et al. Molecular Neurodegeneration (2021) 16:46 https://doi.org/10.1186/s13024-021-00468-x RESEARCH ARTICLE Open Access SETD7-mediated monomethylation is enriched on soluble Tau in Alzheimer’s disease Maria Bichmann1, Nuria Prat Oriol1,2, Ebru Ercan-Herbst1, David C. Schöndorf1,3, Borja Gomez Ramos1,4,5, Vera Schwärzler1, Marie Neu3, Annabelle Schlüter3, Xue Wang6, Liang Jin6, Chenqi Hu6, Yu Tian6, Janina S. Ried7, Per Haberkant8, Laura Gasparini3 and Dagmar E. Ehrnhoefer1,3* Abstract Background: Human tauopathies including Alzheimer’s disease (AD) are characterized by alterations in the post- translational modification (PTM) pattern of Tau, which parallel the formation of insoluble Tau aggregates, neuronal dysfunction and degeneration. While PTMs on aggregated Tau have been studied in detail, much less is known about the modification patterns of soluble Tau. Furthermore, PTMs other than phosphorylation have only come into focus recently and are still understudied. Soluble Tau species are likely responsible for the spreading of pathology during disease progression and are currently being investigated as targets for immunotherapies. A better understanding of their biochemical properties is thus of high importance. Methods: We used a mass spectrometry approach to characterize Tau PTMs on a detergent-soluble fraction of human AD and control brain tissue, which led to the discovery of novel lysine methylation events. We developed specific antibodies against Tau methylated at these sites and biochemically characterized methylated Tau species in extracts from human brain, the rTg4510 mouse model and in hiPSC-derived neurons. Results: Our study demonstrates that methylated Tau levels increase with Tau pathology stage in human AD samples as well as in a mouse model of Tauopathy. -

Genetic'dissection'of'growth'and' Meat'quality'traits'in'pigs''
! ! ! UNIVERSITAT*AUTÒNOMA*DE*BARCELONA* Departament*de*Ciència*Animal*i*dels*Aliments* Facultat*de*Veterinària* CENTRE*DE*RECERCA*EN*AGRIGENÒMICA* Grup*de*Recerca*de*Genòmica*Animal* * GENETIC'DISSECTION'OF'GROWTH'AND' MEAT'QUALITY'TRAITS'IN'PIGS'' ANNA'PUIG'OLIVERAS' * PhD*Thesis*in*Animal*Production* Bellaterra,*September*2015* * Supervisors* Dr.*Josep*Maria*Folch*Albareda*****************Dra.*Maria*Ballester*Devis* ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! 4.#GENERAL#DISCUSSION# # # ! # ! 4.#GENERAL#DISCUSSION# # Consumer$demand$for$healthy$high$quality$pork$products$has$grown$fast$during$the$ last$decades$(Ngapo$et#al.,$2003;$Grunert$2005).$Economically$important$production$ traits$ in$ the$ pork$ industry$ such$ as$ growth,$ fatness$ and$ meat$ quality$ vary$ greatly$ among$ individuals$ and$ do$ not$ show$ simple$ Mendelian$ inheritance$ (Andersson$ &$ Georges$2004).$The$genetic$basis$lying$behind$these$complex$traits$is$believed$to$be$ determined$by$many$loci$with$a$small$effect$and$few$genes$with$moderate$effects$ (Hayes$&$Goddard$2001).$Over$the$years,$all$these$traits$have$been$systematically$ screened$ with$ traditional$ and$ novel$ technologies$ to$ unravel$ their$ genetic$ basis,$ contributing$ with$ new$ advances$ to$ both$ the$ scientific$ community$ and$ the$ pork$ industry.$Approaches$like$candidate$gene$association$analyses$(Linville$et#al.,$2001)$ and$QTL$mapping$(Rothschild$et#al.,$2007)$provided$new$insights$about$the$genetic$ architecture$ of$ pork$ complex$ traits.$ More$ recently,$ highTthroughput$ genotyping$ platforms$