Post-Consultation Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Plymouth, South Hams & West Devon Local Planning Authorities' 2018, 5
Plymouth, South Hams & West Devon Local Planning Authorities’ 2018, 5 Year Housing Land Supply Position Statement July 2019 Contents 1. Introduction ............................................................................................................................................... 2 2. What is the 5 year land supply? ............................................................................................................ 2 3. What is the Housing Delivery Test? .................................................................................................... 3 4. National Policy & Guidance - Demonstrating a 5 Year Supply ...................................................... 9 5. JLP whole plan delivery 2014-2019 & 5 Year Housing Land Supply Position (2019 monitoring point) ........................................................................................................................................... 11 Appendices Appendix 1. MHCLG letter confirming recalculated 2018 HDT measurement for the 3 JLP authorities Appendix 2. Plymouth LPA supply over the next 5 years (2019-2024) Appendix 3 South Hams LPA supply over the next 5 years (2019-2024) Appendix 4. West Devon LPA supply over the next 5 years (2019-2024) Appendix 5. Sites removed from 5 Year Land Supply (lapsed and undeliverable consents & sites considered developable not deliverable 2019-2024) Appendix 6. Amendments to past net additional dwelling delivery due to NPPF/NPPG changes regarding counting student and communal accommodation Appendix 7. List of Small -

Okehampton Hamlets Parish Council
Okehampton Hamlets Parish Council Minutes of the Annual Parish Assembly held at 7.30pm on Tuesday 16th April 2013 at Meldon Village Hall Parish councillors present D Webber (Chair), P Heard, R Maile, M Cooper, and M Littlejohns. Guest speakers Ian Jarvis, Camp Commandant, Okehampton Camp Stephen Goodwin, General Manager, Dartmoor Railway CIC Lisa Wadling, Okehampton Town Events Manager Also Present Cllr M Morse, Cllr J McInnes Clerk – J Gillard 6 members of the public 1. The Chairman welcomed everyone to the meeting, he thanked the Councillors and Clerk for their support throughout the year. 2. Apologies – Councillor Mrs C Marsh. 3. Minutes of the previous Annual Assembly were approved and signed by the Chairman. 4. Matters arising from the minutes - None 5. The Chairman gave the following report for 2012/13: Full compliment of Councillors throughout the year. Chair also represented Parish Councils on DNP authority. Council also represented on : Okehampton United Charities, Holditch Trust, West Devon/Okehampton Liaison Group, Northern Parishes Links Group, Chamber of Trade, Police Liaison Group. Okehampton Matters. Meldon Hall,took part in Rembrance Day parade, Civic Dinner and Ten Tors Breakfast This year the Council have made donations to: OCRA 200.00 OKEHAMPTON TOWN COUNCIL 50.00 FATHERFORD ROAD ALLOTMENT ASS 100.00 ROYAL BRITISH LEGION 50.00 WREN MUSIC 100.00 WEST DEVON CITIZENS ADVICE 300.00 Annual Assembly Minutes 2013 OKEHAMPTON COMMUNITY GARDEN 300.00 MELDON VIADUCT 200.00 NORTH DARTMOOR RESCUE 500.00 TOTAL 1800.00 Localism Act introduced this year – New code of conduct and register of interests Councils can now register land/buildings as Comminty Interest TAP fund introduced, to encourage parishes to work together on projects, approx £19,000 available for Northern Parishes, all distributed during the year, Hamlets joined with the Town on successful application for protective clothing for the volunteer litter/dog poo picker up !! Other parishes done things like spraying weeds, purchasing grit spreaders, purchasing defibrillators. -

West Devon Borough Council East of Okehampton Masterplan Draft
0 West Devon Borough Council East of Okehampton Masterplan Draft Supplementary Planning Document September 2013 – Committee version This document can be made available in large print, Braille or tape format on request. Committee version September 2013 Produced by the Strategic Planning Team West Devon Borough Council Kilworthy Park Tavistock PL19 0BZ Email: [email protected] Telephone: 01822 813600 © West Devon Borough Council East of Okehampton Masterplan – September 2013 Committee Version 2 Contents 1. Introduction Page 5 a. What is a masterplan? b. Why are we preparing a masterplan for new development in Okehampton? c. What will this masterplan look at? d. How have we prepared the masterplan? e. What is the status of the masterplan and how should it be used? 2. Masterplan background Page 9 a. About Okehampton and the Hamlets b. Planning policy context c. Environmental designations 3. Priorities for new development Page 13 a. Community engagement b. Local council engagement c. Infrastructure provider engagement 4. The allocations Page 18 Parcel 1: Opportunity Okehampton Parcel 2: North of Crediton Road Parcel 3: South of Crediton Road Parcel 4: East of Stockley Valley Parcel 5: North of Stockley Hamlet 5. Design principles Page 45 a. Access and street layout - Vehicle - footpaths and cycleways b. Biodiversity c. Boundaries d. Broadband connections e. Building materials and style f. Character areas and development densities g. Open space provision h. Orientation i. Parking j. Properties and their usability k. Public transport l. Site entrances m. Sustainable energy n. Sustainable Urban Drainage o. Street furniture East of Okehampton Masterplan – September 2013 Committee Version 3 6. -

Notice of Election Double Column
NOTICE OF ELECTION West Devon Borough Council Election of Parish Councillors for the Electoral Areas listed below Number of Parish Number of Parish Electoral Areas Councillors to be Electoral Areas Councillors to be elected elected Beaworthy (East Beaworthy Ward) Two Lewdown Grouped (Coryton) Two Beaworthy (Ward) Five Lewdown Grouped (Lewtrenchard) Three Belstone Seven Lewdown Grouped (Marystow) Three Bere Ferrers Thirteen Lewdown Grouped (Thrushelton) Three Bratton Clovelly Seven Lifton Ten Brentor Seven Lydford Seven Bridestowe Seven Mary Tavy Nine Broadwoodkelly Seven Meeth Seven Buckland Monachorum (Buckland Harrowbeer) Two Milton Abbot Grouped (Bradstone) One Buckland Monachorum (Buckland Village) Ten Milton Abbot Grouped (Dunterton) One Burrator Grouped (Meavy Dousland) Four Milton Abbot Grouped (Chillaton) Four Burrator Grouped (Meavy Village) Three Milton Abbot Grouped (Milton Abbot) Four Burrator Grouped (Sheepstor) Two Monkokehampton Seven Burrator Grouped (Walkhampton Dousland) Four North Tawton Twelve Burrator Grouped (Walkhampton Village) Three Northlew Nine Chagford Twelve Okehampton Hamlets (Little Fatherford Ward) One Dartmoor Forest (Huccaby Ward) One Okehampton Hamlets (North Ward) Six Dartmoor Forest (Postbridge Ward) Two Okehampton Hamlets (South Ward) One Dartmoor Forest (Princetown Ward) Seven Okehampton Town Council (North Ward) Eight Drewsteignton (Crockernwell Ward) Two Okehampton Town Council (South Ward) Six Drewsteignton (Venton Ward) One Peter Tavy Seven Drewsteignton (Ward) Three Plasterdown Grouped (Sampford -

1911 Census Families.Pdf
Forenames Surname Relationship Status MarriedFor Gender Age YOB POB Occupation County Address Parish RegDist Hd No Henry YEO Head Married M 25 1886 Middlesex Hoxton Collector of Monies London 34 Kiver Road Upper Holloway N Islington Islington 1 1 Florence YEO Wife Married F 22 1889 Middlesex Islington N London 34 Kiver Road Upper Holloway N Islington Islington 1 3 Unnamed YEO Daughter F 0 (1 MONTH) 1911 Middlesex Islington N London 34 Kiver Road Upper Holloway N Islington Islington 1 4 Under Ground Colliery Harry YEO Head Married M 23 1888 Exmoth Devon Glamorganshire 21 Dolycoed Tylorstown Glam Wales Rhondda Pontypridd 2 1 Labourer Underground Rhoda YEO Wife Married 3 years F 23 1888 Tedhim St Mary Devon Glamorganshire 21 Dolycoed Tylorstown Glam Wales Rhondda Pontypridd 2 2 Harry YEO Son M 1 1910 Exmouth Devon Glamorganshire 21 Dolycoed Tylorstown Glam Wales Rhondda Pontypridd 2 4 Unnamed YEO Son M 0 (3 DAYS) 1911 Tylorstown Glamorgan Glamorganshire 21 Dolycoed Tylorstown Glam Wales Rhondda Pontypridd 2 5 Absalom James YEO Head Married M 35 1876 Okehampton Devon Mason Devonshire White Horse Court Okehampton Devon Esb Missing Okehampton 3 1 Edith YEO Wife Married 9 years F 25 1886 Sticklepark Nr Okehampton Devonshire White Horse Court Okehampton Devon Esb Missing Okehampton 3 2 Elsie Gladys YEO Daughter F 8 1903 Okehampton Devon School Devonshire White Horse Court Okehampton Devon Esb Missing Okehampton 3 4 Willie James YEO Son M 6 1905 Okehampton Devon School Devonshire White Horse Court Okehampton Devon Esb Missing Okehampton 3 5 Absalom -

Npa/Ag/14/046 Dartmoor National Park Authority
NPA/AG/14/046 DARTMOOR NATIONAL PARK AUTHORITY AUDIT AND GOVERNANCE COMMITTEE 15 August 2014 ANNUAL STATEMENT OF ACCOUNTS 2013/14 Report of the Head of Resources Recommendation : That Members review the 2013/14 Statement of Accounts prior to Authority approval on 5 September 2014 1 Introduction 1.1 The Statement of Accounts is a statutory document which all local authorities have to produce and make available for public inspection. In addition, the accounts are subject to external examination by the Authority’s external auditors. 1.2 The Chartered Institute of Public Finance and Accountancy (CIPFA) publishes The Code of Practice on Local Authority Accounting (The Code) which specifies the principles and practices of accounting that must be followed in preparing the statement of accounts. The Statement of Accounts must be authorised for issue and made available for public inspection by 30 June each year; the un-audited copy can be accessed on our website at http://www.dartmoor.gov.uk/__data/assets/pdf_file/0006/462525/Unaudited-Annual- Statement-of-Accounts-2013-14.pdf (copy provided to Members). 1.3 The external auditor reviews compliance against the requirements of The Code and must provide the audit opinion and the Annual Governance Report by 30 September each year. 1.4 There are no significant changes to the format or the content of the Statement of Accounts this year, but there is one change of accounting policy that the Authority has applied relating to the presentation and disclosure of post-employment benefits. The overall measurement of the Authority’s net pension liability has not changed; there are just some reclassifications of the components into which year-on-year changes in the net liability are analysed. -

Heritage at Risk Register 2015, South West
South West Register 2015 HERITAGE AT RISK 2015 / SOUTH WEST Contents Heritage at Risk III Poole (UA) 185 Somerset 185 The Register VII Exmoor (NP) 185 Content and criteria VII Mendip 187 Sedgemoor 192 Criteria for inclusion on the Register IX South Somerset 196 Reducing the risks XI Taunton Deane 203 Key statistics XIV West Somerset 205 South Gloucestershire (UA) 206 Publications and guidance XV Swindon (UA) 209 Key to the entries XVII Torbay (UA) 211 Entries on the Register by local planning XIX authority Wiltshire (UA) 213 Bath and North East Somerset (UA) 1 Bournemouth (UA) 3 Bristol, City of (UA) 4 Cornwall (UA) 8 Devon 47 Dartmoor (NP) 47 East Devon 75 Exeter 83 Exmoor (NP) 83 Mid Devon 84 North Devon 87 South Hams 92 Teignbridge 100 Torridge 103 West Devon 112 Dorset 115 Christchurch 115 East Dorset 116 North Dorset 121 Purbeck 129 West Dorset 136 Weymouth and Portland 153 Gloucestershire 154 Cheltenham 154 Cotswold 155 Forest of Dean 161 Gloucester 165 Stroud 168 Tewkesbury 171 Isles of Scilly (UA) 174 North Somerset (UA) 178 Plymouth, City of (UA) 180 II South West Summary 2015 or the first time, we’ve compared all sites on the Heritage at Risk Register – from houses to hillforts – to help us better understand which types of site are most Fcommonly at risk. There are things that make each region special and, once lost, will mean a sense of our region’s character is lost too. Comparing the South West to the national Register shows that 62.2% of all hillforts and 58.7% of all types of cairns are in our region. -

030614 Full Council Minutes
Minutes of Okehampton Town Council Meeting held on Tuesday 3 June 2014 in the Council Chamber, Town Hall, Okehampton at 7.00 pm Members Present: Councillor P Vachon (Town Mayor) Councillor K Ball Councillor T Cummings Councillor M Davies Councillor Mrs J Goffey Councillor Dr M Ireland Councillor A Leech Councillor C Letchford Councillor Mrs M McDonald Councillor Mrs C Marsh Councillor B Stephens Councillor Mrs J Yelland In Attendance: Mr P R Snell (Town Clerk) Mr B Thompson (Head of Transport Co-ordination Services, Devon County Council) Before proceeding with business, prayers were offered by Councillor Reverend M Davies. 33. Apologies for Absence - Apologies for absence were presented on behalf of Councillor D Weekes and Councillor R Boyce. 34. Deferment of Business - Mr Bruce Thompson, who had agreed to attend the meeting to present Devon County Council’s view on the railway alternatives currently being pursued, confirmed that Devon County Council (DCC) would be supportive of an option where there was demonstrable benefit to the local economy. There were currently 5 upper-tier SW councils working together on a theme to overcome problems of resilience both east and west of Exeter. Mr Thompson indicated that there was a need to build consensus across the South West in order to exploit the potential for connectivity in north and west Devon compared with the Dawlish avoidance option. The strategy should await the Network Rail study currently in progress, build a good business case for the Northern Alternative Route, demonstrating the benefits for Torridge, North Cornwall and West Devon and drawing on prospects for good journey times together with connectivity with the Waterloo line. -

New Okehampton Special School: Approval of Capital Funding and Commencement of the Free School Presumption Process
PTE/20/26 Cabinet 14 October 2020 New Okehampton Special School: Approval of Capital Funding and Commencement of the Free School Presumption Process Report of the Head of Planning, Transportation and Environment Please note that the following recommendations are subject to consideration and determination by the Cabinet (and confirmation under the provisions of the Council’s Constitution) before taking effect. Recommendation: (a) that Cabinet approve revenue funding, and the allocation of existing capital funding, to support the delivery of a new special school in Okehampton, the preparation of a reserved matters planning application following a grant of outline planning permission (which is presently being sought) and full design subject to securing the necessary planning consent; (b) that Cabinet approve the Commencement of the Presumption Free School process subject to securing the necessary planning consent; (c) pursuant to s.122 of the Local Government Act 1972, that Cabinet approve the appropriation of land at East Okehampton Business Park such that it be held for planning purposes under s226(1)(a) of the Town and Country Planning Act 1990; (d) that Cabinet delegates to the Head of Planning, Transportation and Environment power to negotiate and authorise compensation payments and agreements which may be required pursuant to s.122 of the Local Government Act 1972 as a result of the appropriation of the land. 1. Summary Presentation of this report to Cabinet seeks to obtain the necessary approvals to establish a new Special School through the Department for Education’s Free School Presumption process on land at East Okehampton Business Park, approval of capital funding and revenue funding to provide the new school, approval of the appropriation of land and delegated powers to the Head of Planning, Transportation and Environment. -

West Devon Borough
PTE/20/32 Development Management Committee 21 October 2020 County Council Development West Devon Borough: New special educational needs school including two- storey school building, hard and soft play areas, playing fields, car park, turning zone and services/plant store (outline application with all matters reserved), Okehampton East Business Park, Higher Stockley Mead, Okehampton Applicant: Devon County Council Application No: DCC/4194/2020 Date application received by Devon County Council: 28 July 2020 Report of the Chief Planner Please note that the following recommendations are subject to consideration and determination by the Committee before taking effect. Recommendation: It is recommended that outline planning permission is granted subject to the conditions set out in Appendix I of this report (with any subsequent minor changes to the conditions being agreed in consultation with the Chair and Local Member). 1. Summary 1.1 The applicant is seeking outline planning permission for a new Special Educational Needs school including two-storey school building, hard and soft play areas, playing fields, car park, turning zone and services/plant store. 1.2 The main material planning consideration in the determination of this application are that the proposal is a departure from the development plan, specifically Policy DEV14 (Maintaining a flexible mix of employment sites) of the Plymouth and South West Devon Joint Local Plan, together with the impacts on landscape, including Dartmoor National Park, the local highway network, amenity considerations and climate change. 1.3 The planning application, representations received, and consultation responses are available to view on the Council website under reference DCC/4194/2020 or by clicking on the following link: https://planning.devon.gov.uk/PlanDisp.aspx?AppNo=DCC/4194/2020. -

Okehampton North Application
PLANNING APPLICATION REPORT Case Officer: Clare Stewart Parish: Okehampton Hamlets Ward: Okehampton North Application No : 2793/17/FUL Agent/Applicant: Applicant: Mr R Murrin Messrs Burton, West, Croom & Brooks 1 Sunnyridge Castle Road Okehampton EX20 1HU Site Address: Barns adjacent to Lower Chichacott, Chichacott Road, Okehampton, Devon, EX20 1RS Development: Application for proposed barn conversion to two dwellings Reason item is being put before Committee The application has been called in by the Ward Councillor Leech who is not satisfied the proposal would secure the future of a heritage asset and is not convinced there is a need for additional housing in this area unless it is low cost affordable housing. Recommendation: Conditional approval Conditions 1. Time limit 2. Accord with plans 3. Submission of Natural England licence 4. Foul drainage 5. Surface water drainage (with reference to CDA requirements) 6. No demolition works 7. Samples of exterior finishes 8. Stonework 9. Flush fitting rooflights 10. Details of new access gate 11. Retention of existing boundary hedge/bank along road frontage 12. Parking for each unit to be made available prior to occupation and thereafter retained 13. Windows/doors to be retained in timber 14. Removal of permitted development rights Key issues for consideration: Principle, design, heritage, landscape, neighbour amenity, highways. Site Description: The barns are located in the small hamlet of Chichacott approximately 740m to the north east of Okehampton. The barns are situated adhacent to a road and the west of a Grade II listed residence known as Lower Chichacott House. The barns are in separate ownership to the dwellinghouse. -
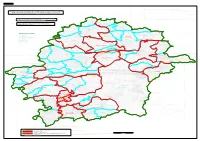
Map Referred to in the West Devon (Electoral Changes) Order 2015 Sheet 1 of 1
SHEET 1, MAP 1 Map referred to in the West Devon (Electoral Changes) Order 2015 Sheet 1 of 1 This map is based upon Ordnance Survey material with the permission of Ordnance Survey on behalf of the Controller of Her Majesty's Stationery Office © Crown copyright. Unauthorised reproduction infringes Crown copyright and may lead to prosecution or civil proceedings. The Local Government Boundary Commission for England GD100049926 2015. MEETH CP IDDESLEIGH CP Boundary alignments and names shown on the mapping background may not be up to date. They may differ from the latest Boundary information applied as part of this review. M O N BROADWOODKELLY K O CP K E C H P A M P T O N HIGHAMPTON BONDLEIGH CP CP HATHERLEIGH CP HATHERLEIGH KEY TO PARISH WARDS EXBOURNE OKEHAMPTON CP CP A NORTH NORTH TAWTON CP B SOUTH JACOBSTOWE EXBOURNE CP OKEHAMPTON HAMLETS CP C LITTLE FATHERFORD D NORTH E SOUTH TAVISTOCK CP SAMPFORD COURTENAY CP F NORTH NORTHLEW CP G SOUTH EAST H SOUTH WEST INWARDLEIGH CP OKEHAMPTON NORTH D SPREYTON CP BEAWORTHY CP A C OKEHAMPTON STICKLEPATH CP CP B GERMANSWEEK SOUTH TAWTON CP CP BELSTONE CP SOUTH TAWTON BRATTON CLOVELLY CP OKEHAMPTON HAMLETS CP OKEHAMPTON SOUTH DREWSTEIGNTON SOURTON CP DREWSTEIGNTON CP E THROWLEIGH CP BRIDESTOWE THRUSHELTON CP LANDS COMMO TO THE PARISHES BRIDESTOWE CP OF BRIDESTOWE AND SOURTON GIDLEIGH CP STOWFORD CP CHAGFORD CP LEWTRENCHARD CP CHAGFORD LIFTON CP LYDFORD CP MARYSTOW CP CORYTON CP TAMARSIDE KELLY CP BRENTOR CP BRADSTONE CP MARY TAVY CP MARY TAVY MILTON ABBOT CP PETER TAVY CP DUNTERTON DARTMOOR CP MILTON