Module 9: Urinary Incontinence
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CMS Manual System Human Services (DHHS) Pub
Department of Health & CMS Manual System Human Services (DHHS) Pub. 100-07 State Operations Centers for Medicare & Provider Certification Medicaid Services (CMS) Transmittal 8 Date: JUNE 28, 2005 NOTE: Transmittal 7, of the State Operations Manual, Pub. 100-07 dated June 27, 2005, has been rescinded and replaced with Transmittal 8, dated June 28, 2005. The word “wound” was misspelled in the Interpretive Guidance section. All other material in this instruction remains the same. SUBJECT: Revision of Appendix PP – Section 483.25(d) – Urinary Incontinence, Tags F315 and F316 I. SUMMARY OF CHANGES: Current Guidance to Surveyors is entirely replaced by the attached revision. The two tags are being combined as one, which will become F315. Tag F316 will be deleted. The regulatory text for both tags will be combined, followed by this revised guidance. NEW/REVISED MATERIAL - EFFECTIVE DATE*: June 28, 2005 IMPLEMENTATION DATE: June 28, 2005 Disclaimer for manual changes only: The revision date and transmittal number apply to the red italicized material only. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents. II. CHANGES IN MANUAL INSTRUCTIONS: (N/A if manual not updated.) (R = REVISED, N = NEW, D = DELETED) – (Only One Per Row.) R/N/D CHAPTER/SECTION/SUBSECTION/TITLE R Appendix PP/Tag F315/Guidance to Surveyors – Urinary Incontinence D Appendix PP/Tag F316/Urinary Incontinence III. FUNDING: Medicare contractors shall implement these instructions within their current operating budgets. IV. ATTACHMENTS: Business Requirements x Manual Instruction Confidential Requirements One-Time Notification Recurring Update Notification *Unless otherwise specified, the effective date is the date of service. -

Urinary Tract Infection (UTI): Western and Ayurvedic Diagnosis and Treatment Approaches
Urinary tract infection (UTI): Western and Ayurvedic Diagnosis and Treatment Approaches. By: Mahsa Ranjbarian Urinary system Renal or Urinary system is one of the 10 body systems that we have. This system is the body drainage system. The urinary system is composed of kidneys (vrikka), ureters (mutravaha nadis), bladder(mutrashaya) and urethra(mutramarga). The kidneys are a pair of bean-shaped, fist size organs that lie in the middle of the back, just below the rib cage, one on each side of the spine. Ureters are tubes that carry the wastes or urine from the kidneys to the bladder. The urine finally exit the body from the urethra when the bladder is full.1 Urethras length is shorter in women than men due to the anatomical differences. Major function of the urinary system is to remove wastes and water from our body through urination. Other important functions of the urinary system are as follows. 1. Prevent dehydration and at the same time prevent the buildup of extra fluid in the body 2. Cleans the blood of metabolic wastes 3. Removing toxins from the body 4. Maintaining the homeostasis of many factors including blood PH and blood pressure 5. Producing erythrocytes 6. make hormones that help regulate blood pressure 7. keep bones strong 8. keep levels of electrolytes, such as potassium and phosphate, stable 2 The Urinary system like any other systems of our body is working under the forces of three doshas, subdoshas. Mutravaha srotas, Ambuvahasrota and raktavahasrota are involved in formation and elimination of the urine. Urine gets separated from the rasa by maladhara kala with the help of pachaka pitta and samana vayu and then through the mutravaha srota(channels carrying the urine) it is taken to the bladder. -

Guide to Treating Your Child's Daytime Or Nighttime Accidents
A GUIDE TO TREATING YOUR CHILD’S Daytime or Nighttime Accidents, Urinary Tract Infections and Constipation UCSF BENIOFF CHILDREN’S HOSPITALS UROLOGY DEPARTMENT This booklet contains information that will help you understand more about your child’s bladder problem(s) and provides tips you can use at home before your first visit to the urology clinic. www.childrenshospitaloakland.org | www.ucsfbenioffchildrens.org 2 | UCSF BENIOFF CHILDREN’S HOSPITALS UROLOGY DEPARTMENT Table of Contents Dear Parent(s), Your child has been referred to the Pediatric Urology Parent Program at UCSF Benioff Children’s Hospitals. We specialize in the treatment of children with bladder and bowel dysfunction. This booklet contains information that will help you understand more about your child’s problem(s) and tips you can use at home before your first visit to the urology clinic. Please review the sections below that match your child’s symptoms. 1. Stool Retention and Urologic Problems (p.3) (Bowel Dysfunction) 2. Bladder Dysfunction (p.7) Includes daytime incontinence (wetting), urinary frequency and infrequency, dysuria (painful urination) and overactive bladder 3. Urinary Tract Infection and Vesicoureteral Reflux (p. 10) 4. Nocturnal Enuresis (p.12) Introduction (Nighttime Bedwetting) It’s distressing to see your child continually having accidents. The good news is that the problem is very 5. Urologic Tests (p.15) common – even if it doesn’t feel that way – and that children generally outgrow it. However, the various interventions we offer can help resolve the issue sooner THIS BOOKLET ALSO CONTAINS: rather than later. » Resources for Parents (p.16) » References (p.17) Childhood bladder and bowel dysfunction takes several forms. -

60 Seasonal Variation in Urinary Frequency
60 Cartwright R1, Rajan P2, Swamy S3, Mariappan P4, Turner K J5, Stewart L4, Khullar V1 1. Dept of Urogynaecology, St Mary's Hospital, London, UK, 2. Dept of Urology, Glasgow Royal Infirmary, UK, 3. Dept of Urogynaecology, St Thomas' Hospital, London, UK, 4. Dept of Urology, Western General Hospital, Edinburgh, UK, 5. Dept of Urology, Royal Bournemouth Hospital, UK SEASONAL VARIATION IN URINARY FREQUENCY, NOCTURIA, AND OTHER LOWER URINARY TRACT SYMPTOMS IN MEN AND WOMEN Hypothesis / aims of study At a population level there are small seasonal effects on the prevalence of clinically relevant lower urinary tract storage symptoms [1], and a significant interaction with overactive bladder treatment response [2]. However, the effect of temperature variation on clinical assessment of lower urinary tract symptoms has not been explored. The aim of this study was to assess the association between atmospheric temperature, bladder diary variables, symptom severity, and urodynamic parameters in men and women with lower urinary tract symptoms. Study design, materials and methods Data were collected at two urodynamic units, Centre 1 situated at 55°52′N, equivalent to Moscow, and Centre 2 at 51°30′N, equivalent to Rotterdam, both with maritime temperate climates (Köppen classification Cfb). Consecutive men and women referred for evaluation were asked to complete both a 3 day frequency-volume chart, and a standardised lower urinary tract symptom and quality of life questionnaire (International Prostate Symptoms Score for men, and King’s Health Questionnaire for women), before undergoing free uroflowmetry, and where indicated, multichannel saline cystometry. Local mean monthly temperatures for each centre were extracted from national meteorological records. -

Lower Urinary Tract Symptoms Should Be Queried When Initiating Sodium Glucose Co- Transporter 2 Inhibitors
Kidney360 Publish Ahead of Print, published on February 3, 2021 as doi:10.34067/KID.0000472021 Lower urinary tract symptoms should be queried when initiating Sodium Glucose Co- Transporter 2 inhibitors Nicolas Krepostman and Holly Kramer 1Departments of Medicine and 2Public Health Sciences, Loyola University Chicago. Maywood, IL Corresponding Author: Holly Kramer MD MPH Loyola University Chicago 2160 S. First Avenue Maywood, IL 60153 Fax 708-216-8296 Office 708-327-9039 Email: [email protected] 1 Copyright 2021 by American Society of Nephrology. The sodium-glucose co-transporter 2 inhibitors (SGLT2i) reduce risk of both macrovascular (myocardial infractions and stroke) (1) and microvascular events (progression of chronic kidney disease) (2) in persons with type 2 diabetes. The beneficial effects of SGLT2i are derived from a cascade of effects subsequent to inhibition of glucose reabsorption in the S1 segment of the proximal tubule. Clinical trials have shown that SGLT2i reduce the absolute risk of kidney failure by 35% relative to placebo (95% CI 54%, 81%).(2) Thus, SGLT2i may be one of the most important interventions provided for adults at high risk for kidney failure. With any intervention, side effects and adverse effects must be considered in order to identify patients appropriate for the intervention and ensure that treated patients are educated regarding potential side effects and the appropriate coping mechanisms for bothersome side effects. For the SGLT2i drug class, adverse events includes hypoglycemia, ketoacidosis, volume depletion (especially when combined with loop diuretics), and genital urinary infections.(3-6) Other important side effects that are not life threatening but nevertheless bothersome are lower urinary tract symptoms (LUTS). -
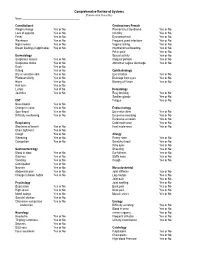
Comprehensive Review of Systems (Please Circle Yes Or No) Name: ______
Comprehensive Review of Systems (Please circle Yes or No) Name: __________________________________________ Constitutional Genitourinary Female Weight change Yes or No Premenstrual Syndrome Yes or No Loss of appetite Yes or No Infertility Yes or No Fever Yes or No Dysmenorrheal Yes or No Weakness Yes or No Frequent yeast infections Yes or No Night sweats Yes or No Vaginal itching Yes or No Breast feeding (if applicable) Yes or No Intermenstrual bleeding Yes or No Pelvic pain Yes or No Dermatology Sexual activity Yes or No Suspicious lesions Yes or No Irregular periods Yes or No Suspicious moles Yes or No Abnormal vaginal discharge Yes or No Rash Yes or No Itching Yes or No Ophthalmology Dry or sensitive skin Yes or No Eye irritation Yes or No Photosensitivity Yes or No Drainage from eyes Yes or No Hives Yes or No Blurring of Vision Yes or No Hair loss Yes or No Lumps Yes of No Hematology Jaundice Yes or No Easy bruising Yes or No Swollen glands Yes or No ENT Fatigue Yes or No Nose bleeds Yes or No Change in voice Yes or No Endocrinology Sore throat Yes or No Excessive thirst Yes or No Difficulty swallowing Yes or No Excessive sweating Yes or No Excessive urination Yes or No Respiratory Cold intolerance Yes or No Shortness of breath Yes or No Heat intolerance Yes or No Chest tightness Yes or No Cough Yes or No Allergy Wheezing Yes or No Runny nose Yes or No Congestion Yes or No Scratchy throat Yes or No Itchy eyes Yes or No Gastroenterology Sneezing Yes or No Blood in stool Yes or No Ear fullness Yes or No Diarrhea Yes or No Stuffy nose -

Urinary Incontinence in Women
Urinary Incontinence in Women National Kidney and Urologic Diseases Information Clearinghouse Millions of women experience involuntary stroke, multiple sclerosis, and physical loss of urine called urinary incontinence problems associated with aging. (UI). Some women may lose a few drops of urine while running or coughing. Others Older women experience UI more often National than younger women. But incontinence Institute of may feel a strong, sudden urge to urinate Diabetes and just before losing a large amount of urine. is not inevitable with age. UI is a medical Digestive problem. Your doctor or nurse can help and Kidney Many women experience both symptoms. Diseases UI can be slightly bothersome or totally you find a solution. No single treatment debilitating. For some women, the risk of works for everyone, but many women can NATIONAL find improvement without surgery. INSTITUTES public embarrassment keeps them from OF HEALTH enjoying many activities with their family Incontinence occurs because of problems and friends. Urine loss can also occur dur with muscles and nerves that help to hold ing sexual activity and cause tremendous or release urine. The body stores urine— emotional distress. water and wastes removed by the kidneys— Women experience UI twice as often as in the bladder, a balloon-like organ. The men. Pregnancy and childbirth, meno bladder connects to the urethra, the tube pause, and the structure of the female uri through which urine leaves the body. nary tract account for this difference. But During urination, muscles in the wall of both women and men can become inconti the bladder contract, forcing urine out of nent from neurologic injury, birth defects, the bladder and into the urethra. -

Overactive Bladder Syndrome Management and Treatment Options Janine Arnold Nicholas Mcleod Ruban Thani-Gasalam Prem Rashid
CLINICAL Overactive bladder syndrome Management and treatment options Janine Arnold Nicholas McLeod Ruban Thani-Gasalam Prem Rashid When compared with demographically matched Background controls, patients with OBS have:10,11 Overactive bladder syndrome is a symptom-based clinical diagnosis. It is • significantly less work productivity characterised by urinary urgency, frequency and nocturia, with or without urge • less sexual satisfaction and more erectile urinary incontinence. These symptoms can often be managed in the primary care dysfunction setting. • higher rates of depressive symptoms Objective • significantly poorer mental health This article provides a review on overactive bladder syndrome and provides advice • poorer quality of sleep. on management for the general practitioner. Postmenopausal women with urge incontinence Discussion have a significantly higher risk of falling and Overactive bladder syndrome can have a significant effect on quality of life, and sustaining a fracture than women without urge affects 12–17% of the population. Prevalence increases with age. The management incontinence.4 of overactive bladder syndrome involves exclusion of underlying pathology. First line treatment includes lifestyle interventions, pelvic floor exercises, bladder Causes training and antimuscarinic agents. Failure of conservative management The symptoms of OBS have many potential causes necessitates urology referral. Second line therapies are more invasive, and include and contributing factors. Normal storage of urine botulinum toxin, neuromodulation or surgical interventions such as augmentation is dependent on spinal reflex mechanisms that cystoplasty or urinary diversion. activate sympathetic and somatic pathways to the Keywords urethral outlet and tonic inhibitory systems in the overactive urinary bladder; urological diseases; urinary incontinence brain that suppress the parasympathetic excitatory outflow to the urinary bladder.4 The normal bladder fills like a compliant balloon, with pressure lower than urethral resistance. -

Voiding Dysfunction
Voiding Dysfunction .. ! 1. Symptomatology and terminology of voiding dysfunction 2. International prostatic symptom scores (IPSS) 3. Hematuria : definition and causes 4. Investigation for patient with hematuria Voiding Dysfunction AB CDE E (Sign & Symptom) GH AB GHI J ! JADK KLLCJ G MNOHEDED LUTS (Lower Urinary Tract Symptom) CDE LUTS G Terminology ISGH B TLUIVNE J UMNMNA NE M J B LD W N D LUTS (lower urinary tract symptom Irritative symptom Obstructive symptom Frequency Weak stream Nocturia Urinary hesitancy Urgency Intermittency Dysuria Postvoid dribbling Straining Acute and chronic urinary Retention Interruption of the stream Sense of residual urine 1 Symptomatology and terminology of voiding dysfunction Frequency KJDE IVE GHJJDEGHC ED BH MNaJJ I K NMbD LK 5-6 f DE g D f LG 300-400 cc. KJDEGIC W N D - Polyuria !E K !Bf ID D 2000 ./ LGICL IJGH WDW N J TOEWDHUIE OEIJLO (Diabetes Insipidus) OE ELI L GH OHfUM I jW N - Decreased bladder capacity GgGHUMN IKG ID D IKEE J D (Partial cystectomy), g Neurogenic bladder - Decreased functional capacity ! !E IKELLIDI D GH GJ M IK (irritation) ID M cystitis OENDIG jELUMNI KJDEW N Nocturia KJDEGHI !BfME O L GHI!NEWN J f MNUD Nocturnal frequency LOHE!BfKJN WDI 2 f DEO M l Na LUIVNE l I GH J frequency E NIE U - Frequency GHI !BfISE g WDG nocturia GICGHI GHIOHE J psychogenic IG - Nocturia without frequency ELI MNaGHIV congestive heart failure G peripheral edema IOHE L ED supine UMN intravascular volume I H!Bf - Nocturia MN EC renal concentrating -

Review of Systems
Review of Systems Check if you currently have or recently have had any of the following problems or concerns GENERAL CV (HEART) o Vomiting GU (URINARY MALE) o Fever o Difficulty breathing o Yellowish skin color o Dysuria o Chills o Near fainting o Gas o Hematuria o Sweats o Chest pain of o Abdominal pain o Discharge discomfort o Anorexia o Racing/skipping o Abdominal bloating o Urinary frequency heart beats o Fatigue o Fatigue o Hemorrhoids o Urinary urgency o Weakness o Lightheadedness o Diarrhea o Blood in urine o Malaise o Shortness of breath o Change in bowel o Inability to empty with exertion habits bladder o Weight Loss o Palpitations o Constipation o Kidney pain o Sleep Disorder o Swelling of o Dark tarry stools o Trouble starting hands/feet urinary stream EYES o Difficulty breathing o Bloody stools o Painful urination while laying down o Vision loss-1 eye o Fainting GU (URINARY FEMALE) ○ Inability to control bladder o Double Vision o Leg cramps with o Foul urinary o Unusual urinary exertion discharge color o Eye irritation o Blush discoloration o Blood in urine o Nocturia of lips or nails o Vision loss-both eyes o Weight gain o Urinary frequency o Incontinence o Blurring RESP (LUNGS) o Inability to empty o Genital sores bladder o Eye pain o Sleep disturbance o Urinary urgency o Decreased libido due to breathing o Halos o Cough o Kidney pain o Erectile dysfunction o Discharge o Shortness of breath o Trouble starting MUSCLES AND JOINTS urinary stream o Light sensitivity o Coughing up blood o Painful urination ○ Muscle cramps ENT -

Diseases and Disorders of the Urinary System
Chapter 10 Diseases and Disorders of the Urinary System Learning Objectives After studying this chapter, you should be able to L Describe the anatomy and the functions of kidneys, nephrons, ureters, urinary bladder, and urethra L Identify the etiology, signs and symptoms, diagnostic tests, and treatment for acute kidney injury and other acute and inflammatory diseases of the urinary system L Know the etiology, and describe the signs and symptoms, diagnostic tests, and treatment of urinary tract infections L Identify the etiology, signs and symptoms, diagnostic tests, and treatment for chronic kidney disease, hypertensive kidney disease, diabetic nephropathy, nephrotic syndrome, end-stage renal disease, and other chronic diseases of the urinary system L Describe kidney dialysis L Recognize the etiology, signs and symptoms, and modes of treat- Histopathology of kidney showing ment for renal cell carcinoma, Wilm’s tumor, and bladder cancer nodular glomerulosclerosis characteristic of diabetes mellitus. (Courtesy of L Describe common congenital disorders of the urinary system the Centers for Disease Control and Prevention/Dr. Edwin P. Wing, Jr., 1974) L Describe common age-related diseases of the urinary system Fact or Fiction? Kidney stones occur only in the kidneys. Fiction: Kidney stones may form anywhere within the urinary system, but they usually form in the renal pelvis or calyces of the kidney and they can lodge in the ureters. 198 M10_ZELM4744_08_SE_C10.indd 198 04/04/14 3:20 PM Disease Chronicle What’s in a Name? Many anatomical structures once bore the names of the scientists who first discovered them. Recently anatomists have revised anatomical nomenclature and we no longer formally name organs after scientists. -

Name Chapter 29: Alterations of Renal and Urinary Tract Function I. Urinary Tract Obstruction • Urinary Tract Obstruction Is
PATHOPHYSIOLOGY Name Chapter 29: Alterations of Renal and Urinary Tract Function I. Urinary Tract Obstruction Urinary tract obstruction is interference with the flow of urine at any site along the urinary tract. o Could be caused by many factors, including kidney stones, an enlarged prostate gland, or urethral strictures. Obstructive uropathy - anatomic changes in the urinary system caused by obstruction. o Severity is based on location, completeness, and duration of blockage, whether one or both sides of the urinary tract is involved, and the cause. A. Upper Urinary Tract Obstruction Blockage affecting flow through structures above the bladder. Causes dilation of the ureter (hydroureter); renal pelvis, calyces, and the proximal renal parenchyma (hydronephrosis); or all of these (ureterohydronephrosis). Pathophysiology: o Sustained dilation leads to enlargement and fibrosis of portions of the nephron tubule system. o The distal tubules are affected first followed by the proximal tubules. o This decreases the kidney's ability to concentrate urine, causing an increase in urine volume. o The affected kidney is unable to conserve sodium, bicarbonate, and water or to excrete hydrogen or potassium, leading to metabolic acidosis and dehydration. o The glomeruli are damaged later in the process due to increased hydrostatic pressure in the Bowman’s capsule. o This decreases the glomerular filtration rate. o As glomerular damage becomes extreme, urine volume decreases and oligouria occurs. o Irreversible damage occurs after about 4 weeks of obstruction. Compensatory hypertrophy of the opposite kidney occurs to partially offset loss of function of the obstructed kidney (or if one kidney is removed). Postobstructive diuresis – high urine output that follows relief of the obstruction.