Acid–Base Problems in Diabetic Ketoacidosis Kamel S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Body Fluid Compartments Dr Sunita Mittal
Body fluid compartments Dr Sunita Mittal Learning Objectives To learn: ▪ Composition of body fluid compartments. ▪ Differences of various body fluid compartments. ▪Molarity, Equivalence,Osmolarity-Osmolality, Osmotic pressure and Tonicity of substances ▪ Effect of dehydration and overhydration on body fluids Why is this knowledge important? ▪To understand various changes in body fluid compartments, we should understand normal configuration of body fluids. Total Body Water (TBW) Water is 60% by body weight (42 L in an adult of 70 kg - a major part of body). Water content varies in different body organs & tissues, Distribution of TBW in various fluid compartments Total Body Water (TBW) Volume (60% bw) ________________________________________________________________ Intracellular Fluid Compartment Extracellular Fluid Compartment (40%) (20%) _______________________________________ Extra Vascular Comp Intra Vascular Comp (15%) (Plasma ) (05%) Electrolytes distribution in body fluid compartments Intracellular fluid comp.mEq/L Extracellular fluid comp.mEq/L Major Anions Major Cation Major Anions + HPO4- - Major Cation K Cl- Proteins - Na+ HCO3- A set ‘Terminology’ is required to understand change of volume &/or ionic conc of various body fluid compartments. Molarity Definition Example Equivalence Osmolarity Osmolarity is total no. of osmotically active solute particles (the particles which attract water to it) per 1 L of solvent - Osm/L. Example- Osmolarity and Osmolality? Osmolarity is total no. of osmotically active solute particles per 1 L of solvent - Osm/L Osmolality is total no. of osmotically active solute particles per 1 Kg of solvent - Osm/Kg Osmosis Tendency of water to move passively, across a semi-permeable membrane, separating two fluids of different osmolarity is referred to as ‘Osmosis’. Osmotic Pressure Osmotic pressure is the pressure, applied to stop the flow of solvent molecules from low osmolarity to a compartment of high osmolarity, separated through a semi-permeable membrane. -

ISPAD Clinical Practice Consensus Guidelines 2018: Diabetic Ketoacidosis and the Hyperglycem
Received: 11 April 2018 Accepted: 31 May 2018 DOI: 10.1111/pedi.12701 ISPAD CLINICAL PRACTICE CONSENSUS GUIDELINES ISPAD Clinical Practice Consensus Guidelines 2018: Diabetic ketoacidosis and the hyperglycemic hyperosmolar state Joseph I. Wolfsdorf1 | Nicole Glaser2 | Michael Agus1,3 | Maria Fritsch4 | Ragnar Hanas5 | Arleta Rewers6 | Mark A. Sperling7 | Ethel Codner8 1Division of Endocrinology, Boston Children's Hospital, Boston, Massachusetts 2Department of Pediatrics, Section of Endocrinology, University of California, Davis School of Medicine, Sacramento, California 3Division of Critical Care Medicine, Boston Children's Hospital, Boston, Massachusetts 4Department of Pediatric and Adolescent Medicine, Medical University of Vienna, Vienna, Austria 5Department of Pediatrics, NU Hospital Group, Uddevalla and Sahlgrenska Academy, Gothenburg University, Uddevalla, Sweden 6Department of Pediatrics, School of Medicine, University of Colorado, Aurora, Colorado 7Division of Endocrinology, Diabetes and Metabolism, Department of Pediatrics, Icahn School of Medicine at Mount Sinai, New York, New York 8Institute of Maternal and Child Research, School of Medicine, University of Chile, Santiago, Chile Correspondence Joseph I. Wolfsdorf, Division of Endocrinology, Boston Children's Hospital, 300 Longwood Avenue, Boston, MA. Email: [email protected] 1 | SUMMARY OF WHAT IS Risk factors for DKA in newly diagnosed patients include younger NEW/DIFFERENT age, delayed diagnosis, lower socioeconomic status, and residence in a country with a low prevalence of type 1 diabetes mellitus (T1DM). Recommendations concerning fluid management have been modified Risk factors for DKA in patients with known diabetes include to reflect recent findings from a randomized controlled clinical trial omission of insulin for various reasons, limited access to medical ser- showing no difference in cerebral injury in patients rehydrated at dif- vices, and unrecognized interruption of insulin delivery in patients ferent rates with either 0.45% or 0.9% saline. -

ACS/ASE Medical Student Core Curriculum Acid-Base Balance
ACS/ASE Medical Student Core Curriculum Acid-Base Balance ACID-BASE BALANCE Epidemiology/Pathophysiology Understanding the physiology of acid-base homeostasis is important to the surgeon. The two acid-base buffer systems in the human body are the metabolic system (kidneys) and the respiratory system (lungs). The simultaneous equilibrium reactions that take place to maintain normal acid-base balance are: H" HCO* ↔ H CO ↔ H O l CO g To classify the type of disturbance, a blood gas (preferably arterial) and basic metabolic panel must be obtained. A basic understanding of normal acid-base buffer physiology is required to understand alterations in these labs. The normal pH of human blood is 7.40 (7.35-7.45). This number is tightly regulated by the two buffer systems mentioned above. The lungs contain carbonic anhydrase which is capable of converting carbonic acid to water and CO2. The respiratory response results in an alteration to ventilation which allows acid to be retained or expelled as CO2. Therefore, bradypnea will result in respiratory acidosis while tachypnea will result in respiratory alkalosis. The respiratory buffer system is fast acting, resulting in respiratory compensation within 30 minutes and taking approximately 12 to 24 hours to reach equilibrium. The renal metabolic response results in alterations in bicarbonate excretion. This system is more time consuming and can typically takes at least three to five days to reach equilibrium. Five primary classifications of acid-base imbalance: • Metabolic acidosis • Metabolic alkalosis • Respiratory acidosis • Respiratory alkalosis • Mixed acid-base disturbance It is important to remember that more than one of the above processes can be present in a patient at any given time. -

The Basic Principles of Acid-Base Regulation*
The Basic Principles of Acid-Base Regulation* ORHAN MUREN, M.D. Associate Professor of Medicine and Anesthesiology, Medical College of Virginia, Health Sciences Division of Virginia Commonwealth University, Richmond, Virginia Acid-base homeostasis refers to those chemical In normal people, the concentration of H• is and physiological processes which maintain the hy approximately 40 nanomoles ( n moles) per liter of drogen ion (H•) activity in body fluids at the levels plasma. One nanomole equals 10-9 moles. However, compatible with life and normal functioning. This is it would be more correct to indicate the thermo an enormous task due to the fact that reactions which dynamic activities rather than the concentrations, produce H• and reactions which consume H• are the two being related as follows: continously occurring in human beings. On one hand there is acid production (fixed activity ----.- = activity coefficient and volatile acid) and on the other hand acid elimi concentration nation (fixed and volatile acid). Normally in a given time, such as in a day, acid elimination is equal At infinite dilution the activity coefficient is to acid production. Whenever there is imbalance equal to one. However, in concentrations in body between input and output, acid-base disturbances fluids, it is much less than one. The pH meter will occur. electrode responds to hydrogen ion activity and not Many biochemical processes require optimum concentration. However, it is customary to work in H• ion concentration. Changes in H• concentration concentrations, and values for the different equilib markedly affect the catalytic activity of enzymes. rium constants are adjusted accordingly, as indicated Myocardial and muscular contraction, vascular tone, by a prime after a symbol such as K'. -

Acid–Base Problems in Diabetic Ketoacidosis Kamel S
The new england journal of medicine Review Article Disorders of Fluids and Electrolytes Julie R. Ingelfinger, M.D., Editor Acid–Base Problems in Diabetic Ketoacidosis Kamel S. Kamel, M.D., and Mitchell L. Halperin, M.D. From the Renal Division, St. Michael’s his review focuses on three issues facing clinicians who care for Hospital and University of Toronto, and patients with diabetic ketoacidosis; all of the issues are related to acid–base Keenan Research Center, Li Ka Shing Knowledge Institute of St. Michael’s disorders. The first issue is the use of the plasma anion gap and the calculation Hospital, University of Toronto, Toronto. T of the ratio of the change in this gap to the change in the concentration of plasma Address reprint requests to Dr. Halperin bicarbonate in these patients; the second concerns the administration of sodium bi- at the Department of Medicine, Univer- sity of Toronto Keenan Research Center, carbonate; and the third is the possible contribution of intracellular acidosis to the Li Ka Shing Knowledge Institute of St. development of cerebral edema, particularly in children with diabetic ketoacidosis. In Michael’s Hospital, 30 Bond St., Rm. this article, we examine the available data and attempt to integrate the data with 408, Toronto, ON M5B 1W8, Canada, or at mitchell . halperin@ utoronto . ca. principles of physiology and metabolic regulation and provide clinical guidance. N Engl J Med 2015;372:546-54. DOI: 10.1056/NEJMra1207788 Plasma Bicarbonate and the Plasma Anion Gap Copyright © 2015 Massachusetts Medical Society. The accumulation of ketoacids in the extracellular fluid leads to a loss of bicarbonate anions and a gain of ketoacid anions. -

Ketoalkalosis: Masked Presentation of Diabetic Ketoacidosis with Literature Review
Case Report J Endocrinol Metab. 2017;7(6):194-196 Ketoalkalosis: Masked Presentation of Diabetic Ketoacidosis With Literature Review Vinod Kumara, Sushant M. Nanavatia, c, Fnu Komala, Luis Carlos Ortiza, Namrata Paula, Manhedar Kumarb, Patrick Michaela, Monisha Singhal Abstract sis would be masqueraded by alkalosis. We present a unique case of 25 years old female with DKA and alkalemia. Most dreaded complication in type 1 diabetes mellitus remains dia- betic ketoacidosis (DKA): plasma blood glucose > 250 mg/dL, serum Case Report bicarbonate < 18 mEq/L, anion gap metabolic acidosis and ketosis. Insulin deficiency with high levels of glucagon and stress hormones causing ketogenesis in liver, elevated lipolysis in peripheral tissues, and A 25-year-old female with type 1 diabetes mellitus presented increased free fatty acids contribute the formation of ketones leading with complaints of intractable vomiting, generalized weakness to metabolic acidosis. And hence DKA is also termed as ketoacidosis. and abdominal pain. Six hours prior to arrival to emergency Unusually, patients with diuretic use, alkali ingestion, intractable vom- department (ED), she started to experience diffuse abdominal iting, or hypercortisolism may present with alkalemia in DKA. Con- pain around periumbilical area and subsequently started in- traction (Metabolic) Alkalosis masquerades metabolic acidosis with tractable non-bilious vomiting. At home, she was prescribed anion gap and low to normal bicarbonate that uncovers on provision of to insulin detemir 25 units once a day along with insulin aspart intravenous fluids. We present a case of a 25-year-old female with DKA 6 units along with three meals. She stated of adherent to insu- presenting with intractable vomiting, alkalotic pH and high anion gap. -

It Is Chloride Depletion Alkalosis, Not Contraction Alkalosis
SCIENCE IN RENAL MEDICINE www.jasn.org It Is Chloride Depletion Alkalosis, Not Contraction Alkalosis Robert G. Luke and John H. Galla Department of Medicine, University of Cincinnati College of Medicine, Cincinnati, Ohio ABSTRACT Maintenance of metabolic alkalosis generated by chloride depletion is often attributed aspiration, chloruretic diuretics, NaNO3 to volume contraction. In balance and clearance studies in rats and humans, we infusion (an effect of un-reabsorbable showed that chloride repletion in the face of persisting alkali loading, volume anions), and prior hypercapnia (post- contraction, and potassium and sodium depletion completely corrects alkalosis hypercapnic CDA) were all used to gen- by a renal mechanism. Nephron segment studies strongly suggest the corrective erate CDA. These studies establish that 2 response is orchestrated in the collecting duct, which has several transporters Cl repletion by NaCl or KCl—but not integral to acid-base regulation, the most important of which is pendrin, a luminal replacement of Na+ and K+ losses without 2 2 Cl/HCO3 exchanger. Chloride depletion alkalosis should replace the notion of Cl —fully corrects CDA in the mainte- contraction alkalosis. nance phase. The issue of the specific role of ECF volume depletion was not re- J Am Soc Nephrol 23: 204–207, 2012. doi: 10.1681/ASN.2011070720 solved at this time. To separate chloride from volume re- pletion, we first studied rats with selective Chloridedepletionisthecommonestofthe identical to that in the plasma of the dogs CDA produced by peritoneal dialysis 3 three major causes of metabolic alkalosis; with stable alkalemia. These isometric in- against NaHCO3 and a normal serum po- theothersrelatetopotassiumdepletion/ fusions completely corrected alkalosis by tassium concentration. -
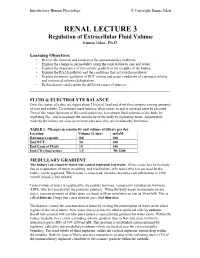
RENAL LECTURE 3 Regulation of Extracellular Fluid Volume Emma Jakoi, Ph.D
Introductory Human Physiology © Copyright Emma Jakoi RENAL LECTURE 3 Regulation of Extracellular Fluid Volume Emma Jakoi, Ph.D. Learning Objectives • Review the function and location of the juxtamedullary nephrons. • Explain the change in permeability along the renal tubule to ions and water. • Explain the importance of the osmotic gradient in the medulla of the kidney. • Explain the RAAS pathway and the conditions that activate this pathway. • Explain hormonal regulation of ECF volume and under conditions of expanded volume and contracted volume (dehydration • Define diuresis and explain the different causes of diuresis. _____________________________________________________________ FLUID & ELECTROLYTE BALANCE Over the course of a day, we ingest about 2 liters of food and drink that contains varying amounts of ions and solutes. To maintain mass balance, what comes in and is not used must be excreted. Two of the major functions of the renal system are to maintain fluid volumes of the body by regulating Na+ and to maintain the osmolarity of the body by regulating water. Adjustments made by the kidney are slow (over hours) because they are mediated by hormones. TABLE 1. Changes in osmolarity and volume of filtrate per day Location Volume (L/day) mOsM Bowman's capsule 180 300 End PCT 54 300 End Loop of Henle 18 100 End CD (final urine) 1.5 50-1200 MEDULLARY GRADIENT The kidney can conserve water but cannot replenish lost water. Of the water lost by the body due to evaporation of sweat, breathing, and metabolism, only water which is excreted by the kidney can be regulated. When water is conserved, the urine becomes concentrated up to 1200 mOsM (blood is 300 mOsM). -

Episode 146 DKA Recognition & ED Management
• Negative urine ketones should not be used to rule out diabetic ketoacidosis, as urine tests measure the presence of acetoacetate, but not β-hydroxybutyrate A β-hydroxybutyrate level > 1.5 mmol/L has a sensitivity of 98- Episode 146 DKA Recognition & Management 100% and specificity of 78.6-93.3% for the diagnosis of DKA in diabetic patients presenting to the ED with elevated serum glucose levels. With Drs Mel Baimel, Leeor Sommer, Bourke Tillman Prepared by Winny Li, September 2020 Clinical Pearl: Many patients with DKA present with some degree of abdominal pain. Severe abdominal pain with only mild The Difficulty in Diagnosing Diabetic Ketoacidosis (DKA) ketoacidosis argues against DKA as the cause. When in doubt about need for an abdominal imaging, resuscitate the patient There are no definitive criteria for the diagnosis of DKA according first, and perform serial abdominal examinations. Have a low to the 2018 Canadian DKA Guidelines. As such, it is important to threshold to image if the ketoacidosis improves but the patient have a low threshold to consider the diagnosis in any diabetic continues to be symptomatic or clinically worsens. patient who presents with polyuria, polydipsia, hyperpnea, abdominal pain/nausea/vomiting and altered level of awareness. While most patients with DKA will have the triad of hyperglycemia, anion gap metabolic acidosis and ketonemia, Severity categorization of DKA there are exceptions: • DKA patients can have a normal glucose (euglycemic DKA) • DKA patients can have a normal pH and a normal bicarbonate (normal VBG) in the context of ketoacidosis plus metabolic alkalosis as a result of vomiting and/or the triggering illness 1 Differentiating DKA from Hyperglycemic Hyperosmolar DKA lab work-up Syndrome (HHS) DKA work-up should include CBC, electrolytes, extended electrolytes, creatinine, BUN, albumin, VBG, lactate, serum ketones, as well as consideration for: • BhCG (trigger of DKA) • ECG/Trop (only if ischemia suggested in history) • Cultures, UA etc. -

Metabolic Alkalosis
METABOLIC ALKALOSIS Ricardo M Heguilén MD Unidad de Nefrología. Hospital Juan A Fernández Universidad de Buenos Aires. ARGENTINA The problem in perspective Metabolic alkalosis (MA) is one of the most common electrolyte disturbances observed in hospitalized patients, and accounts for nearly half of all acid-base disorders. Metabolic alkalosis, when severe, represents a serious and life-threatening medical condition with mortality rates ranging from 50% for pHs higher than 7.55 to almost 80% at pHs in excess of 7.65 • Severe alkalosis predisposes to refractory arrhythmias by reducing coronary blood flow. • Tissue perfusion is severely compromised as a consequence of diffuse arteriolar constriction and by decreasing the cerebral blood flow MA may lead to altered consciousness and seizures. • In patients with poor respiratory status, the normal compensatory decrease in the ventilatory response to MA may cause severe hypoxemia. • Alkalosis leads to hypokalemia which can cause arrhythmias, neuromuscular dysfunction and by increasing the production of ammonia can precipitate hepatic encephalopathy in patients with preexistent chronic liver disease. • In MA hydrogen ions are released from the anionic binding sites of albumin, calcium is then taken up resulting in a dramatic reduction in the serum concentration of ionized calcium. Definitions Metabolic alkalosis refers to a condition that leads to a primary increase in serum - - bicarbonate concentration ([HCO3 ]) occurring as a consequence of a gain in HCO3 to, or a loss of H+ from the body. MA manifests as alkalemia (pH >7.40). As compensatory mechanism, MA yields to alveolar hypoventilation with the consequent increase in arterial carbon dioxide tension (PaCO2). This compensatory rise in PaCO2, minimize the change in pH that might otherwise occur. -

Clinical and Pathophysiologic Spectrum of Acquired Distal Renal Tubular Acidosis
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Kidney International, Vol. 20 (1981), PP. 389—396 Clinical and pathophysiologic spectrum of acquired distal renal tubular acidosis DANIEL C. BATLLE, JOHN T. SEHY, MELVIN K. ROSEMAN, JOSE A. L. ARRUDA, and NEIL A. KURTZMAN Sections of Nephrology, University of Illinois Abraham Lincoln School of Medicine, and the Veterans Administration West Side Hospital in Chicago, Illinois Clinical and pathophysiologic spectrum of acquired distal renal tubular derniers malades indique que Ia pompe était capable de secréter des acidosis. Urinary acidification was studied in nine patients with hyper- ions hydrogene dans des conditions de stimulation maximales. Cette chioremic metabolic acidosis. The aim of this study was to investigate modalité est previsible chez les malades qui ont un deficit sélectif et the mechanism(s) of impaired distal acidification by the systematic isolC d'aldostérone et qui sont aussi capables d'abaisser Ic pH de leur administration of sodium sulfate and neutral phosphate. No impairment urine en presence d'une acidose metabolique systémique. La modalité of proximal acidification was apparent because all patients had a d'acidification particuliCre du dernier malade qui Ctait en méme temps fractional bicarbonate excretion below 5% at plasma bicarbonate con- hyperkaliemique peut Ctre expliquee par un mécanisme dépendant de Ia centrations above 22 mEq/liter. All patients except two were unable to difference de potentiel. Cette situation peut étre reconnue par Ia lower urine pH below 5.5 despite systemic metabolic acidosis. The two constatation d'un désordre portant a La fois sur Ia secretion de ions patients who lowered urine pH normally were hyperkalemic and had hydrogene et celle de potassium. -
Hyperglycemic Emergencies in Adults Canadian Journal of Diabetes
Can J Diabetes 42 (2018) S109–S114 Contents lists available at ScienceDirect Canadian Journal of Diabetes journal homepage: www.canadianjournalofdiabetes.com 2018 Clinical Practice Guidelines Hyperglycemic Emergencies in Adults Diabetes Canada Clinical Practice Guidelines Expert Committee Jeannette Goguen MD, MEd, FRCPC, Jeremy Gilbert MD, FRCPC insulin deficiency, hyperglycemia causes urinary losses of water and KEY MESSAGES electrolytes (sodium, potassium, chloride) and the resultant extra- cellular fluid volume (ECFV) depletion. Potassium is shifted out of • Diabetic ketoacidosis and hyperosmolar hyperglycemic state should be sus- cells, and ketoacidosis occurs as a result of elevated glucagon levels pected in people who have diabetes and are ill. If either diabetic ketoaci- and insulin deficiency (in the case of type 1 diabetes). There may dosis or hyperosmolar hyperglycemic state is diagnosed, precipitating factors must be sought and treated. also be high catecholamine levels suppressing insulin release (in • Diabetic ketoacidosis and hyperosmolar hyperglycemic state are medical the case of type 2 diabetes). In DKA, ketoacidosis is prominent while, emergencies that require treatment and monitoring for multiple meta- in HHS, the main features are ECFV depletion and hyperosmolarity. bolic abnormalities and vigilance for complications. HHS is the preferred term to describe this condition as opposed to A normal or mildly elevated blood glucose level does not rule out dia- • hyperosmolar nonketotic coma (HONKC) since less than one-third betic ketoacidosis in certain conditions, such as pregnancy or with SGLT2 inhibitor use. of people with HHS actually present with a coma (1). • Diabetic ketoacidosis requires intravenous insulin administration (0.1 units/ Risk factors for DKA include new diagnosis of diabetes melli- kg/h) for resolution.