Innovations in Tamil Nadu
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1. ABOUT GANDHIGRAM TRUST with the Vision of 'Holistic Village
1. ABOUT GANDHIGRAM TRUST With the vision of ‘Holistic village development as envisioned by Mahatma Gandhi the Gandhigram Trust began its operation in the year 1947 with the blessings of Mahatma Gandhi by his ardent disciples. Dr. T.S. Soundram and Dr. G. Ramachandran started with handful of dedicated volunteers and with few institutions now Gandhigram grown to a height like a banyan tree, having many institution giving so much of employment and rehabilitations. Now it is stepping in to the 71st year of existence Village development denotes overall development of rural areas with a view to improve the quality of life of the rural people. It encompasses development of agriculture and its allied activities, cottage and small scale industries, traditional crafts, creation of socio-economic infrastrucuture, proper usage of rural human resources and improvement in community services and facilities. To attain this holistic village development, Gandhigram Trust empowers the rural people through quality education, physical and social welfare measures and knowledge and skills required for income generation. Thus, we have five dimensions of activities to realize the vision of the Founders. Thus, 1. SOCIAL WELFARE Through Sowbhagya Illam at Gandhigram and Dr. Soundram Illam at Sivasailam Social welfare measures of child protection and development of vulnerable children are being are taken care of Kasturba Sevikashram Special Higher Secondary School imparts education and life skills to school dropout girls, widows, divorcees and destitute women. 2. EDUCATION Empowering the rural people through quality education from Kindergarten level to higher secondary school level is taken care by the educational institutions which Gandhigram and at Sivasailam. -

Registration Form (PDF, 108KB)
About The Institute The Gandhigram Rural Institute is one of the unique higher education institutions functioning with a vision of promotion of a casteless and classless society through instruction, research and extension. Based on Mahatma Gandhi’s revolutionary concept of `Nai Talim’ system of education Dr.T.S.Soundram and Dr.G.Ramachandram sculptured this institute in 1956. The Work of the Institute invited national attention and the Government of India (Ministry of Education), on the recommendation of the University Grants Commission, conferred the status of a Deemed University on the institute under section (3) of the UGC Act of 1956, on 3rd August, 1976. Today it has emerged as a renowned university both at national and international level for its remarkable contribution to rural education and its services. The Institute was accredited with Five Star Status by NAAC, in February 2002 and re-accredited with `A’ grade by NAAC in 2010. MHRD, assessing all the Deemed Universities in India, awarded `A’ grade to the Institute in 2013 About The Department The Department of Home Science was established in the year 1956. The Department offers B.Sc and M.Sc programmes under Choice Based Credit System, besides M.Phil and Ph.D programmes in Home Science. The department has also undertaken many research projects funded by DST, UGC, ICSSR and TNSCS&T (at National level) and American Association of Physicians of Indian Origin (AAPI) USA, Bernard Van Leer Foundation, Netherland, (at International Level) and has research collaboration with Leibniz University Hannover, Germany. The Department has organized several conferences, seminars and workshops at national level. -

The Gandhigram Rural Institute Deemed University Prospectus
The Gandhigram Rural Institute Deemed University (Ministry of Human Resource Development, Govt. of India) Gandhigram - 624 302 Dindigul District, Tamil Nadu - India Prospectus 2016-2017 Library Physics Lab XXXII Convocation Language Lab Computer Lab Athletic Chemistry Lab PROSPECTUS 2016-2017 THE GANDHIGRAM RURAL INSTITUTE – DEEMED UNIVERSITY (Ministry of Human Resource Development, Govt. of India) GANDHIGRAM – 624 302 DINDIGUL DISTRICT, TAMIL NADU - INDIA Salient Features of Gandhigram Rural Institute INFRASTRUCTURE AND FACULTIES Sprawling campus of over 200 acres nestling in a green valley of the beautiful Sirumalai range Highly qualified teaching staff Excellent academic atmosphere AMINITIES Well-equipped laboratory, library and computer facilities Wi-fi facility in the entire campus and browsing facility in hostels Well- maintained separate hostels for boys and girls CURRICULAM Choice Based Credit System (CBCS) of curriculum Core courses in Hindi, Malayalam and French for Under-Graduate Programmes Mandatory course in Computer Applications for all Programmes Provision for add-on courses and Career-oriented Programmes Physical Education and Yoga for all students Soft Skills at UG and PG to enhance employment potential Implementation of National Knowledge Network EXTENSION Credit-laden Village Placement Programme (VPP) for UG and PG Programmes Emphasis on experiential learning Extension as integral part of the curriculum Value- based education National Service Scheme (NSS) for all students Shanti Sena for moulding the -

Unpaid Dividend-17-18-I3 (PDF)
Note: This sheet is applicable for uploading the particulars related to the unclaimed and unpaid amount pending with company. Make sure that the details are in accordance with the information already provided in e-form IEPF-2 CIN/BCIN L72200KA1999PLC025564 Prefill Company/Bank Name MINDTREE LIMITED Date Of AGM(DD-MON-YYYY) 17-JUL-2018 Sum of unpaid and unclaimed dividend 696104.00 Sum of interest on matured debentures 0.00 Sum of matured deposit 0.00 Sum of interest on matured deposit 0.00 Sum of matured debentures 0.00 Sum of interest on application money due for refund 0.00 Sum of application money due for refund 0.00 Redemption amount of preference shares 0.00 Sales proceed for fractional shares 0.00 Validate Clear Proposed Date of Investor First Investor Middle Investor Last Father/Husband Father/Husband Father/Husband Last DP Id-Client Id- Amount Address Country State District Pin Code Folio Number Investment Type transfer to IEPF Name Name Name First Name Middle Name Name Account Number transferred (DD-MON-YYYY) 49/2 4TH CROSS 5TH BLOCK MIND00000000AZ00 Amount for unclaimed and A ANAND NA KORAMANGALA BANGALORE INDIA Karnataka 560095 54.00 23-May-2025 2539 unpaid dividend KARNATAKA 69 I FLOOR SANJEEVAPPA LAYOUT MIND00000000AZ00 Amount for unclaimed and A ANTONY FELIX NA MEG COLONY JAIBHARATH NAGAR INDIA Karnataka 560033 72.00 23-May-2025 2646 unpaid dividend BANGALORE ROOM NO 6 G 15 M L CAMP 12044700-01567454- Amount for unclaimed and A ARUNCHETTIYAR AKCHETTIYAR INDIA Maharashtra 400019 10.00 23-May-2025 MATUNGA MUMBAI MI00 unpaid -

Report 1-15 Pages.P65
Inclusive Development The expression inclusive development has become part of the vocabulary in recent times. Economists and politicians all over the world talk about inclusive development. This idea evolved in the 1970s as a reaction to the social exclusion of a large group of unemployed people in the industrialized nations of Western Europe who could not participate in the normal activities of the society. Since then the concept of inclusion has gradually crossed the European borders and reached the developing nations of the world with the efforts of the United Nations agencies by the nineties. Thanks to the founders Dr.T.S. Soundram and Dr. G. Ramachandran Gandhigram has been engaged in inclusive development since its inception in 1947. Our main activities cover the fields of Social Welfare, Health and Hygiene, Education and Employment Generation. Some 1240 SHGs have been formed by us since 1990s and they are grouped in 37 Federations. Apart from microcredit, some 3000 SHG women have become individual entrepreneurs. There are 56 Joint ventures of SHGs in different trades. SHGs of women are managing distribution of water supply in many village Panchayats. They are also engaged in solid and liquid waste management in many villages. Under a project titled Scheme of Funds for Regeneration of Traditional Industries (SFURTI) 700 artisans engaged in collection, cultivation, semi processing and marketing of herbal plants and herbal based finished products have benefitted financially. They have learnt how to collect plants in a scientific manner without destroying the nature. The project was successfully implemented in four blocks under Dindigul and Theni District and completed in March 2012. -

Documentary Production and Cultural Studies Film 3202 (Code 43813)
Study Abroad India: Documentary Production and Cultural Studies Film 3202 (code 43813) (4 hours; 3 credits), International Documentary Production TVRA 4849 (code 3513) Undergraduate Study Abroad India TVRA 7749x (code 3421) Graduate Study Abroad India Faculty Program Director: Professor Annette Danto Brooklyn College Film Department 2900 Bedford Avenue, 217 West End Building Tel: 718-951-5664 [email protected]; [email protected] This 21 day course will offer a meaningful combination of lectures, field trips, production work and sightseeing. Students will learn about South Indian cultures, religions, history and cinema, with excursions to major cultural, historical and religious sights. Hyderabad’s Ramoji Film City and Mahendra Ecole Central will provide the setting for studying documentary production within a South Indian context. Through a series of classroom lectures and screenings students will receive a comprehensive introduction to South Indian cinema, with an emphasis on documentary. CUNY students will work collaboratively with Mahendra Ecole Central students on the preproduction, production and post production of short documentary projects. The production component of the course will involve on-going collaboration between CUNY students and Mahendra Ecole Centrale/Ramoji Film City students. This will include: tech sessions, writing assignments, group exercises, research and development of a documentary topic, and the production and post production of that documentary. Students with little or no background in documentary production will learn some of the basic technical skills required to operate digital cameras, sound equipment, as well as how to structure a short documentary. All students will be expected to participate as crew members. Those with a preference for non-technical crew positions will be able to work as: writers, script supervisors, production coordinators and assistants. -

Unpaid Dividend-17-18-I2 (PDF)
Note: This sheet is applicable for uploading the particulars related to the unclaimed and unpaid amount pending with company. Make sure that the details are in accordance with the information already provided in e-form IEPF-2 CIN/BCIN L72200KA1999PLC025564 Prefill Company/Bank Name MINDTREE LIMITED Date Of AGM(DD-MON-YYYY) 17-JUL-2018 Sum of unpaid and unclaimed dividend 709686.00 Sum of interest on matured debentures 0.00 Sum of matured deposit 0.00 Sum of interest on matured deposit 0.00 Sum of matured debentures 0.00 Sum of interest on application money due for refund 0.00 Sum of application money due for refund 0.00 Redemption amount of preference shares 0.00 Sales proceed for fractional shares 0.00 Validate Clear Proposed Date of Investor First Investor Middle Investor Last Father/Husband Father/Husband Father/Husband Last DP Id-Client Id- Amount Address Country State District Pin Code Folio Number Investment Type transfer to IEPF Name Name Name First Name Middle Name Name Account Number transferred (DD-MON-YYYY) 49/2 4TH CROSS 5TH BLOCK MIND00000000AZ00 Amount for unclaimed and A ANAND NA KORAMANGALA BANGALORE INDIA Karnataka 560095 54.00 21-Feb-2025 2539 unpaid dividend KARNATAKA 69 I FLOOR SANJEEVAPPA LAYOUT MIND00000000AZ00 Amount for unclaimed and A ANTONY FELIX NA MEG COLONY JAIBHARATH NAGAR INDIA Karnataka 560033 72.00 21-Feb-2025 2646 unpaid dividend BANGALORE IN300394-13455837- Amount for unclaimed and A BASHKARAN NA 40 OLD MUNCHIFF COURT STREETINDIA Tamil Nadu 637001 10.00 21-Feb-2025 0000 unpaid dividend NO 198 ANUGRAHA -
PGDHPE Prospectus
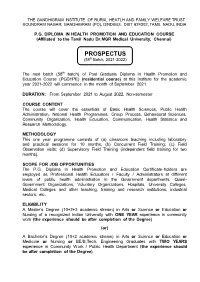
THE GANDHIGRAM INSTITUTE OF RURAL HEATLH AND FAMILY WELFARE TRUST SOUNDRAM NAGAR, GANDHIGRAM (PO), DINDIGUL DIST 624302, TAMIL NADU, INDIA P.G. DIPLOMA IN HEALTH PROMOTION AND EDUCATION COURSE (Affiliated to the Tamil Nadu Dr.MGR Medical University, Chennai) PROSPECTUS (58th Batch, 2021-2022) The next batch (58th batch) of Post Graduate Diploma in Health Promotion and Education Course (PGDHPE) (residential course) at this Institute for the academic year 2021-2022 will commence in the month of September 2021. DURATION: From September 2021 to August 2022, Non-semester COURSE CONTENT The course will cover the essentials of Basic Health Sciences, Public Health Administration, National Health Programmes, Group Process, Behavioural Sciences, Community Organization, Health Education, Communication, Health Statistics and Research Methodology. METHODOLOGY This one year programme consists of (a) classroom teaching including laboratory and practical sessions for 10 months; (b) Concurrent Field Training; (c) Field Observation visits; (d) Supervisory Field Training (independent field training for two months). SCOPE FOR JOB OPPORTUNITIES The P.G. Diploma in Health Promotion and Education Certificate-holders are employed as Professional Health Educators / Faculty / Administrators at different levels of public health administration in the Government departments, Quasi- Government Organizations, Voluntary Organizations, Hospitals, University Colleges, Medical Colleges and other teaching, training and research institutions, industrial sectors, etc. ELIGIBILITY A Master’s Degree (10+2+3 academic stream) in Arts or Science or Education or Nursing of a recognized Indian University with ONE YEAR experience in community work (the experience should be after completion of the Degree) (or) A Bachelor’s Degree (10+2 academic stream) in Arts or Science or Education or Medicine or Nursing or BE/B.Tech. -

Private Schools Fee Determination Committee Chennai-600 006 - Fees Fixed for the Year 2013-2016 - District: Dindugal Sl
PRIVATE SCHOOLS FEE DETERMINATION COMMITTEE CHENNAI-600 006 - FEES FIXED FOR THE YEAR 2013-2016 - DISTRICT: DINDUGAL SL. SCHOOL HEARING SCHOOL NAME & ADDRESS YEAR LKG UKG I II III IV V VI VII VIII IX X XI XII NO. CODE DATE 2013 - 14 4500 4500 6550 6550 6550 6550 6550 - - - - - - - BRINDAVAN NURSERY & PRIMARY SCHOOL 1 090004 KALLIMANDAYAM 10-5-13 2014 - 15 4950 4950 7205 7205 7205 7205 7205 - - - - - - - ODDANCHATRAM DINDIGUL 2015 - 16 5445 5445 7926 7926 7926 7926 7926 - - - - - - - DANISH NURSERY & 2013 - 14 4800 4800 5800 5800 5800 5800 5800 - - - - - - - PRIMARY SCHOOL NO:211 MAIN ROAD 2 090007 10-5-13 2014 - 15 5280 5280 6380 6380 6380 6380 6380 - - - - - - - POOMBARAI KOADAIKANAL DINDIGUL 2015 - 16 5808 5808 7018 7018 7018 7018 7018 - - - - - - - Karunai Dhan Nursery & 2013 - 14 4800 4800 5700 5700 5700 5700 5700 - - - - - - - Primary School 12.06.2B/6, E.B. 3 090010 10-05-2013 2014 - 15 5280 5280 6270 6270 6270 6270 6270 - - - - - - - Colony, Nilakottai, Dindigul Distr 2015 - 16 5808 5808 6897 6897 6897 6897 6897 - - - - - - - 2013 - 14 3700 3700 4500 4500 4500 4500 4500 - - - - - - - Kennedy Nursery & Primary School 4 090011 13-03-13 2014 - 15 4070 4070 4950 4950 4950 4950 4950 - - - - - - - Nagal Nursery Dindigul-3 2015 - 16 4477 4477 5445 5445 5445 5445 5445 - - - - - - - PRAKK FOUNDATION 2013 - 14 5400 5400 5800 5800 5800 5800 5800 - - - - - - - NURSERY & PRIMARY SCHOOL 5 090012 HOLIDAY HOME 10-5-13 2014 - 15 5940 5940 6380 6380 6380 6380 6380 - - - - - - - GOLF ROAD KODAIKANAL DINDIGUL 2015 - 16 6534 6534 7018 7018 7018 7018 7018 - - - - - - - Shri. Gurumuki 2013 - 14 5700 5700 6500 6500 6500 6500 6500 - - - - - - - Vidhyasshram Nursery & Primary School 6 090014 1395, Pudhu Kapilliya 10-05-2013 2014 - 15 6270 6270 7150 7150 7150 7150 7150 - - - - - - - Patti, Thadicombu Via, Dindigul District. -

Unpaid Dividend-15-16-I4 (PDF)
Note: This sheet is applicable for uploading the particulars related to the unclaimed and unpaid amount pending with company. Make sure that the details are in accordance with the information already provided in e-form IEPF-2 CIN/BCIN L72200KA1999PLC025564 Prefill Company/Bank Name MINDTREE LIMITED Date Of AGM(DD-MON-YYYY) 17-JUL-2018 Sum of unpaid and unclaimed dividend 759188.00 Sum of interest on matured debentures 0.00 Sum of matured deposit 0.00 Sum of interest on matured deposit 0.00 Sum of matured debentures 0.00 Sum of interest on application money due for refund 0.00 Sum of application money due for refund 0.00 Redemption amount of preference shares 0.00 Sales proceed for fractional shares 0.00 Validate Clear Proposed Date of Investor First Investor Middle Investor Last Father/Husband Father/Husband Father/Husband Last DP Id-Client Id- Amount Address Country State District Pin Code Folio Number Investment Type transfer to IEPF Name Name Name First Name Middle Name Name Account Number transferred (DD-MON-YYYY) 49/2 4TH CROSS 5TH BLOCK KORAMANGALA BANGALORE MIND00000000AZ00 Amount for unclaimed and A ANAND NA KARNATAKA INDIA Karnataka 560095 2539 unpaid dividend 72.00 28-Apr-2023 69 I FLOOR SANJEEVAPPA LAYOUT MEG COLONY JAIBHARATH NAGAR MIND00000000AZ00 Amount for unclaimed and A ANTONY FELIX NA BANGALORE INDIA Karnataka 560033 2646 unpaid dividend 72.00 28-Apr-2023 NO 198 ANUGRAHA II FLOOR OLD POLICE STATION ROAD MIND00000000AZ00 Amount for unclaimed and A G SUDHINDRA NA THYAGARAJANAGAR BANGALORE INDIA Karnataka 560028 2723 unpaid -

Diploma in Medical Laboratory Technology
The Gandhigram Institute of Rural Health & Family Welfare Trust Ambathurai Rs. Gandhigram PO, Dindigul District, Tamil Nadu Diploma in Medical Laboratory Technology Introduction: GIRH&FWT was established in the year 1964 by Dr.(Mrs.) T.S .Soundaram and Dr.G.Ramachandran, with support from Government of Tamil Nadu, Government of India and Ford Foundation. About the Course: This course is recognized by Government of Tamil Nadu as per G.O. Ms.No.122 /PME / 03-04-2012. Objectives: At the end of the training programme, the trainee would develop and enforce a professional code of conduct. At the end of the course the trainees would be able to perform all the pathological, serological and Bio-Chemical examination of all the samples efficiently. Salient features of the course: Intensive training given in basic laboratory techniques Well equipped laboratory in Pathology, Microbiology and Bio-Chemistry are available in the Institute. Guest lectures by renowned medical persons. Observation cum skill development hospital postings in reputed hospitals for a period of one month Co-education Separate hostel facilities are available for male and female candidates. Mess facility is also available for hostel students. Admission Details No. of Seats : 15 Duration : 2 years Eligibility : Candidates who have passed +2 with science subject a) Physics, Chemistry Botany and zoology b) Physics, Chemistry, Biology with both in theory and practical with minimum 35% marks and with not less than 50% aggregate in the above subjects and 45% aggregate for SC/ST/SC-A candidates. Age : 17 years completed less than 35 years as on 30th June of the academic year Photocopy of certificates to be attached along with the application 1. -

DR. NAME Father's /Husband Name
TAMILNADU STATE VETERINARY COUNCIL, CHENNAI-600035. DRAFT ELECTORAL ROLL-2013 SVPR Roll. Father's /Husband TNSVC SVPR SVPR PAGE.N No: DR. NAME Name ADDRESS Reg.No: YEAR Sl.NO: O: 44 /183-3, PUSHPAGAM EAST YMR 1 SAIRABANU S. P. SAMSUDEEN PATTI, DINDIGUL -624001. 2 2002 2 1 25 / 32A, KUNJAN VILAI, MANIKATTIPOTTAL (P.O.), 2 RAMESH S. R.SUYAMBU NAGERCOIL 629 501 3 2002 3 1 27, CHELLA PERUMAL ST., K.G.SUBRAMANIA SHOLINGHUR 631 102, VELLORE 3 VIJAYAKUMAR K. S. N DISTRICT 4 2002 4 1 # 220, METTU STREET, SAMPATH K.R.KARUNAKAR MANSION, NATHAM P.O., 4 SAMPATH K. AN CHENGALPATTU 603 001 5 2002 5 2 156D/163B, Subasri Nagar, Extn.I, 5 KAMALRAJ V. D. VENKATESAN Porur, Chennai - 600 0116 6 2002 6 2 ANAIPALAYAM (P.O.) ANDAGALUR GATE (VIA), RASIPURAM (TK), 6 LAVANYA K. A.KAILASAM NAMAKKAL DT., 637 401 7 2002 7 2 KEELA RADHA VEEDI, MUDUKULATHUR 623 704 , 7 KANNAN ALPADI A. T.T.ALPADI RAMANATHAPURAM DT., 8 2002 8 2 102, ARANI KOOT ROAD, PADMAVATHY A. W/o. A. KAMALA CHEYYAR - 604407 8 KANNAN THIRUVANNAMALAI DIST. 9 2002 9 3 122, MAIN ROAD. OLAGADAM 638 9 GANAPATHI RAJ M. R.MURUGESAN 314, ERODE DISTRICT 10 2002 10 3 OLD NO. 8,9 NEW NO. 5, RATHINAM R.GOVINDARAJA STREET, FIRST LANE, NEAR FIVE 10 DHANARAJ G. N CORNER, COIMBATORE-641001. 11 2002 11 3 15 / 1, MURUGA BHAVANAM, FIRST STREET, KAKKAN NAGAR, SURESH I. PALAYAMKOTTAI 11 S. IYYAPILLAI 627 353 12 2002 12 3 NO.17 & 19, FOURTH STREET, GOVINDA SWAMY NAGAR, KANDANCHAVADI, MADRAS 600 12 SARASWATHI M.