Toxicological Profile for Carbon Monoxide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Sanitization: Concentration, Temperature, and Exposure Time
Sanitization: Concentration, Temperature, and Exposure Time Did you know? According to the CDC, contaminated equipment is one of the top five risk factors that contribute to foodborne illnesses. Food contact surfaces in your establishment must be cleaned and sanitized. This can be done either by heating an object to a high enough temperature to kill harmful micro-organisms or it can be treated with a chemical sanitizing compound. 1. Heat Sanitization: Allowing a food contact surface to be exposed to high heat for a designated period of time will sanitize the surface. An acceptable method of hot water sanitizing is by utilizing the three compartment sink. The final step of the wash, rinse, and sanitizing procedure is immersion of the object in water with a temperature of at least 170°F for no less than 30 seconds. The most common method of hot water sanitizing takes place in the final rinse cycle of dishwashing machines. Water temperature must be at least 180°F, but not greater than 200°F. At temperatures greater than 200°F, water vaporizes into steam before sanitization can occur. It is important to note that the surface temperature of the object being sanitized must be at 160°F for a long enough time to kill the bacteria. 2. Chemical Sanitization: Sanitizing is also achieved through the use of chemical compounds capable of destroying disease causing bacteria. Common sanitizers are chlorine (bleach), iodine, and quaternary ammonium. Chemical sanitizers have found widespread acceptance in the food service industry. These compounds are regulated by the U.S. Environmental Protection Agency and consequently require labeling with the word “Sanitizer.” The labeling should also include what concentration to use, data on minimum effective uses and warnings of possible health hazards. -

The Effect of Carbon Monoxide Sources and Meteorologic Changes in Carbon Monoxide Intoxication: a Retrospective Study
Cilt: 3 Sayı: 1 Şubat 2020 / Vol: 3 Issue: 1 February 2020 https://dergipark.org.tr/tr/pub/actamednicomedia Research Article | Araştırma Makalesi THE EFFECT OF CARBON MONOXIDE SOURCES AND METEOROLOGIC CHANGES IN CARBON MONOXIDE INTOXICATION: A RETROSPECTIVE STUDY KARBONMONOKSİT KAYNAKLARININ VE METEOROLOJİK DEĞİŞİKLİKLERİN KARBONMONOKSİT ZEHİRLENMELERİNE ETKİSİ: RETROSPEKTİF ÇALIŞMA Duygu Yılmaz1, Umut Yücel Çavuş2, Sinan Yıldırım3, Bahar Gülcay Çat Bakır4*, Gözde Besi Tetik5, Onur Evren Yılmaz6, Mehtap Kaynakçı Bayram7 1Manisa Turgutlu State Hospital, Department of Emergency Medicine, Manisa, Turkey. 2Ankara Education and Research Hospital, Department of Emergency Medicine, Ankara, Turkey. 3Çanakkale State Hospital, Department of Emergency Medicine, Çanakkale,Turkey. 4Mersin City Education and Research Hospital, Department of Emergency Medicine, Mersin, Turkey. 5Gaziantep Şehitkamil State Hospital, Department of Emergency Medicine, Gaziantep, Turkey. 6Medical Park Hospital, Department of Plastic and Reconstructive Surgery, İzmir, Turkey. 7Kayseri City Education and Research Hospital, Department of Emergency Medicine, Kayseri, Turkey. ABSTRACT ÖZ Objective: Carbon monoxide (CO) poisoning is frequently seen in Amaç: Karbonmonoksit (CO) zehirlenmelerine, özellikle soğuk emergency departments (ED) especially in cold weather. We havalarda olmak üzere acil servis birimlerinde sıklıkla karşılaşılır. investigated the relationship of some of the meteorological factors Çalışmamızda, bazı meteorolojik faktörlerin CO zehirlenmesinin with the sources -

Sea Surface Temperatures on the Great Barrier Reef: a Contribution to the Study of Coral Bleaching
GREAT BARRIER REEF MARINE PARK AUTHORITY RESEARCH PUBLICATION No. 57 Sea Surface Temperatures on the Great Barrier Reef: a Contribution to the Study of Coral Bleaching JM Lough 551.460 109943 1999 RESEARCH PUBLICATION No. 57 Sea Surface Temperatures on the Great Barrier Reef: a Contribution to the Study of Coral Bleaching JM Lough Australian Institute of Marine Science AUSTRALIAN INSTITUTE GREAT BARRIER REEF OF MARINE SCIENCE MARINE PARK AUTHORITY A REPORT TO THE GREAT BARRIER REEF MARINE PARK AUTHORITY O Great Barrier Reef Marine Park Authority, Australian Institute of Marine Science 1999 ISSN 1037-1508 ISBN 0 642 23069 2 This work is copyright. Apart from any use as permitted under the Copyright Act 1968, no part may be reproduced by any process without prior written permission from the Great Barrier Reef Marine Park Authority and the Australian Institute of Marine Science. Requests and inquiries concerning reproduction and rights should be addressed to the Director, Information Support Group, Great Barrier Reef Marine Park Authority, PO Box 1379, Townsville Qld 4810. The opinions expressed in this document are not necessarily those of the Great Barrier Reef Marine Park Authority. Accuracy in calculations, figures, tables, names, quotations, references etc. is the complete responsibility of the author. National Library of Australia Cataloguing-in-Publication data: Lough, J. M. Sea surface temperatures on the Great Barrier Reef : a contribution to the study of coral bleaching. Bibliography. ISBN 0 642 23069 2. 1. Ocean temperature - Queensland - Great Barrier Reef. 2. Corals - Queensland - Great Barrier Reef - Effect of temperature on. 3. Coral reef ecology - Australia - Great Barrier Reef (Qld.) - Effect of temperature on. -

Asphyxia Neonatorum
CLINICAL REVIEW Asphyxia Neonatorum Raul C. Banagale, MD, and Steven M. Donn, MD Ann Arbor, Michigan Various biochemical and structural changes affecting the newborn’s well being develop as a result of perinatal asphyxia. Central nervous system ab normalities are frequent complications with high mortality and morbidity. Cardiac compromise may lead to dysrhythmias and cardiogenic shock. Coagulopathy in the form of disseminated intravascular coagulation or mas sive pulmonary hemorrhage are potentially lethal complications. Necrotizing enterocolitis, acute renal failure, and endocrine problems affecting fluid elec trolyte balance are likely to occur. Even the adrenal glands and pancreas are vulnerable to perinatal oxygen deprivation. The best form of management appears to be anticipation, early identification, and prevention of potential obstetrical-neonatal problems. Every effort should be made to carry out ef fective resuscitation measures on the depressed infant at the time of delivery. erinatal asphyxia produces a wide diversity of in molecules brought into the alveoli inadequately com Pjury in the newborn. Severe birth asphyxia, evi pensate for the uptake by the blood, causing decreases denced by Apgar scores of three or less at one minute, in alveolar oxygen pressure (P02), arterial P02 (Pa02) develops not only in the preterm but also in the term and arterial oxygen saturation. Correspondingly, arte and post-term infant. The knowledge encompassing rial carbon dioxide pressure (PaC02) rises because the the causes, detection, diagnosis, and management of insufficient ventilation cannot expel the volume of the clinical entities resulting from perinatal oxygen carbon dioxide that is added to the alveoli by the pul deprivation has been further enriched by investigators monary capillary blood. -

Respiratory Physiology - Part B Experimental Determination of Anatomical Dead Space Value (Human 9 - Version Sept
Comp. Vert. Physiology- BI 244 Respiratory Physiology - Part B Experimental Determination of Anatomical Dead Space Value (Human 9 - Version Sept. 10, 2013) [This version has been modified to also serve as a tutorial in how to run HUMAN's artificial organs] Part of the respiratory physiology computer simulation work for this week allows you to obtain a hand-on feeling for the effects of anatomical dead space on alveolar ventilation. The functional importance of dead space can explored via employing HUMAN's artificial respirator to vary the respiration rate and tidal volume. DEAD SPACE DETERMINATION Introduction The lack of unidirectional respiratory medium flow in non-avian air ventilators creates the existence of an anatomical dead space. The anatomical dead space of an air ventilator is a fixed volume not normally under physiological control. However, the relative importance of dead space is adjustable by appropriate respiratory maneuvers. For example, recall the use by panting animals of their dead space to reduce a potentially harmful respiratory alkalosis while hyperventilating. In general, for any given level of lung ventilation, the fraction of the tidal volume attributed to dead space will affect the resulting level of alveolar ventilation, and therefore the efficiency (in terms of gas exchange) of that ventilation. [You should, of course, refresh your knowledge of total lung ventilation, tidal volume alveolar ventilation.] Your objective here is to observe the effects of a constant "unknown" dead space on resulting alveolar ventilation by respiring the model at a variety of tidal volume-frequency combinations. You are then asked to calculate the functional dead space based on the data you collect. -

Pulmonary Barotrauma During Hypoxia in a Diver While Underwater
POLISH HYPERBARIC RESEARCH 2(71)2020 Journal of Polish Hyperbaric Medicine and Technology Society PULMONARY BAROTRAUMA DURING HYPOXIA IN A DIVER WHILE UNDERWATER Brunon Kierznikowicz, Władysław Wolański, Romuald Olszański Institute of Maritime and Tropical Medicine of the Military Medical Academy, Gdynia, Poland ABSTRACT The article describes a diver performing a dive at small depths in a dry suit, breathing from a single-stage apparatus placed on his back. As a result of training deficiencies, the diver began breathing from inside the suit, which led to hypoxia and subsequent uncontrolled ascent. Upon returning to the surface, the diver developed neurological symptoms based on which a diagnosis of pulmonary barotrauma was made. The diver was successfully treated with therapeutic recompression-decompression. Keywords: diving, accident, hypoxia, pulmonary barotrauma. ARTICLE INFO PolHypRes 2020 Vol. 71 Issue 2 pp. 45 – 50 ISSN: 1734-7009 eISSN: 2084-0535 Casuistic (case description) article DOI: 10.2478/phr-2020-0009 Pages: 6, figures: 0, tables: 1 Originally published in the Naval Health Service Yearbook 1977-1978 page www of the periodical: www.phr.net.pl Acceptance for print in PHR: 27.10.2019 r. Publisher Polish Hyperbaric Medicine and Technology Society 2020 Vol. 71 Issue 2 INTRODUCTION that he suddenly experienced an "impact" from an increased amount of air flowing into his lungs during In recent years, we can observe a continuous inhalation. Fearing a lung injury, he immediately pulled the dynamic development of diving technology. At the same mouthpiece out of his mouth and started breathing air time, the spectrum of works carried out by scuba divers for from inside the suit for about 2 minutes. -

Lecture 3. the Basic Properties of the Natural Atmosphere 1. Composition
Lecture 3. The basic properties of the natural atmosphere Objectives: 1. Composition of air. 2. Pressure. 3. Temperature. 4. Density. 5. Concentration. Mole. Mixing ratio. 6. Gas laws. 7. Dry air and moist air. Readings: Turco: p.11-27, 38-43, 366-367, 490-492; Brimblecombe: p. 1-5 1. Composition of air. The word atmosphere derives from the Greek atmo (vapor) and spherios (sphere). The Earth’s atmosphere is a mixture of gases that we call air. Air usually contains a number of small particles (atmospheric aerosols), clouds of condensed water, and ice cloud. NOTE : The atmosphere is a thin veil of gases; if our planet were the size of an apple, its atmosphere would be thick as the apple peel. Some 80% of the mass of the atmosphere is within 10 km of the surface of the Earth, which has a diameter of about 12,742 km. The Earth’s atmosphere as a mixture of gases is characterized by pressure, temperature, and density which vary with altitude (will be discussed in Lecture 4). The atmosphere below about 100 km is called Homosphere. This part of the atmosphere consists of uniform mixtures of gases as illustrated in Table 3.1. 1 Table 3.1. The composition of air. Gases Fraction of air Constant gases Nitrogen, N2 78.08% Oxygen, O2 20.95% Argon, Ar 0.93% Neon, Ne 0.0018% Helium, He 0.0005% Krypton, Kr 0.00011% Xenon, Xe 0.000009% Variable gases Water vapor, H2O 4.0% (maximum, in the tropics) 0.00001% (minimum, at the South Pole) Carbon dioxide, CO2 0.0365% (increasing ~0.4% per year) Methane, CH4 ~0.00018% (increases due to agriculture) Hydrogen, H2 ~0.00006% Nitrous oxide, N2O ~0.00003% Carbon monoxide, CO ~0.000009% Ozone, O3 ~0.000001% - 0.0004% Fluorocarbon 12, CF2Cl2 ~0.00000005% Other gases 1% Oxygen 21% Nitrogen 78% 2 • Some gases in Table 3.1 are called constant gases because the ratio of the number of molecules for each gas and the total number of molecules of air do not change substantially from time to time or place to place. -

Temperature Relationships of Great Lakes Fishes: By
Temperature Relationships of Great Lakes Fishes: A Data Compilation by Donald A. Wismer ’ and Alan E. Christie Great Lakes Fishery Commission Special Publication No. 87-3 Citation: Wismer, D.A. and A.E. Christie. 1987. Temperature Relationships of Great Lakes Fishes: A Data Compilation. Great Lakes Fish. Comm. Spec. Pub. 87-3. 165 p. GREAT LAKES FISHERY COMMISSION 1451 Green Road Ann Arbor, Ml48105 USA July, 1987 1 Environmental Studies & Assessments Dept. Ontario Hydro 700 University Avenue, Location H10 F2 Toronto, Ontario M5G 1X6 Canada TABLE OF CONTENTS Page 1.0 INTRODUCTION 1 1.1 Purpose 1.2 Summary 1.3 Literature Review 1.4 Database Advantages and Limitations 2.0 METHODS 2 2.1 Species List 2 2.2 Database Design Considerations 2 2.3 Definition of Terms 3 3.0 DATABASE SUMMARY 9 3.1 Organization 9 3.2 Content 10 4.0 REFERENCES 18 5.0 FISH TEMPERATURE DATABASE 29 5.1 Abbreviations 29 LIST OF TABLES Page Great Lakes Fish Species and Types of Temperature Data 11 Alphabetical Listing of Reviewed Fish Species by 15 Common Name LIST OF FIGURES Page Diagram Showing Temperature Relations of Fish 5 1.0 INTRODUCTION 1.1 Purpose The purpose of this report is to compile a temperature database for Great Lakes fishes. The database was prepared to provide a basis for preliminary decisions concerning the siting, design, and environ- mental performance standards of new generating stations and appropriate mitigative approaches to resolve undesirable fish community interactions at existing generating stations. The contents of this document should also be useful to fisheries research and management agencies in the Great Lakes Basin. -

Carbon Monoxide Levels and Risks
Carbon Monoxide Levels and Risks CO Level Action CO Level Action 0.1 ppm Natural atmosphere level or clean air. 70-75 ppm Heart patients experience an increase in chest pain. Significant decrease in 1 ppm An increase of 1 ppm in the maximum dai- oxygen available to the myocardium/ ly one-hour exposure is associated with a heart (HbCO 10%). 0.96 percent increase in the risk of hospi- 100 ppm Headache, tiredness, dizziness, nausea talization from cardiovascular disease within 2 hrs of exposure. At 5 hrs, dam- among people over the age of 65. age to hearts and brains. (Lewey & Drabkin) (Circulation: Journal of the AHA, Sept, 2009) 200 ppm Healthy adults will have headache, nau- 3-7 ppm 6% increase in the rate of admission in sea at this level. hospitals of non-elderly for asthma. (L. Shep- pard et al.,Epidemiology, Jan 1999) NIOSH & OSHA recommend evacua- tion of the workplace at this level. 5-6 ppm Significant risk of low birth weight if exposed during last trimester - in a study 400 ppm Frontal headache within 1-2 hours—life of 125,573 pregnancies (Ritz & Yu, Environ. threatening within 3 hours. Health Perspectives, 1999). 500 ppm Concentration in a garage when a cold 9 ppm EPA and WHO maximum outdoor air lev- car is started in an open garage and el, all ages, (TWA, 8 hrs). Maximum allow- warmed up for 2 minutes. (Greiner, 1997) able indoor level (ASHRAE) 800 ppm Healthy adults will have nausea, dizzi- Lowest CO level producing significant ef- ness and convulsions within 45 fects on cardiac function (ST-segment minutes. -

INFLUENCE of TEMPERATURE on DIFFUSION and SORPTION of 237Np(V) THROUGH BENTONITE ENGINEERED BARRIERS
Clemson University TigerPrints All Theses Theses 5-2017 Influence of emperT ature on Diffusion and Sorption of 237Np(V) through Bentonite Engineered Barriers Rachel Nicole Pope Clemson University, [email protected] Follow this and additional works at: https://tigerprints.clemson.edu/all_theses Recommended Citation Pope, Rachel Nicole, "Influence of emperT ature on Diffusion and Sorption of 237Np(V) through Bentonite Engineered Barriers" (2017). All Theses. 2666. https://tigerprints.clemson.edu/all_theses/2666 This Thesis is brought to you for free and open access by the Theses at TigerPrints. It has been accepted for inclusion in All Theses by an authorized administrator of TigerPrints. For more information, please contact [email protected]. INFLUENCE OF TEMPERATURE ON DIFFUSION AND SORPTION OF 237Np(V) THROUGH BENTONITE ENGINEERED BARRIERS A Thesis Presented to the Graduate School of Clemson University In Partial Fulfillment of the Requirements for the Degree Master of Science Environmental Engineering and Earth Sciences by Rachel Nicole Pope May 2017 Accepted by: Dr. Brian A. Powell, Committee Chair Dr. Mark Schlautman Dr. Lindsay Shuller‐Nickles ABSTRACT Diffusion rates of 237Np(V), 3H, and 22Na through Na‐montmorillonite were studied under variable dry bulk density and temperature. Distribution coefficients were extrapolated for conservative tracers. Two sampling methods were implemented, and effects of each sampling method were compared. The first focused on an exchange of the lower concentration reservoir frequently while the second kept the lower concentration reservoir consistent. In both sampling methods, tritium diffusion coefficients decreased with an increase in dry bulk density and increased with an increase in temperature. Sodium diffusion rates followed the same trends as tritium with the exception of sorption phenomena. -
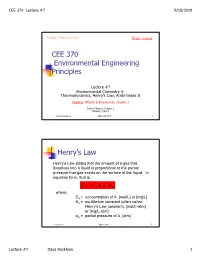
CEE 370 Environmental Engineering Principles Henry's
CEE 370 Lecture #7 9/18/2019 Updated: 18 September 2019 Print version CEE 370 Environmental Engineering Principles Lecture #7 Environmental Chemistry V: Thermodynamics, Henry’s Law, Acids-bases II Reading: Mihelcic & Zimmerman, Chapter 3 Davis & Masten, Chapter 2 Mihelcic, Chapt 3 David Reckhow CEE 370 L#7 1 Henry’s Law Henry's Law states that the amount of a gas that dissolves into a liquid is proportional to the partial pressure that gas exerts on the surface of the liquid. In equation form, that is: C AH = K p A where, CA = concentration of A, [mol/L] or [mg/L] KH = equilibrium constant (often called Henry's Law constant), [mol/L-atm] or [mg/L-atm] pA = partial pressure of A, [atm] David Reckhow CEE 370 L#7 2 Lecture #7 Dave Reckhow 1 CEE 370 Lecture #7 9/18/2019 Henry’s Law Constants Reaction Name Kh, mol/L-atm pKh = -log Kh -2 CO2(g) _ CO2(aq) Carbon 3.41 x 10 1.47 dioxide NH3(g) _ NH3(aq) Ammonia 57.6 -1.76 -1 H2S(g) _ H2S(aq) Hydrogen 1.02 x 10 0.99 sulfide -3 CH4(g) _ CH4(aq) Methane 1.50 x 10 2.82 -3 O2(g) _ O2(aq) Oxygen 1.26 x 10 2.90 David Reckhow CEE 370 L#7 3 Example: Solubility of O2 in Water Background Although the atmosphere we breathe is comprised of approximately 20.9 percent oxygen, oxygen is only slightly soluble in water. In addition, the solubility decreases as the temperature increases. -

Pressure Vs. Volume and Boyle's
Pressure vs. Volume and Boyle’s Law SCIENTIFIC Boyle’s Law Introduction In 1642 Evangelista Torricelli, who had worked as an assistant to Galileo, conducted a famous experiment demonstrating that the weight of air would support a column of mercury about 30 inches high in an inverted tube. Torricelli’s experiment provided the first measurement of the invisible pressure of air. Robert Boyle, a “skeptical chemist” working in England, was inspired by Torricelli’s experiment to measure the pressure of air when it was compressed or expanded. The results of Boyle’s experiments were published in 1662 and became essentially the first gas law—a mathematical equation describing the relationship between the volume and pressure of air. What is Boyle’s law and how can it be demonstrated? Concepts • Gas properties • Pressure • Boyle’s law • Kinetic-molecular theory Background Open end Robert Boyle built a simple apparatus to measure the relationship between the pressure and volume of air. The apparatus ∆h ∆h = 29.9 in. Hg consisted of a J-shaped glass tube that was Sealed end 1 sealed at one end and open to the atmosphere V2 = /2V1 Trapped air (V1) at the other end. A sample of air was trapped in the sealed end by pouring mercury into Mercury the tube (see Figure 1). In the beginning of (Hg) the experiment, the height of the mercury Figure 1. Figure 2. column was equal in the two sides of the tube. The pressure of the air trapped in the sealed end was equal to that of the surrounding air and equivalent to 29.9 inches (760 mm) of mercury.