Acremonium Mycetoma: a Case Report and Discussion
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Subcutaneous Phaeohyphomycosis Caused by Exophiala Salmonis
Case Report Clinical Microbiology Ann Lab Med 2012;32:438-441 http://dx.doi.org/10.3343/alm.2012.32.6.438 ISSN 2234-3806 • eISSN 2234-3814 Subcutaneous Phaeohyphomycosis Caused by Exophiala salmonis Young Ahn Yoon, M.D.1, Kyung Sun Park, M.D.1, Jang Ho Lee, M.T.1, Ki-Sun Sung, M.D.2, Chang-Seok Ki, M.D.1, and Nam Yong Lee, M.D.1 Departments of Laboratory Medicine and Genetics1, Orthopedic Surgery2, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea We report a case of subcutaneous infection in a 55-yr-old Korean diabetic patient who Received: June 18, 2012 presented with a cystic mass of the ankle. Black fungal colonies were observed after cul- Revision received: July 30, 2012 Accepted: September 12, 2012 turing on blood and Sabouraud dextrose agar. On microscopic observation, septated ellip- soidal or cylindrical conidia accumulating on an annellide were visualized after staining Corresponding author: Nam Yong Lee Department of Laboratory Medicine and with lactophenol cotton blue. The organism was identified as Exophiala salmonis by se- Genetics, Samsung Medical Center, quencing of the ribosomal DNA internal transcribed spacer region. Phaeohyphomycosis is 81 Irwon-ro, Gangnam-gu, Seoul 135-710, a heterogeneous group of mycotic infections caused by dematiaceous fungi and is com- Korea Tel: +82-2-3410–2706 monly associated with immunocompromised patients. The most common clinical mani- Fax: +82-2-3410–2719 festations of subcutaneous lesions are abscesses or cystic masses. To the best of our E-mail: [email protected] knowledge, this is the first reported case in Korea of subcutaneous phaeohyphomycosis caused by E. -

Exophiala Jeanselmei, with a Case Report and in Vitro Antifungal Susceptibility of the Species
UvA-DARE (Digital Academic Repository) Biodiversity, pathogenicity and antifungal susceptibility of Cladophialophora and relatives Badali, H. Publication date 2010 Link to publication Citation for published version (APA): Badali, H. (2010). Biodiversity, pathogenicity and antifungal susceptibility of Cladophialophora and relatives. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:02 Oct 2021 Chapter 6 The clinical spectrum of Exophiala jeanselmei, with a case report and in vitro antifungal susceptibility of the species H. Badali 1, 2, 3, M.J. Najafzadeh 1, 2, M. van Esbroeck 4, E. van den Enden 4, B. Tarazooie 1, J.F.G.M. Meis 5, G.S. de Hoog 1, 2 1CBS-KNAW Fungal Biodiversity Centre, Utrecht, The Netherlands, 2Institute of Biodiversity and Ecosystem Dynamics, University of Amsterdam, Amsterdam, The Netherlands, 3Department of Medical Mycology and Parasitology, School of Medicine/Molecular and Cell Biology Research Centre, Mazandaran University of Medical Sciences, Sari, Iran, 4Institute of Tropical Medicine, Nationalestraat 155, 2000 Antwerp, Belgium,5Department of Medical Microbiology and Infectious Diseases, Canisius Wilhelmina Hospital, Nijmegen, The Netherlands. -

Indoor Wet Cells As a Habitat for Melanized Fungi, Opportunistic
www.nature.com/scientificreports OPEN Indoor wet cells as a habitat for melanized fungi, opportunistic pathogens on humans and other Received: 23 June 2017 Accepted: 30 April 2018 vertebrates Published: xx xx xxxx Xiaofang Wang1,2, Wenying Cai1, A. H. G. Gerrits van den Ende3, Junmin Zhang1, Ting Xie4, Liyan Xi1,5, Xiqing Li1, Jiufeng Sun6 & Sybren de Hoog3,7,8,9 Indoor wet cells serve as an environmental reservoir for a wide diversity of melanized fungi. A total of 313 melanized fungi were isolated at fve locations in Guangzhou, China. Internal transcribed spacer (rDNA ITS) sequencing showed a preponderance of 27 species belonging to 10 genera; 64.22% (n = 201) were known as human opportunists in the orders Chaetothyriales and Venturiales, potentially causing cutaneous and sometimes deep infections. Knufa epidermidis was the most frequently encountered species in bathrooms (n = 26), while in kitchens Ochroconis musae (n = 14), Phialophora oxyspora (n = 12) and P. europaea (n = 10) were prevalent. Since the majority of species isolated are common agents of cutaneous infections and are rarely encountered in the natural environment, it is hypothesized that indoor facilities explain the previously enigmatic sources of infection by these organisms. Black yeast-like and other melanized fungi are frequently isolated from clinical specimens and are known as etiologic agents of a gamut of opportunistic infections, but for many species their natural habitat is unknown and hence the source and route of transmission remain enigmatic. Te majority of clinically relevant black yeast-like fungi belong to the order Chaetothyriales, while some belong to the Venturiales. Propagules are mostly hydro- philic1 and reluctantly dispersed by air, infections mostly being of traumatic origin. -

Superficial Fungal Infection
Infeksi jamur superfisial (mikosis superfisialis) R. Wahyuningsih Dep. Parasitologi FK UKI 31 Maret 2020 Klasifikasi mikosis superfisialis berdasarkan penyebab • Dermatofitosis • kandidiasis superfisialis • Infeksi Malassezia/panu M. Raquel Vieira, ESCMID Dermatofitosis • Infeksi jaringan keratin (kulit, kuku & rambut) oleh jamur filamen gol. dermatofita • genus dermatofita – Tricophyton, – Microsporum – Epidermophyton, • ± 10 spesies menyebabkan dermatofitosis pada manusia Asian incidence of the most common mycoses identified All values are percentages In Asia, T. rubrum and T. mentagrophytes are the most commonly isolated pathogens, causing tinea pedis and unguium, as is the case in Europe. Havlickova et al, Mycoses Dermatophytosis di Indonesia • Geofilik: M . gypseum • Zoofilik: M. canis • Antropofilik: – T. rubrum – T. concentricum – E. floccosum Patologi & organ terinfeksi Kuku kulit rambut Trichophyton + + + Microsporum + + + Epidermophyton + + - http://www.njmoldinspection.com/mycoses/moldinfections.html Dermatophytoses...... • Gejala klinik tergantung pada: • Lokalisasi infeksi • Respons imun pejamu • Spesies jamur • Lesi: karakteristik (ring worm) tetapi dalam kondisi imuno supresi menjadi tidak khas perlu pemeriksaan laboratorium Dermatofita & dermatofitosis T. rubrum: biakan. kapang, pigmen merah, mikrokonidia lonjong, tetesan air mata/anggur, makrokonidia seperti pinsil/cerutu . antropofilik, . kelainan kronik mis. • tinea kruris, onikomiksosis De Berker, N Engl J Med 2009;360:2108-16 Dermatofita & dermatofitosis M. canis -

Fusarium Subglutinans a New Eumycetoma Agent
Medical Mycology Case Reports 2 (2013) 128–131 Contents lists available at SciVerse ScienceDirect Medical Mycology Case Reports journal homepage: www.elsevier.com/locate/mmcr Fusarium subglutinans: A new eumycetoma agent$ Pablo Campos-Macías a, Roberto Arenas-Guzmán b, Francisca Hernández-Hernández c,n a Laboratorio de Microbiología, Facultad de Medicina, Universidad de Guanajuato, León, Guanajuato 37320, México b Sección de Micología, Hospital General Dr. Manuel Gea González, México D.F. 14080, México c Departamento de Microbiología y Parasitología, Facultad de Medicina, Universidad Nacional Autónoma de México, México D.F. 04510, México article info abstract Article history: Eumycetoma is a chronic subcutaneous mycosis mainly caused by Madurella spp. Fusarium opportunistic Received 31 May 2013 infections in humans are often caused by Fusarium solani and Fusarium oxysporum. We report a case of Received in revised form eumycetoma by F. subglutinans, diagnosed by clinical aspect and culture, and confirmed by PCR 20 June 2013 sequencing. The patient was successfully treated with oral itraconazole. To our knowledge, this is the Accepted 26 June 2013 second report of human infection and the first case of mycetoma by Fusarium subglutinans. & 2013 The Authors. Published by Elsevier B.V on behalf of International Society for Human and Animal Keywords: Mycology All rights reserved. Eumycetoma Mycetoma Fusarium subglutinans Itraconazole 1. Introduction eye infections [7,8], and infections of immunosuppressed patients [9]. To our knowledge, there had been only 1 case of Fusarium Mycetoma is an infectious, inflammatory and chronic disease subglutinans infection documented in the literature, a hyalohypho- that affects the skin and subcutaneous tissue. Regardless of the mycosis case in a 72-year-old seemingly immunocompetent patient aetiologic agent (bacteria or fungi), the clinical disease is essen- [10]. -

Fungal Infections (Mycoses): Dermatophytoses (Tinea, Ringworm)
Editorial | Journal of Gandaki Medical College-Nepal Fungal Infections (Mycoses): Dermatophytoses (Tinea, Ringworm) Reddy KR Professor & Head Microbiology Department Gandaki Medical College & Teaching Hospital, Pokhara, Nepal Medical Mycology, a study of fungal epidemiology, ecology, pathogenesis, diagnosis, prevention and treatment in human beings, is a newly recognized discipline of biomedical sciences, advancing rapidly. Earlier, the fungi were believed to be mere contaminants, commensals or nonpathogenic agents but now these are commonly recognized as medically relevant organisms causing potentially fatal diseases. The discipline of medical mycology attained recognition as an independent medical speciality in the world sciences in 1910 when French dermatologist Journal of Raymond Jacques Adrien Sabouraud (1864 - 1936) published his seminal treatise Les Teignes. This monumental work was a comprehensive account of most of then GANDAKI known dermatophytes, which is still being referred by the mycologists. Thus he MEDICAL referred as the “Father of Medical Mycology”. COLLEGE- has laid down the foundation of the field of Medical Mycology. He has been aptly There are significant developments in treatment modalities of fungal infections NEPAL antifungal agent available. Nystatin was discovered in 1951 and subsequently and we have achieved new prospects. However, till 1950s there was no specific (J-GMC-N) amphotericin B was introduced in 1957 and was sanctioned for treatment of human beings. In the 1970s, the field was dominated by the azole derivatives. J-GMC-N | Volume 10 | Issue 01 developed to treat fungal infections. By the end of the 20th century, the fungi have Now this is the most active field of interest, where potential drugs are being January-June 2017 been reported to be developing drug resistance, especially among yeasts. -
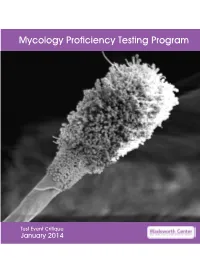
Mycology Proficiency Testing Program
Mycology Proficiency Testing Program Test Event Critique January 2014 Table of Contents Mycology Laboratory 2 Mycology Proficiency Testing Program 3 Test Specimens & Grading Policy 5 Test Analyte Master Lists 7 Performance Summary 11 Commercial Device Usage Statistics 13 Mold Descriptions 14 M-1 Stachybotrys chartarum 14 M-2 Aspergillus clavatus 18 M-3 Microsporum gypseum 22 M-4 Scopulariopsis species 26 M-5 Sporothrix schenckii species complex 30 Yeast Descriptions 34 Y-1 Cryptococcus uniguttulatus 34 Y-2 Saccharomyces cerevisiae 37 Y-3 Candida dubliniensis 40 Y-4 Candida lipolytica 43 Y-5 Cryptococcus laurentii 46 Direct Detection - Cryptococcal Antigen 49 Antifungal Susceptibility Testing - Yeast 52 Antifungal Susceptibility Testing - Mold (Educational) 54 1 Mycology Laboratory Mycology Laboratory at the Wadsworth Center, New York State Department of Health (NYSDOH) is a reference diagnostic laboratory for the fungal diseases. The laboratory services include testing for the dimorphic pathogenic fungi, unusual molds and yeasts pathogens, antifungal susceptibility testing including tests with research protocols, molecular tests including rapid identification and strain typing, outbreak and pseudo-outbreak investigations, laboratory contamination and accident investigations and related environmental surveys. The Fungal Culture Collection of the Mycology Laboratory is an important resource for high quality cultures used in the proficiency-testing program and for the in-house development and standardization of new diagnostic tests. Mycology Proficiency Testing Program provides technical expertise to NYSDOH Clinical Laboratory Evaluation Program (CLEP). The program is responsible for conducting the Clinical Laboratory Improvement Amendments (CLIA)-compliant Proficiency Testing (Mycology) for clinical laboratories in New York State. All analytes for these test events are prepared and standardized internally. -

Jamaica UHSM ¤ 1,2* University Hospital Harish Gugnani , David W Denning of South Manchester NHS Foundation Trust ¤Professor of Microbiology & Epidemiology, St
Burden of serious fungal infections in Jamaica UHSM ¤ 1,2* University Hospital Harish Gugnani , David W Denning of South Manchester NHS Foundation Trust ¤Professor of Microbiology & Epidemiology, St. James School of Medicine, Kralendjik, Bonaire (Dutch Caribbean). 1 LEADING WI The University of Manchester, Manchester Academic Health Science Centre, Manchester, U.K. INTERNATIONAL 2 FUNGAL The University Hospital of South Manchester, (*Corresponding Author) National Aspergillosis Centre (NAC) Manchester, U.K. EDUCATION Background and Rationale The incidence and prevalence of fungal infections in Jamaica is unknown. The first human case of Conidiobolus coronatus infection was discovered in Jamaica (Bras et al. 1965). Cases of histoplasmosis and eumycetoma are reported (Fincharn & DeCeulaer 1980, Nicholson et al., 2004; Fletcher et al, 2001). Tinea capitis is very frequent in children Chronic pulmonary (East-Innis et al., 2006), because of the population being aspergillosis with aspergilloma (in the left upper lobe) in a 53- predominantly of African ancestry. In a one year study of 665 HIV yr-old, HIV-negative Jamaican male, developing after one infected patients, 46% of whom had CD4 cell counts <200/uL, 23 had year of antitubercular treatment; his baseline IgG pneumocystis pneumonia and 3 had cryptococcal meningitis (Barrow titer was 741 mg/L (0-40). As a smoker, he also had moderate et al. 2010). We estimated the burden of fungal infections in Jamaica emphysema. from published literature and modelling. Table 1. Estimated burden of fungal disease in Jamaica Fungal None HIV Respiratory Cancer ICU Total Rate Methods condition /AIDS /Tx burden 100k We also extracted data from published papers on epidemiology and Oesophageal ? 2,100 - ? - 2,100 77 from the WHO STOP TB program and UNAIDS. -

Fungal Infections
FUNGAL INFECTIONS SUPERFICIAL MYCOSES DEEP MYCOSES MIXED MYCOSES • Subcutaneous mycoses : important infections • Mycologists and clinicians • Common tropical subcutaneous mycoses • Signs, symptoms, diagnostic methods, therapy • Identify the causative agent • Adequate treatment Clinical classification of Mycoses CUTANEOUS SUBCUTANEOUS OPPORTUNISTIC SYSTEMIC Superficial Chromoblastomycosis Aspergillosis Aspergillosis mycoses Sporotrichosis Candidosis Blastomycosis Tinea Mycetoma Cryptococcosis Candidosis Piedra (eumycotic) Geotrichosis Coccidioidomycosis Candidosis Phaeohyphomycosis Dermatophytosis Zygomycosis Histoplasmosis Fusariosis Cryptococcosis Trichosporonosis Geotrichosis Paracoccidioidomyc osis Zygomycosis Fusariosis Trichosporonosis Sporotrichosis • Deep / subcutaneous mycosis • Sporothrix schenckii • Saprophytic , I.P. : 8-30 days • Geographical distribution Clinical varieties (Sporotrichosis) Cutaneous • Lymphangitic or Pulmonary lymphocutaneous Renal Systemic • Fixed or endemic Bone • Mycetoma like Joint • Cellulitic Meninges Lymphangitic form (Sporotrichosis) • Commonest • Exposed sites • Dermal nodule pustule ulcer sporotrichotic chancre) (Sporotrichosis) (Sporotrichosis) • Draining lymphatic inflamed & swollen • Multiple nodules along lymphatics • New nodules - every few (Sporotrichosis) days • Thin purulent discharge • Chronic - regional lymph nodes swollen - break down • Primary lesion may heal spontaneously • General health - may not be affected (Sporotrichosis) (Sporotrichosis) Fixed/Endemic variety (Sporotrichosis) • -

Mycetoma: New Hope for Neglected Patients?
MYCETOMA: NEW HOPE FOR NEGLECTED PATIENTS? Developing effective treatments for a truly neglected disease DNDi MYCETOMA: NEW HOPE FOR NEGLECTED PATIENTS? Among the most neglected of neglected tropical diseases, the fungal form of mycetoma, eumycetoma, has no effective treatment. Currently, eumycetoma is managed with sub-optimal drugs and surgery, including amputation of affected limbs. An effective, affordable, and easy-to-administer treatment is urgently needed. Mycetoma is a slow-growing Photo: Abraham Ali/Imageworks/DNDi. bacterial or fungal infection, most often of the foot, that may spread to other parts of the body and can cause severe deformity. It is a debilitating disease that most often affects poor people in rural areas with limited access to health care. Due to the lack of effectiveness of available treatment, most lesions do not heal and instead recur on other parts of the body, leading to amputation and sometimes repeated amputations. In rare cases, when it affects the lungs or the brain, it can be fatal. In all instances patients are unable to work and often face severe social stigma. Mycetoma is so neglected that until 2016, it was not even listed in the World Health Organization’s list of neglected tropical diseases. Despite the impact of mycetoma, there has been little or no I got mycetoma 19 years ago after I was pricked funding or research attention to the disease until very recently. by a thorn. Even after numerous treatments, eight surgeries, and finally an amputation of my Mycetoma is so neglected that leg, I don’t think I am healed. I dropped out of until 2016, it was not even listed in the World Health Organization’s school after my first surgery and I had to stop list of neglected tropical diseases. -

Actinomycetoma: an Update on Diagnosis and Treatment
Actinomycetoma: An Update on Diagnosis and Treatment Roberto Arenas, MD; Ramón Felipe Fernandez Martinez, MD; Edoardo Torres-Guerrero, MD; Carlos Garcia, MD PRACTICE POINTS • Diagnosis of actinomycetoma is based on clinical manifestations including increased swelling and deformity of affected areas, presence of granulation tissue, scars, abscesses, sinus tracts, and a purulent exudate containing microorganisms. • The feet are the most commonly affected location, followed by the trunk (back and chest), arms, forearms, legs, knees, and thighs. • Specific diagnosis of actinomycetoma requires clinical examination ascopy well as direct examination of culture and biopsy results. • Overall, the cure rate for actinomycetoma ranges from 60% to 90%. not Mycetoma is a chronic infection that develops ycetoma is a subcutaneous disease that can after traumatic inoculation of the skin with eitherDo be caused by aerobic bacteria (actinomy- true fungi or aerobic actinomycetes. The resultant Mcetoma) or fungi (eumycetoma). Diagnosis infections are known as eumycetoma or actinomy- is based on clinical manifestations, including swell- cetoma, respectively. Although actinomycetoma is ing and deformity of affected areas, as well as rare in developed countries, migration of patients the presence of granulation tissue, scars, abscesses, from endemic areas makes knowledge of this con- sinus tracts, and a purulent exudate that contains dition crucial for dermatologists worldwide. We the microorganisms. present a review of the current concepts in the The worldwide proportion of mycetomas is epidemiology, clinical presentation,CUTIS diagnosis, 60% actinomycetomas and 40% eumycetomas.1 The and treatment of actinomycetoma. disease is endemic in tropical, subtropical, and tem- Cutis. 2017;99:E11-E15. perate regions, predominating between latitudes 30°N and 15°S. -
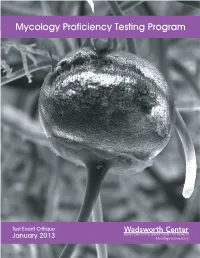
Mycology Proficiency Testing Program
Mycology Proficiency Testing Program Test Event Critique January 2013 Mycology Laboratory Table of Contents Mycology Laboratory 2 Mycology Proficiency Testing Program 3 Test Specimens & Grading Policy 5 Test Analyte Master Lists 7 Performance Summary 11 Commercial Device Usage Statistics 15 Mold Descriptions 16 M-1 Exserohilum species 16 M-2 Phialophora species 20 M-3 Chrysosporium species 25 M-4 Fusarium species 30 M-5 Rhizopus species 34 Yeast Descriptions 38 Y-1 Rhodotorula mucilaginosa 38 Y-2 Trichosporon asahii 41 Y-3 Candida glabrata 44 Y-4 Candida albicans 47 Y-5 Geotrichum candidum 50 Direct Detection - Cryptococcal Antigen 53 Antifungal Susceptibility Testing - Yeast 55 Antifungal Susceptibility Testing - Mold (Educational) 60 1 Mycology Laboratory Mycology Laboratory at the Wadsworth Center, New York State Department of Health (NYSDOH) is a reference diagnostic laboratory for the fungal diseases. The laboratory services include testing for the dimorphic pathogenic fungi, unusual molds and yeasts pathogens, antifungal susceptibility testing including tests with research protocols, molecular tests including rapid identification and strain typing, outbreak and pseudo-outbreak investigations, laboratory contamination and accident investigations and related environmental surveys. The Fungal Culture Collection of the Mycology Laboratory is an important resource for high quality cultures used in the proficiency-testing program and for the in-house development and standardization of new diagnostic tests. Mycology Proficiency Testing Program provides technical expertise to NYSDOH Clinical Laboratory Evaluation Program (CLEP). The program is responsible for conducting the Clinical Laboratory Improvement Amendments (CLIA)-compliant Proficiency Testing (Mycology) for clinical laboratories in New York State. All analytes for these test events are prepared and standardized internally.