The Severity of Naloxone-Precipitated Opiate Withdrawal Is Attenuated by Felbamate, a Possible Glycine Antagonist Therese A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Optum Essential Health Benefits Enhanced Formulary PDL January
PENICILLINS ketorolac tromethamineQL GENERIC mefenamic acid amoxicillin/clavulanate potassium nabumetone amoxicillin/clavulanate potassium ER naproxen January 2016 ampicillin naproxen sodium ampicillin sodium naproxen sodium CR ESSENTIAL HEALTH BENEFITS ampicillin-sulbactam naproxen sodium ER ENHANCED PREFERRED DRUG LIST nafcillin sodium naproxen DR The Optum Preferred Drug List is a guide identifying oxacillin sodium oxaprozin preferred brand-name medicines within select penicillin G potassium piroxicam therapeutic categories. The Preferred Drug List may piperacillin sodium/ tazobactam sulindac not include all drugs covered by your prescription sodium tolmetin sodium drug benefit. Generic medicines are available within many of the therapeutic categories listed, in addition piperacillin sodium/tazobactam Fenoprofen Calcium sodium to categories not listed, and should be considered Meclofenamate Sodium piperacillin/tazobactam as the first line of prescribing. Tolmetin Sodium Amoxicillin/Clavulanate Potassium LOW COST GENERIC PREFERRED For benefit coverage or restrictions please check indomethacin your benefit plan document(s). This listing is revised Augmentin meloxicam periodically as new drugs and new prescribing LOW COST GENERIC naproxen kit information becomes available. It is recommended amoxicillin that you bring this list of medications when you or a dicloxacillin sodium CARDIOVASCULAR covered family member sees a physician or other penicillin v potassium ACE-INHIBITORS healthcare provider. GENERIC QUINOLONES captopril ANTI-INFECTIVES -

Pharmacokinetic Drug–Drug Interactions Among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients
International Journal of Molecular Sciences Review Pharmacokinetic Drug–Drug Interactions among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients Marta Kara´zniewicz-Łada 1 , Anna K. Główka 2 , Aniceta A. Mikulska 1 and Franciszek K. Główka 1,* 1 Department of Physical Pharmacy and Pharmacokinetics, Poznan University of Medical Sciences, 60-781 Pozna´n,Poland; [email protected] (M.K.-Ł.); [email protected] (A.A.M.) 2 Department of Bromatology, Poznan University of Medical Sciences, 60-354 Pozna´n,Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-(0)61-854-64-37 Abstract: Anti-epileptic drugs (AEDs) are an important group of drugs of several generations, rang- ing from the oldest phenobarbital (1912) to the most recent cenobamate (2019). Cannabidiol (CBD) is increasingly used to treat epilepsy. The outbreak of the SARS-CoV-2 pandemic in 2019 created new challenges in the effective treatment of epilepsy in COVID-19 patients. The purpose of this review is to present data from the last few years on drug–drug interactions among of AEDs, as well as AEDs with other drugs, nutrients and food. Literature data was collected mainly in PubMed, as well as google base. The most important pharmacokinetic parameters of the chosen 29 AEDs, mechanism of action and clinical application, as well as their biotransformation, are presented. We pay a special attention to the new potential interactions of the applied first-generation AEDs (carba- Citation: Kara´zniewicz-Łada,M.; mazepine, oxcarbazepine, phenytoin, phenobarbital and primidone), on decreased concentration Główka, A.K.; Mikulska, A.A.; of some medications (atazanavir and remdesivir), or their compositions (darunavir/cobicistat and Główka, F.K. -

Chapter 25 Mechanisms of Action of Antiepileptic Drugs
Chapter 25 Mechanisms of action of antiepileptic drugs GRAEME J. SILLS Department of Molecular and Clinical Pharmacology, University of Liverpool _________________________________________________________________________ Introduction The serendipitous discovery of the anticonvulsant properties of phenobarbital in 1912 marked the foundation of the modern pharmacotherapy of epilepsy. The subsequent 70 years saw the introduction of phenytoin, ethosuximide, carbamazepine, sodium valproate and a range of benzodiazepines. Collectively, these compounds have come to be regarded as the ‘established’ antiepileptic drugs (AEDs). A concerted period of development of drugs for epilepsy throughout the 1980s and 1990s has resulted (to date) in 16 new agents being licensed as add-on treatment for difficult-to-control adult and/or paediatric epilepsy, with some becoming available as monotherapy for newly diagnosed patients. Together, these have become known as the ‘modern’ AEDs. Throughout this period of unprecedented drug development, there have also been considerable advances in our understanding of how antiepileptic agents exert their effects at the cellular level. AEDs are neither preventive nor curative and are employed solely as a means of controlling symptoms (i.e. suppression of seizures). Recurrent seizure activity is the manifestation of an intermittent and excessive hyperexcitability of the nervous system and, while the pharmacological minutiae of currently marketed AEDs remain to be completely unravelled, these agents essentially redress the balance between neuronal excitation and inhibition. Three major classes of mechanism are recognised: modulation of voltage-gated ion channels; enhancement of gamma-aminobutyric acid (GABA)-mediated inhibitory neurotransmission; and attenuation of glutamate-mediated excitatory neurotransmission. The principal pharmacological targets of currently available AEDs are highlighted in Table 1 and discussed further below. -

Pentazocine and Naloxone
PATIENT & CAREGIVER EDUCATION Pentazocine and Naloxone This information from Lexicomp® explains what you need to know about this medication, including what it’s used for, how to take it, its side effects, and when to call your healthcare provider. Warning This drug is a strong pain drug that can put you at risk for addiction, abuse, and misuse. Misuse or abuse of this drug can lead to overdose and death. Talk with your doctor. You will be watched closely to make sure you do not misuse, abuse, or become addicted to this drug. This drug may cause very bad and sometimes deadly breathing problems. Call your doctor right away if you have slow, shallow, or trouble breathing. The chance of very bad and sometimes deadly breathing problems may be greater when you first start this drug or anytime your dose is raised. Even one dose of this drug may be deadly if it is taken by someone else or by accident, especially in children. If this drug is taken by someone else or by accident, get medical help right away. Keep all drugs in a safe place. Keep all drugs out of the reach of children and pets. Using this drug for a long time during pregnancy may lead to withdrawal in the newborn baby. This can be life-threatening. Talk with the doctor. This drug has an opioid drug in it. Severe side effects have happened when opioid drugs were used with benzodiazepines, alcohol, marijuana or other forms of cannabis, or prescription or OTC drugs that may cause drowsiness or slowed actions. -

Phencyclidine: an Update
Phencyclidine: An Update U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES • Public Health Service • Alcohol, Drug Abuse and Mental Health Administration Phencyclidine: An Update Editor: Doris H. Clouet, Ph.D. Division of Preclinical Research National Institute on Drug Abuse and New York State Division of Substance Abuse Services NIDA Research Monograph 64 1986 DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Alcohol, Drug Abuse, and Mental Health Administratlon National Institute on Drug Abuse 5600 Fishers Lane Rockville, Maryland 20657 For sale by the Superintendent of Documents, U.S. Government Printing Office Washington, DC 20402 NIDA Research Monographs are prepared by the research divisions of the National lnstitute on Drug Abuse and published by its Office of Science The primary objective of the series is to provide critical reviews of research problem areas and techniques, the content of state-of-the-art conferences, and integrative research reviews. its dual publication emphasis is rapid and targeted dissemination to the scientific and professional community. Editorial Advisors MARTIN W. ADLER, Ph.D. SIDNEY COHEN, M.D. Temple University School of Medicine Los Angeles, California Philadelphia, Pennsylvania SYDNEY ARCHER, Ph.D. MARY L. JACOBSON Rensselaer Polytechnic lnstitute National Federation of Parents for Troy, New York Drug Free Youth RICHARD E. BELLEVILLE, Ph.D. Omaha, Nebraska NB Associates, Health Sciences Rockville, Maryland REESE T. JONES, M.D. KARST J. BESTEMAN Langley Porter Neuropsychiatric lnstitute Alcohol and Drug Problems Association San Francisco, California of North America Washington, D.C. DENISE KANDEL, Ph.D GILBERT J. BOTV N, Ph.D. College of Physicians and Surgeons of Cornell University Medical College Columbia University New York, New York New York, New York JOSEPH V. -

5 Clinical Pearls for Contraception and Preconception Counseling
EDITORIAL Women with epilepsy: 5 clinical pearls for contraception and preconception counseling For women with epilepsy, intrauterine devices are the optimal reversible contraceptive, and, preconception, the use of antiepileptic drugs with the lowest teratogenic potential should be considered Robert L. Barbieri, MD Editor in Chief, OBG MANAGEMENT Chair, Obstetrics and Gynecology Brigham and Women’s Hospital, Boston, Massachusetts Kate Macy Ladd Professor of Obstetrics, Gynecology and Reproductive Biology Harvard Medical School, Boston n 2015, 1.2% of the US population bazepine (Aptiom), felbamate (Fel- becoming pregnant while taking the was estimated to have active epi- batol), oxcarbazepine (Trileptal), oral contraceptive.6 Carbamazepine, Ilepsy.1 For neurologists, key goals perampanel (Fycompa), phenobarbi- a strong inducer of hepatic enzymes, in the treatment of epilepsy include: tal, phenytoin (Dilantin), primidone was the most frequently used AED in controlling seizures, minimizing (Mysoline), rufinamide (Banzel), this sample. adverse effects of antiepileptic drugs and topiramate (Topamax) (at dos- Many studies report that carba- (AEDs) and optimizing quality of ages >200 mg daily). According to mazepine accelerates the metabo- life. For obstetrician-gynecologists, Lexicomp, the following AEDs do not lisms of estrogen and progestins and women with epilepsy (WWE) have cause clinically significant changes reduces contraceptive efficacy. For unique contraceptive, preconcep- in hepatic enzymes that metabolize example, in one study 20 healthy tion, and obstetric needs that require steroid hormones: acetazolamide women were administered an ethi- highly specialized approaches to (Diamox), clonazepam (Klonopin), nyl estradiol (20 µg)-levonorgestrel care. Here, I highlight 5 care points ethosuximide (Zarontin), gabapentin (100 µg) contraceptive, and randomly that are important to keep in mind (Neurontin), lacosamide (Vimpat), assigned to either receive carbamaze- when counseling WWE. -

SAMHSA Opioid Overdose Prevention TOOLKIT
SAMHSA Opioid Overdose Prevention TOOLKIT Opioid Use Disorder Facts Five Essential Steps for First Responders Information for Prescribers Safety Advice for Patients & Family Members Recovering From Opioid Overdose TABLE OF CONTENTS SAMHSA Opioid Overdose Prevention Toolkit Opioid Use Disorder Facts.................................................................................................................. 1 Scope of the Problem....................................................................................................................... 1 Strategies to Prevent Overdose Deaths.......................................................................................... 2 Resources for Communities............................................................................................................. 4 Five Essential Steps for First Responders ........................................................................................ 5 Step 1: Evaluate for Signs of Opioid Overdose ................................................................................ 5 Step 2: Call 911 for Help .................................................................................................................. 5 Step 3: Administer Naloxone ............................................................................................................ 6 Step 4: Support the Person’s Breathing ........................................................................................... 7 Step 5: Monitor the Person’s Response .......................................................................................... -
NMMC West Point CDM.Xlsx
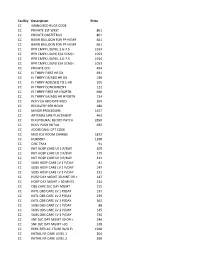
Facility Description Price CC SWING BED RUGS CODE CC PRIVATE 1ST WEST 861 CC PRIVATE OBSTETRICS 861 CC BAKRI BALLOON FOR PP HEMR 661 CC BAKRI BALLOON FOR PP HEMR 661 CC RPR CMPX LID/N/L 2.6‐7.5 1914 CC RPR CMPX LID/N/ E/A 5CM/< 1053 CC RPR CMPX LID/N/L 2.6‐7.5 1914 CC RPR CMPX LID/N/ E/A 5CM/< 1053 CC PRIVATE ECU 494 CC IV THRPY FIRST HR DX 691 CC IV THRPY EA/ADD HR DX 190 CC IV THRPY ADD/SEQ TO 1 HR 205 CC IV THRPY CONCURRENT 122 CC IV THRPY FIRST HR HYDRTN 690 CC IV THRPY EA/ADD HR HYDRTN 134 CC INJ IV EA ADD DIFF MED 269 CC RECOVERY PER HOUR 280 CC MINOR PROCEDURE 1627 CC ARTERIAL LINE PLACEMENT 463 CC INJ EPIDURAL BLOOD PATCH 2850 CC INJ IV PUSH INITIAL 692 CC ADDITIONAL CPT CODE CC MED ICU ROOM CHARGE 1872 CC NURSERY 1200 CC CIRC TRAY 91 CC INIT HOSP CARE LV 1 P/DAY 205 CC INIT HOSP CARE LV 2 P/DAY 279 CC INIT HOSP CARE LV 3 P/DAY 412 CC SUBS HOSP CARE LV 1 P/DAY 81 CC SUBS HOSP CARE LV 2 P/DAY 147 CC SUBS HOSP CARE LV 3 P/DAY 212 CC HOSP DAY MGMT 30 MNT OR < 147 CC HOSP DAY MGMT > 30 MNTS 214 CC OBS CARE D/C DAY MGMT 155 CC INITL OBS CARE LV 1 P/DAY 197 CC INITL OBS CARE LV 2 P/DAY 239 CC INITL OBS CARE LV 3 P/DAY 362 CC SUBS OBS CARE LV 1 P/DAY 88 CC SUBS OBS CARE LV 2 P/DAY 145 CC SUBS OBS CARE LV 3 P/DAY 236 CC SNF D/C DAY MGMT 30 OR < 240 CC SNF D/C DAY MGMT >30 318 CC PERC REPLAC J TUBE W/O FL 1948 CC INITIAL NF CARE LEVEL 1 204 CC INITIAL NF CARE LEVEL 2 290 CC INITIAL NF CARE LEVEL 3 368 CC SUBSQENT NF CARE LEVEL 197 CC SUBSQENT NF CARE LEVEL 2 151 CC SUBSQENT NF CARE LEVEL 3 198 CC SUBSQENT NF CARE LEVEL 4 295 CC OBS OR I/P -

Drug and Medication Classification Schedule
KENTUCKY HORSE RACING COMMISSION UNIFORM DRUG, MEDICATION, AND SUBSTANCE CLASSIFICATION SCHEDULE KHRC 8-020-1 (11/2018) Class A drugs, medications, and substances are those (1) that have the highest potential to influence performance in the equine athlete, regardless of their approval by the United States Food and Drug Administration, or (2) that lack approval by the United States Food and Drug Administration but have pharmacologic effects similar to certain Class B drugs, medications, or substances that are approved by the United States Food and Drug Administration. Acecarbromal Bolasterone Cimaterol Divalproex Fluanisone Acetophenazine Boldione Citalopram Dixyrazine Fludiazepam Adinazolam Brimondine Cllibucaine Donepezil Flunitrazepam Alcuronium Bromazepam Clobazam Dopamine Fluopromazine Alfentanil Bromfenac Clocapramine Doxacurium Fluoresone Almotriptan Bromisovalum Clomethiazole Doxapram Fluoxetine Alphaprodine Bromocriptine Clomipramine Doxazosin Flupenthixol Alpidem Bromperidol Clonazepam Doxefazepam Flupirtine Alprazolam Brotizolam Clorazepate Doxepin Flurazepam Alprenolol Bufexamac Clormecaine Droperidol Fluspirilene Althesin Bupivacaine Clostebol Duloxetine Flutoprazepam Aminorex Buprenorphine Clothiapine Eletriptan Fluvoxamine Amisulpride Buspirone Clotiazepam Enalapril Formebolone Amitriptyline Bupropion Cloxazolam Enciprazine Fosinopril Amobarbital Butabartital Clozapine Endorphins Furzabol Amoxapine Butacaine Cobratoxin Enkephalins Galantamine Amperozide Butalbital Cocaine Ephedrine Gallamine Amphetamine Butanilicaine Codeine -
Evaluation of Biased and Balanced Salvinorin a Analogs in Preclinical Models of Pain
fnins-14-00765 July 18, 2020 Time: 20:26 # 1 ORIGINAL RESEARCH published: 21 July 2020 doi: 10.3389/fnins.2020.00765 Evaluation of Biased and Balanced Salvinorin A Analogs in Preclinical Models of Pain Kelly F. Paton1, Andrew Biggerstaff1, Sophia Kaska2, Rachel S. Crowley3, Anne C. La Flamme1,4, Thomas E. Prisinzano2,3 and Bronwyn M. Kivell1* 1 School of Biological Sciences, Centre for Biodiscovery, Faculty of Science, Victoria University of Wellington, Wellington, New Zealand, 2 Department of Pharmaceutical Sciences, College of Pharmacy, University of Kentucky, Lexington, KY, United States, 3 Department of Medicinal Chemistry, School of Pharmacy, The University of Kansas, Lawrence, KS, United States, 4 Malaghan Institute of Medical Research, Wellington, New Zealand In the search for safer, non-addictive analgesics, kappa opioid receptor (KOPr) agonists are a potential target, as unlike mu-opioid analgesics, they do not have abuse potential. Salvinorin A (SalA) is a potent and selective KOPr agonist, however, clinical utility is limited by the short duration of action and aversive side effects. Biasing KOPr signaling toward G-protein activation has been highlighted as a key cellular mechanism to reduce the side effects of KOPr agonists. The present study investigated KOPr signaling bias and the acute antinociceptive effects and side effects of two novel analogs of SalA, Edited by: 16-Bromo SalA and 16-Ethynyl SalA. 16-Bromo SalA showed G-protein signaling bias, Dominique Massotte, whereas 16-Ethynyl SalA displayed balanced signaling properties. In the dose-response Université de Strasbourg, France tail-withdrawal assay, SalA, 16-Ethynyl SalA and 16-Bromo SalA were more potent than Reviewed by: Mariana Spetea, the traditional KOPr agonist U50,488, and 16-Ethynyl SalA was more efficacious. -

TALWIN Nx Is an Analgesic for Oral Administration
NDA 018733/S-015 Page 4 TALWIN® Nx CIV pentazocine hydrochloride and naloxone hydrochloride, USP Analgesic for Oral Use Only WARNING: TALWIN® Nx is intended for oral use only. Severe, potentially lethal, reactions may result from misuse of TALWIN® Nx by injection either alone or in combination with other substances. (See DRUG ABUSE AND DEPENDENCE section.) DESCRIPTION TALWIN Nx (pentazocine and naloxone hydrochlorides, USP) contains pentazocine hydrochloride, USP, equivalent to 50 mg base and is a member of the benzazocine series (also known as the benzomorphan series), and naloxone hydrochloride, USP, equivalent to 0.5 mg base. TALWIN Nx is an analgesic for oral administration. Chemically, pentazocine hydrochloride is (2R*,6R*,11R*)-1,2,3,4,5,6-Hexahydro-6,11 dimethyl-3-(3-methyl-2-butenyl)-2,6-methano-3-benzazocin-8-ol hydrochloride, a white, crystalline substance soluble in acidic aqueous solutions, and has the following structural formula: C19H27NO·HCl M.W. 321.88 Chemically, naloxone hydrochloride is Morphinan-6-one,4,5-epoxy-3,14-dihydroxy-17-(2 propenyl)-, hydrochloride, (5α)-. It is a slightly off-white powder, and is soluble in water and dilute acids, and has the following structural formula: Reference ID: 2909136 NDA 018733/S-015 Page 5 C19H21NO4·HCl M.W.=363.84 Inactive Ingredients: Colloidal Silicon Dioxide, Dibasic Calcium Phosphate, D&C Yellow #10, FD&C Yellow #6, Magnesium Stearate, Microcrystalline Cellulose, Sodium Lauryl Sulfate, Starch. CLINICAL PHARMACOLOGY Pentazocine is a Schedule IV opioid analgesic which when administered orally in a 50 mg dose appears equivalent in analgesic effect to 60 mg of codeine. -

Status Epilepticus
Status Epilepticus By Aaron M. Cook, Pharm.D., BCPS, BCCCP Reviewed by Gretchen M. Brophy, Pharm.D., FCCP, BCPS; Matthew J. Korobey, Pharm.D. BCCCP; and You Min Sohn, Pharm.D., M.S., BCPS, BCCCP LEARNING OBJECTIVES 1. Evaluate factors that may affect treatment success in patients with status epilepticus. 2. Distinguish gaps in the literature related to optimal status epilepticus treatment. 3. Evaluate therapeutic strategies for super-refractory status epilepticus. 4. Assess the impact of timing of status epilepticus treatment initiation, and develop strategies to optimize effective treatment. DEFINITIONS OF STATUS EPILEPTICUS ABBREVIATIONS IN THIS CHAPTER Status epilepticus is defined as continuous seizure activity for EEG Electroencephalogram greater than 5 minutes or consecutive seizures without regaining GABA g-Aminobutyric acid consciousness over 5 minutes. Status epilepticus is common in ICH Intracerebral hemorrhage the epilepsy population and is often associated with acute, severe NMDA N-methyl-D-aspartate neurological injury or illness such as traumatic brain injury (TBI), TBI Traumatic brain injury intracerebral hemorrhage (ICH), meningitis, or pharmacologic toxic- Table of other common abbreviations. ity/withdrawal. Overall, the incidence of status epilepticus is about 12 per 100,000 individuals, a value that has increased 50% since the early 2000s (Dham 2014). Status epilepticus is often divided into “convulsive” status epilepticus (in which the patient has obvi- ous clinical manifestations of seizures, mental status impairment, or postictal focal neurological deficits) and “nonconvulsive” status epi- lepticus (in which the patient has no obvious clinical manifestations of seizure, but seizure activity is revealed on electroencephalogram [EEG]). Refractory status epilepticus is defined as status epilepticus that persists despite treatment with at least two antiepileptic drugs.