Airway Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Paramedic Airway Management Course
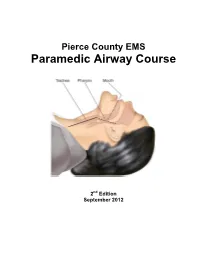
Pierce County EMS Paramedic Airway Course 2nd Edition September 2012 Pierce County EMS Paramedic Airway Management Course Table of Contents: Acknowledgements ............................................................................................ 3 Course Purpose and Description ..................................................................... 4 Background ........................................................................................................ 5 Assessing the Need for Emergency Airway Management ............................. 6 Effective Use of the Bag-Valve Mask ............................................................... 7 Endotracheal Intubation—Preparing for First Pass Success ........................ 8 RSI & Endotracheal Intubation ....................................................................... 11 Confirming, Securing and Monitoring Airway Placement ............................ 15 Use of Alternative “Rescue Airways” ............................................................ 16 Surgical Airways .............................................................................................. 17 Emergency Airway Management in Special Populations: ........................... 18 Pediatric Patients Geriatric Patients Trauma Patients Bariatric Patients Pregnant Patients Ten Tips for Best Practices in Emergency Airway Management ................ 21 Airway Performance Documentation and CQI Analysis ............................... 22 Conclusion ...................................................................................................... -

Mapping the Use of Simulation in Prehospital Care – a Literature Review Anna Abelsson1*, Ingrid Rystedt1, Björn-Ove Suserud2 and Lillemor Lindwall1
Abelsson et al. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2014, 22:22 http://www.sjtrem.com/content/22/1/22 REVIEW Open Access Mapping the use of simulation in prehospital care – a literature review Anna Abelsson1*, Ingrid Rystedt1, Björn-Ove Suserud2 and Lillemor Lindwall1 Abstract Background: High energy trauma is rare and, as a result, training of prehospital care providers often takes place during the real situation, with the patient as the object for the learning process. Such training could instead be carried out in the context of simulation, out of danger for both patients and personnel. The aim of this study was to provide an overview of the development and foci of research on simulation in prehospital care practice. Methods: An integrative literature review were used. Articles based on quantitative as well as qualitative research methods were included, resulting in a comprehensive overview of existing published research. For published articles to be included in the review, the focus of the article had to be prehospital care providers, in prehospital settings. Furthermore, included articles must target interventions that were carried out in a simulation context. Results: The volume of published research is distributed between 1984- 2012 and across the regions North America, Europe, Oceania, Asia and Middle East. The simulation methods used were manikins, films, images or paper, live actors, animals and virtual reality. The staff categories focused upon were paramedics, emergency medical technicians (EMTs), medical doctors (MDs), nurse and fire fighters. The main topics of published research on simulation with prehospital care providers included: Intubation, Trauma care, Cardiac Pulmonary Resuscitation (CPR), Ventilation and Triage. -

Resuscitation and Defibrillation
AARC GUIDELINE: RESUSCITATION AND DEFIBRILLATION AARC Clinical Practice Guideline Resuscitation and Defibrillation in the Health Care Setting— 2004 Revision & Update RAD 1.0 PROCEDURE: signs, level of consciousness, and blood gas val- Recognition of signs suggesting the possibility ues—included in those conditions are or the presence of cardiopulmonary arrest, initia- 4.1 Airway obstruction—partial or complete tion of resuscitation, and therapeutic use of de- 4.2 Acute myocardial infarction with cardio- fibrillation in adults. dynamic instability 4.3 Life-threatening dysrhythmias RAD 2.0 DESCRIPTION/DEFINITION: 4.4 Hypovolemic shock Resuscitation in the health care setting for the 4.5 Severe infections purpose of this guideline encompasses all care 4.6 Spinal cord or head injury necessary to deal with sudden and often life- 4.7 Drug overdose threatening events affecting the cardiopul- 4.8 Pulmonary edema monary system, and involves the identification, 4.9 Anaphylaxis assessment, and treatment of patients in danger 4.10 Pulmonary embolus of or in frank arrest, including the high-risk de- 4.11 Smoke inhalation livery patient. This includes (1) alerting the re- 4.12 Defibrillation is indicated when cardiac suscitation team and the managing physician; (2) arrest results in or is due to ventricular fibril- using adjunctive equipment and special tech- lation.1-5 niques for establishing, maintaining, and moni- 4.13 Pulseless ventricular tachycardia toring effective ventilation and circulation; (3) monitoring the electrocardiograph and recogniz- -
EMS Patient Care Procedure Documents for NC EMS Systems
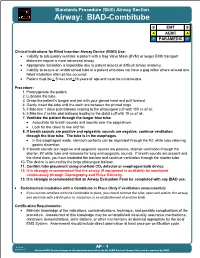
Standards Procedure (Skill) Airway Section Airway: BIAD-Combitube B EMT B A AEMT A P PARAMEDIC P Clinical Indications for Blind Insertion Airway Device (BIAD) Use: Inability to adequately ventilate a patient with a Bag Valve Mask (BVM) or longer EMS transport distances require a more advanced airway. Appropriate intubation is impossible due to patient access or difficult airway anatomy. Inability to secure an endotracheal tube in a patient who does not have a gag reflex where at least one failed intubation attempt has occurred. Patient must be > 5 feet and >16 years of age and must be unconscious. Procedure: 1. Preoxygenate the patient. 2. Lubricate the tube. 3. Grasp the patient s tongue and jaw with your gloved hand and pull forward. 4. Gently insert the tube until the teeth are between the printed rings. 5. Inflate line 1 (blue pilot balloon) leading to the pharyngeal cuff with 100 cc of air. 6. Inflate line 2 (white pilot balloon) leading to the distal cuff with 15 cc of air. 7. Ventilate the patient through the longer blue tube. Auscultate for breath sounds and sounds over the epigastrium. Look for the chest to rise and fall. 8. If breath sounds are positive and epigastric sounds are negative, continue ventilation through the blue tube. The tube is in the esophagus. In the esophageal mode, stomach contents can be aspirated through the #2, white tube relieving gastric distention. 9. If breath sounds are negative and epigastric sounds are positive, attempt ventilation through the shorter, #2 white tube and reassess for lung and epigastric sounds. -

OPITO Medical Emergency Response and Planning Requirements (Implementation Date 8Th November 2019)
OPITO Medical Emergency Response and Planning Requirements (Implementation date 8th November 2019) OPITO Medical Emergency Response and Planning Requirements © OPITO The content of this document was developed and reviewed in 2015 by OPITO to improve Emergency Response Arrangements based on accepted industry best practices. It was updated in 2019 to reflect a more risk-based approach towards requirements for each type of Training Centre. Guidance on this document is available by contacting OPITO. © OPITO All rights reserved. No part of this publication may be reproduced, stored in a retrieval or information storage system, or transmitted, in any form or by any means, mechanical, photocopying, recording or otherwise, without the prior permission in writing of the publishers. AMENDMENTS AMENDMENT & DATE PAGES CHANGES CHECKED BY APPROVED MADE BY BY Revision 0 released January Global Technical Industry and Global 2016 Coordinator OPITO Approvals Technical Department Director Rev 1 released August 2019 Approvals Approvals Director, All QA Department Standards Director Any amendments made to this document by OPITO will be recorded above. Revision 1 (August 2019) Page 2 of 29 OPITO Medical Emergency Response and Planning Requirements © OPITO CONTENTS INTRODUCTION ........................................................................................................................ 4 SECTION 1 - RISK BASED PLANNING ..................................................................................... 7 1.1 MEDICAL EMERGENCY RESPONSE AND PLANNING -

Emerging Uses of Capnography in Emergency Medicine in Emergency Capnography Uses of Emerging
Emerging Uses of Capnography in Emergency Medicine WHITEPAPER INTRODUCTION The Physiologic Basis for Capnography Capnography is based on a discovery by chemist Joseph Black, who, in 1875, noted the properties of a gas released during exhalation that he called “fixed air.” That gas—carbon dioxide (CO2)—is produced as a consequence of cellular metabolism as the waste product of combining oxygen and glucose to produce energy. Carbon dioxide exits the body via the lungs. The concentration of CO2 in an exhaled breath reflects cardiac output and pulmonary blood flow as the gas is transported by the venous system to the right side of the heart and then pumped into the lungs by the right ventricle. Capnographs measure the concentration of CO2 at the end of each exhaled breath, commonly known as the end- tidal carbon dioxide (EtCO2). As long as the heart is beating and blood is flowing, CO2 is delivered continuously to the lungs for exhalation. An EtCO2 value outside the normal range in a patient with normal pulmonary blood flow indicates a problem with ventilation that may require immediate attention. Any deviation from normal ventilation quickly changes EtCO2, even when SpO2—the indirect measurement of oxygen saturation in the blood—remains normal. Thus, EtCO2 is a more sensitive and rapid indicator of ventilation problems than SpO2.1 Why EtCO2 Monitoring Is Important It is generally accepted that EtCO2 monitoring is the practice standard for determining whether endotracheal tubes are correctly placed. However, there are other important indications for its use as well. Ventilatory monitoring by EtCO2 measurement has long been a standard in the surgical and intensive care patient populations. -

Basic Airway Management & Decision Making
Roberts: Clinical Procedures in Emergency Medicine, 5th ed. CHAPTER 3 – Basic Airway Management and Decision-Making Robert F. Reardon, Phillip E. Mason, Joseph E. Clinton Over the last few decades, several important changes have occurred in emergency airway management. Bag-mask ventilation has been supplemented by intermediate, or backup, ventilation devices like the laryngeal mask airway (LMA), the Combitube, and the laryngeal tube. These have become important devices for the initial resuscitation of apneic patients and for rescue ventilation when intubation fails.[1] Noninvasive positive-pressure ventilation (NPPV) is now used in place of tracheal intubation in some critically ill patients. Despite these advances, basic techniques such as opening the airway, oxygenation, and bag-mask ventilation remain the cornerstones of good emergency airway management. [2] [3] Airway maintenance without endotracheal intubation is one of the most important emergency [4] airway management techniques to keep patients alive until a definitive airway can be established. This chapter describes basic airway skills including opening the airway, O2 therapy, NPPV, bag-mask ventilation, and intermediate ventilation devices. Because of the complexity of these skills and decisions, providers should develop a simple, organized approach to emergency airway management, being cognizant that when a specific intervention has failed, it is time to move rapidly to a different approach. Developing a simple preconceived algorithm that employs proven techniques and is applicable to a broad range of clinical scenarios will help providers manage difficult, anxiety-provoking emergency airways. THE CHALLENGE OF EMERGENCY AIRWAY MANAGEMENT Although other specialists are sometimes available, most emergency airways are managed by emergency clinicians.[5] Airway management in the emergency department (ED) is much different from airway management in the controlled setting of the operating room. -

EPFR EMS Bid List 2010
EPFR EMS Bid List 2010 Item Category and Description Size and Unit of Packaging Unit of Issue Estimated Unit Price Extended Price Boundtree Item # Bandaging Consumption Including Shipping 151527 Tape, 1" Transpore Clear 12/BX BX 20 372-7111EA Tape, 1" Silk EA 36 47-1914BX Tape, 1" Paper 12/BX BX 4 372-7112BX Tape, 2" Silk 6/BX BX 6 625-2045033BX Tape, 2" Waterproof 6/BX BX 4 105BLF Hy-Tape 1/2" X 5 yd 36/CS CS 1 1211-209 Hemcon 2" X 4" EA 16 F165200 Bandaid, Fabric 1 X 3" 100/BX BX 20 533-MS-TRI40EA Triangular Bandage 40x40x54 EA 132 276-602PB96EA Kling Gauze Roll 2" EA 180 276-603PB96EA Kling Gauze Roll 3" EA 180 276-604PB96EA Kling Gauze Roll 4" X 4.1 yd EA 180 276-606PB48EA Kling Gauze Roll 6" X 85" EA 36 150031 Kerlex Gauze Roll 4" X 4.1 yd EA 100 J2540 Gauze Pad, Sterile 8 Ply 2" X 2" 50/TR TR 80 085360 Gauze Pad, Sterile 2/PK 4" X 4" 25/BX BX 100 085590 Gauze Pad, ABD 5" X 9" 25/TR TR 10 085810 Gauze Pad, ABD 8" X 10" 20/TR TR 10 150062 Trauma Dressing 10" X 30" EA 50 150066K1 Vaseline Gauze 3" x 9" EA 20 56-0967 Obstetrics Kit EA 4 533-MS-BS0033EA Burn Sheets 60 X 96" Sterile EA 24 Philips Products 2742-ATM3713A Adult Defibrillation Pads Philips MRX EA 70 M3717A Pedi Defibrillation Pads Philips MRX EA 20 M2202A EKG Electrodes Philips MRX 5/PK PK 3200 13955C Ped/Neo Electrodes Philips MRX 30/PK PK 1 174620 ETCO2 Adapter ET Adult/Ped Philips MRX EA 100 Page 1 of 11 EPFR EMS Bid List 2010 M1923A ETCO2 Adapter ET Ped/Infant Philips MRX EA 10 177653 ETCO2 Adapter NC Adult Philips MRX EA 200 M2520A ETCO2 Adapter NC Pediatric Philips -
Washington State First Responder (EMR) Field Protocols
WASHINGTON STATE DEPARTMENT OF HEALTH HEALTH SYSTEMS QUALITY ASSURANCE DIVISION OFFICE OF EMERGENCY MEDICAL AND TRAUMA PREVENTION FIRST RESPONDER FIELD PROTOCOLS DOH Pub. 530-001, (Revised September 2005) These protocols have been reviewed and endorsed by the Medical Program Directors and the Department of Health, Licensing and Certification Advisory Committee. For questions or comments, contact: Licensing and Certification Section Office of Emergency Medical and Trauma Prevention P.O. Box 47853 Olympia, Washington 98504-7853 360-236-2840 These First Responder Field Protocols are State Protocols that establish the standard for field performance. EMS County Medical Program Directors may NOT have protocols that vary from these without specific written approval from the Department of Health. Any deviation from these protocols must be identified to and approved in writing by the Department of Health. THESE FIELD PROTOCOLS WERE DEVELOPED AND WRITTEN WITH THE ASSISTANCE OF THE FOLLOWING INDIVIDUALS: WASHINGTON STATE EM/TP PROTOCOL WORK GROUP Nina Conn Patty Courson Kenny Karnes Dane Kessler Richard Kness Marc Muhr Jim Palmer Terry Patton Jack Pinza Lynn Wittwer, MD 2 Introduction These protocols were developed by the Washington State Protocol Work Group and represent the consolidation of recommendations for emergency pre-hospital patient care from many local and national sources. The assessment information in the First Responder General Orders is intended to be considered with all protocols. These protocols are intended to: 1. Provide a guide to the appropriate emergency medical care procedures to be employed by EMS personnel while working under the direction of the County Medical Program Director; 2. Assist in the standardization of pre-hospital care in Washington State; 3. -

Bag-Valve Mask Ventilation” Page 1
FDNY–EMS CME JOURNAL 2009_J01 “Back to the Basics”: BAG -VALVE MASK VENTILATION lthough all airway skills are important, the most important skill, and perhaps the most difficult, is the ability to use a bag and mask to effectively oxygenate and ventilate a patient. While over A the years there have been important advances in emergency airway management, such as alternative airways (e.g. Combitube), Bag-Valve Mask (BVM) ventilation is a life-saving skill that is often underappreciated. While BVM ventilation may seem mundane compared to placing an advanced airway (e.g. endotracheal tube, Combitube), it is actually a skill that is difficult to master. The false belief that BVM ventilation is an easy skill has led many health-care providers to mistakenly think they are proficient in this skill. The purpose of this article is to review BVM ventilation and associated skills and techniques to effectively ventilate a patient. In the second half of this article is a review of some of the advanced airway tools and techniques. While most applicable for Advanced Life Support (ALS) providers, it is beneficial for all personnel to have an awareness of them. Proper positioning of the patient is a critical element for successful BVM ventilation. The classic teaching for both ventilation and intubation positioning is placing the patient in the “sniffing position” provided there are no spinal precautions that need to be taken. The purpose is to allow for proper alignment of the oropharyngeal axes (Figure 1). Figure 1 FDNY–EMS CME Journal 2009_J01 “Bag-Valve Mask Ventilation” Page 1. However, this still may be inadequate, especially for pediatric and obese patients. -

This Procedure Includes the Following: • Endotracheal Intubation (Plus Use of Supraglottic Airway Laryngopharyngeal Tube (S.A
ADVANCED AIRWAY PROCEDURES This procedure includes the following: Endotracheal intubation (plus use of Supraglottic Airway Laryngopharyngeal Tube (S.A.L.T. device), gum elastic bougie assisted tracheal intubation, video laryngoscopy) Non-Visualized Airways (Dual lumen airway, King LT-D™ Airway, Laryngeal Mask Airway (LMA)) Cricothyroidotomy – needle and surgical GENERAL CONSIDERATIONS Rescuers must be aware of the risks and benefits of advanced airway management techniques. In cases of cardiac arrest the insertion of an advanced airway may require interruption of chest compressions for many seconds, the rescuer should weigh the need for compressions against the need for insertion of an advanced airway. Rescuers may defer insertion of an advanced airway until the patient fails to respond to initial CPR and defibrillation attempts or demonstrates return of spontaneous circulation. Providers should have a second (back-up) strategy for airway management and ventilation if they are unable to establish the first-choice airway adjunct. Bag-mask ventilation may provide that back-up strategy. ENDOTRACHEAL INTUBATION A. Indications for emergency endotracheal intubation are: 1. Inability of the rescuer to adequately ventilate the patient with a bag-mask device 2. The absence of airway protective reflexes (coma and cardiac arrest) B. In most case, endotracheal intubation provides definite control of the airway. Its purposes include: 1. Actively ventilating the patient 2. Delivering high concentrations of oxygen 3. Suctioning secretions and maintaining airway patency 4. Preventing aspiration of gastric contents, upper airway secretions or blood 5. Prevented gastric distention due to assisted ventilations 6. Administering positive pressure when extra fluid is present in alveoli 7. Administering medications during resuscitation for absorption through lungs as a last resort C. -

Complications Associated with the Esophageal- Tracheal Combitube
124 REPORTSCANADIAN OF JOURNALORIGINAL OFINVESTIGATIONS ANESTHESIA Complications associated with the Esophageal- Tracheal Combitube® in the pre-hospital setting [Complications associées avec l’utilisation du Combitube dans la prise en charge des arrêts cardio-respiratoires en préhospitalier] Marie-Claude Vézina MD, Claude A. Trépanier MD FRCPC, Pierre C. Nicole MD FRCPC, Martin R. Lessard MD FRCPC Purpose: The Esophageal-Tracheal Combitube® (Combitube) CAN J ANESTH 2007 / 54: 2 / pp 124–128 is widely used for the management of the airway during cardi- opulmonary resuscitation in the pre-hospital setting. Although serious complications have been reported with the Combitube, there is a paucity of data relative to the frequency and nature Objectif : Le Esophageal-Tracheal Combitube® (Combitube) est of such complications. The objective of this retrospective study couramment utilisé pour assurer le contrôle des voies aériennes lors was to determine the incidence and the nature of complications de situations d’arrêt cardio-respiratoire en préhospitalier. Bien que associated to the Combitube in the pre-hospital setting. des complications graves reliées à l’utilisation du Combitube aient Methods: Since 1993, in the Quebec City Health Region, the été rapportées, leur incidence réelle est mal connue. L’objectif de basic life support treatment algorithm for emergency medical cette étude rétrospective était d’estimer l’incidence et la nature technicians has included the use of a Combitube as the primary des complications associées à l’utilisation du Combitube en pré- airway device for management of all patients presenting with hospitalier. cardiac or respiratory arrest. The database of the emergency Méthode : Depuis 1993, le protocole de prise en charge préhospi- coordination services was searched for the period between talière de l’Agence régionale de santé de Québec inclut l’insertion 1993 and 2003 (2,981 patients).