Knowledge, Attitudes and Practices of Young People in Zimbabwe On
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cholera in Zimbabwe: Epidemiological Bulletin Number 12 Week 9 (22-28 February 2009)
Cholera in Zimbabwe: Epidemiological Bulletin Number 12 Week 9 (22-28 February 2009) Foreword This is the 12th epidemiological bulletin to be issued since the onset of a countrywide Zimbabwe cholera epidemic first reported in August, 2008. Bulletins are to be published weekly to coincide with the end of an epidemiological week (Sunday to Saturday). Daily cumulative caseload updates are posted on the OCHA website http://ochaonline.un.org/Default.aspx?alias=ochaonline.un.org/zimbabwe The bulletin provides a weekly overview of the epidemic in Zimbabwe, including province by province data, to inform and improve the continuing public health response. It also provides guidance to agencies on issues relating to data collection, analysis and interpretation, and suggests operational strategies on the basis of epidemiological patterns so far. The WHO Team welcomes feedback and data provided by individual agencies. Given the scope of this epidemic, errors and omissions are inevitable: we will be grateful for any information that helps to rectify these. Please send any comments and feedback to the Cholera Control and Command Centre Email: [email protected]. Toll free number for alert by district and province is 08089001 or 08089002 or 08089000 Mobile number for alerts is 0912 104 257 Source: Ministry of Health and Child Welfare Rapid Disease Notification System 1 Foreword 1 1. Outbreak summary 3 2. National Overview 4 2.1. Cases and deaths 4 2.2. Mortality 5 2.3. Cholera treatment centres (CTC and CTU) 6 2.4. Surveillance findings by province 7 3. Laboratory testing 14 4. Activities carried out by the C4 15 5. -

Zimbabwe-HIV-Estimates Report 2018
ZIMBABWE NATIONAL AND SUB-NATIONAL HIV ESTIMATES REPORT 2017 AIDS & TB PROGRAMME MINISTRY OF HEALTH AND CHILD CARE July 2018 Foreword The Ministry of Health and Child Care (MOHCC) in collaboration with National AIDS Council (NAC) and support from partners, produced the Zimbabwe 2017 National, Provincial and District HIV and AIDS Estimates. The UNAIDS, Avenir Health and NAC continued to provide technical assistance and training in order to build national capacity to produce sub-national estimates in order to track the epidemic. The 2017 Estimates report gives estimates for the impact of the programme. It provide an update of the HIV and AIDS estimates and projections, which include HIV prevalence and incidence, programme coverages, AIDS-related deaths and orphans, pregnant women in need of PMTCT services in the country based on the Spectrum Model version 5.63. The 2017 Estimates report will assist the country to monitor progress towards the fast track targets by outlining programme coverage and possible gaps. This report will assist programme managers in accounting for efforts in the national response and policy makers in planning and resource mobilization. Brigadier General (Dr.) G. Gwinji Permanent Secretary for Health and Child Care Page | i Acknowledgements The Ministry of Health and Child Care (MOHCC) would want to acknowledge effort from all individuals and organizations that contributed to the production of these estimates and projections. We are particularly grateful to the National AIDS Council (NAC) for funding the national and sub-national capacity building and report writing workshop. We are also grateful to the National HIV and AIDS Estimates Working Group for working tirelessly to produce this report. -

Second Joint Donor Review of International Organization For
Second Joint Donor Review of International Organization for Migration (IOM) Programmes on Emergency Assistance to Mobile and Vulnerable Populations in Zimbabwe, Humanitarian Assistance to Returned Migrants and Mobile Populations at the South Africa-Zimbabwe Border, and the Safe Journey Information Campaign 28 May – 5 June 2007 For DFID, Sida, USAID and ECHO Brighton M. Mvumi (Faculty of Agriculture, University of Zimbabwe) Marion Pratt (USAID/Washington and the University of Arizona) Helen Robson (DfID/London) June 2007 IOM JOINT DONOR REVIEW 2007 ACKNOWLEDGEMENTS We gratefully acknowledge the assistance provided by IOM for the scheduling, transportation, work space, staff time, and document compilation. The open attitude of the staff members towards the review process and institutional strengths and weaknesses – a rare characteristic - is also highly commended. The team also thanks the beneficiaries, implementing partners, United Nations agencies, donor representatives, and local and national authorities for sharing their experiences with us, and finally DFID for coordinating the review. Cover picture (by Brighton Mvumi): The borehole that supplies irrigation water for Zunidza resettled community, Makoni district, Manicaland province. 2 IOM JOINT DONOR REVIEW 2007 TABLE OF CONTENTS ACKNOWLEDGEMENTS ....................................................................................2 EXECUTIVE SUMMARY ......................................................................................5 General Findings .............................................................................................5 -

Cholera in Zimbabwe: Epidemiological Bulletin Number 27 Week 24 (7 to 13 June 2009)
Cholera in Zimbabwe: Epidemiological Bulletin Number 27 Week 24 (7 to 13 June 2009) Foreword This is the 27th epidemiological bulletin to be issued since the onset of a countrywide Zimbabwe cholera epidemic first reported in August 2008. Bulletins are published weekly to coincide with the end of an epidemiological week (Sunday to Saturday). Daily cumulative caseload updates are posted on the WHO website, http://www.who.int/hac/crises/zwe/en/index.html and http://www.who.int/hac/crises/zmb/sitreps/cholera_daily_updates/en/index.html as well as on the OCHA website http://ochaonline.un.org/zimbabwe The bulletin provides a weekly overview of the epidemic in Zimbabwe, including province by province data, to inform and improve the continuing public health response. It also provides guidance to agencies on issues relating to data collection, analysis and interpretation, and suggests operational strategies on the basis of epidemiological patterns so far. The WHO Team welcomes feedback and data provided by individual agencies. Given the scope of this epidemic, errors and omissions are inevitable: we will be grateful for any information that helps to rectify these. Please send any comments and feedback to the Cholera Control and Command Centre Email: [email protected]. Toll free number for alert by district and province is 08089001 or 08089002 or 08089000 Mobile number for alerts is 0912 104 257 Acknowledgements We are very grateful to MoHCW District Medical Officers, Provincial Surveillance Officers, Provincial Medical Directors, Environmental Heath Officers, and MoHCW's department of surveillance, who have helped to gather and share the bulk of the information presented here. -

ITB/ZWE30/2021/02442 for the Supply and Installation of Solar
Invitation to Bid (ITB) Quotation For the supply and installation of solar equipment in Zimbabwe Reference No.: ITB/ZWE30/2021/02442 1 SCHEDULE OF REQUIREMENTS UN Women in Zimbabwe is supporting the establishment of mobile Spotlight Knowledge Hubs (Converted 40ft- long shipping container (11.9m - length x 2.23m - width x 2.5m - height: interior) into an office / Communication hub with 10 workstations and library) on SGBV, VAWG and SRHR as well as Gender Equality and Women’s Empowerment issues in general to provide a foundation for the development of critical gender and women's rights research, including feminist research. The mobile Spotlight Knowledge Hubs are expected to increase the number of women’s rights groups and relevant CSOs using knowledge products developed by UN Women and other participating UN agencies in the design of their own programmes on VAWG, including SGBV/HP, and on women and girls’ SRHR. They are also expected to support the training of women in business (including beneficiaries of the Spotlight Safe Markets) and girls on financial literacy and digital literacy respectively. In its physical form, each mobile Spotlight Knowledge Hub will be mainly composed of a library and a computer lab made out of a converted shipping container. UN Women is therefore seeking quotations for the supply and installation of Solar Equipment that will be used in ten (10) Spotlight Knowledge Hub units located at ZIMPOST OFFICES in Karoi (Mashonaland West Province), Epworth (Harare province), Maphisa (Matabeleland South Province) ,Chipinge (Manicaland Province), Mutasa, (Manicaland Province) , Umzingwane (Matabeleland South Province),Hopely, Tariro Youth Centre (Harare Province), Hurungwe, (Mashonaland West Province), Rushinga Post Office: (Mashonaland Central Province) and Guruve, Post Office: (Mashonaland Central Province). -

ZIMBABWE COUNTRY of ORIGIN INFORMATION (COI) REPORT COI Service
ZIMBABWE COUNTRY OF ORIGIN INFORMATION (COI) REPORT COI Service 25 March 2011 ZIMBABWE 25 MARCH 2011 Contents Preface Latest News EVENTS IN ZIMBABWE FROM 22 FEBRUARY 2011 TO 24 MARCH 2011 Useful news sources for further information REPORTS ON ZIMBABWE PUBLISHED OR ACCESSED BETWEEN 22 FEBRUARY 2011 AND 24 MARCH 2011 Paragraphs Background Information 1. GEOGRAPHY ............................................................................................................ 1.01 Public holidays ..................................................................................................... 1.06 Map ........................................................................................................................ 1.07 2. ECONOMY ................................................................................................................ 2.01 Remittances .......................................................................................................... 2.06 Sanctions .............................................................................................................. 2.08 3. HISTORY (19TH CENTURY TO 2008)............................................................................. 3.01 Matabeleland massacres 1983 - 87 ..................................................................... 3.03 Political events: late 1980s - 2007...................................................................... 3.06 Events in 2008 - 2010 ........................................................................................... 3.23 -

“Bullets for Each of You” RIGHTS State-Sponsored Violence Since Zimbabwe’S March 29 Elections WATCH
Zimbabwe HUMAN “Bullets for Each of You” RIGHTS State-Sponsored Violence since Zimbabwe’s March 29 Elections WATCH “Bullets for Each of You” State-Sponsored Violence since Zimbabwe’s March 29 Elections Copyright © 2008 Human Rights Watch All rights reserved. Printed in the United States of America ISBN: 1-56432-324-2 Cover design by Rafael Jimenez Human Rights Watch 350 Fifth Avenue, 34th floor New York, NY 10118-3299 USA Tel: +1 212 290 4700, Fax: +1 212 736 1300 [email protected] Poststraße 4-5 10178 Berlin, Germany Tel: +49 30 2593 06-10, Fax: +49 30 2593 0629 [email protected] Avenue des Gaulois, 7 1040 Brussels, Belgium Tel: + 32 (2) 732 2009, Fax: + 32 (2) 732 0471 [email protected] 64-66 Rue de Lausanne 1202 Geneva, Switzerland Tel: +41 22 738 0481, Fax: +41 22 738 1791 [email protected] 2-12 Pentonville Road, 2nd Floor London N1 9HF, UK Tel: +44 20 7713 1995, Fax: +44 20 7713 1800 [email protected] 27 Rue de Lisbonne 75008 Paris, France Tel: +33 (1)43 59 55 35, Fax: +33 (1) 43 59 55 22 [email protected] 1630 Connecticut Avenue, N.W., Suite 500 Washington, DC 20009 USA Tel: +1 202 612 4321, Fax: +1 202 612 4333 [email protected] Web Site Address: http://www.hrw.org June 2008 1-56432-324-2 “Bullets for Each of You” State-Sponsored Violence since Zimbabwe’s March 29 Elections I. Summary............................................................................................................... 1 II. Recommendations ...............................................................................................5 To the Government of Zimbabwe.........................................................................5 To the Movement for Democratic Change .......................................................... -

Country Advice Zimbabwe Zimbabwe – ZWE37118 – Harare –
Country Advice Zimbabwe Zimbabwe – ZWE37118 – Harare – Movement for Democratic Change – MDC supporters – National Youth Service – Internal relocation – Tribal groups 12 August 2010 1. Please provide information on the risk of harm to active pro-MDC supporters and activists in Zimbabwe. Please also comment on the situation for people who sympathise with or secretly support the MDC but do not openly express those views. Human Rights Watch and the US Department of State report that both perceived and known MDC members and supporters, as well as their families, continue to be harassed, arbitrarily arrested, assaulted, intimidated and killed. The perpetrators are primarily members and supporters of ZANU-PF, ZANU-PF affiliated youth militia, war veterans and, to a lesser extent, police officers and security forces. On a number of occasions, citizens have reported being “harassed or assaulted for listening to music or singing songs affiliated with the MDC-T”. ZANU-PF supporters and state security agents also reportedly “abducted and tortured dozens of opposition and civil society members, as well as student leaders, as part of an effort to intimidate MDC supporters and civil society members and leaders”. Such abductions were rarely investigated by the government. Furthermore, ZANU-PF government officials reportedly removed perceived MDC supporters from civil service positions and the military.1 Political violence against perceived ZANU-PF opponents, including citizens suspected of being sympathetic to the MDC, has continued despite the signing of a power-sharing agreement between ZANU-PF and the MDC in September 2008, and the formation of the unity government in February 2009. Throughout 2009, political violence targeting opposition MDC members and supporters resulted in at least three deaths, while at least 19 people died from injuries sustained during the 2008 election-related political violence. -
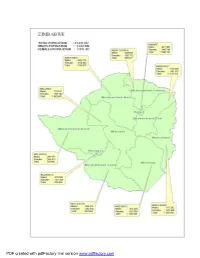
Table of Contents Table of Contents
PDF created with pdfFactory trial version www.pdffactory.com Table of Contents Table of Contents...............................................................................................................................1 Foreword...........................................................................................................................................2 Executive Summary...........................................................................................................................3 Chapter 1:..........................................................................................................................................5 Population Size and Structure.........................................................................................................5 Chapter 2:........................................................................................................................................15 Population Distribution.................................................................................................................15 Chapter 3:........................................................................................................................................22 Internal Migration.........................................................................................................................22 Chapter 4:........................................................................................................................................47 Household Characteristics.............................................................................................................47 -

Zimbabwe Urban Areas VAC
VAC Zimbabwe Urban Areas VAC Food Security and Vulnerability ZIMBABWE Vulnerability SADC FANR Assessment – September 2003 Ass essment Com mittee Vulnerability Assessment Committee Zimbabwe National Vulnerability Assessment Committee in collaboration with the SADC FANR Vulnerability Assessment Committee ZIMBABWE Some 7.5 million people (2.5 in urban areas and 5.01 million in rural areas) of the population is food insecure in 2003/04 marketing year. Urban Report No. 1 February 2004 Harare Prepared in collaboration with SIRDC – Food and Nutrition Programme, Ministry of Agriculture- National Early Warning Unit, Civil Protection Unit, CSO, MOHCW, Ministry of Public Service Labour and Social Welfare, Ministry of Education, WFP, Unicef, FEWS NET, GOAL, MEDAIR and ACF. With financial support from Government of Zimbabwe, UNDP,DFID and SADC FANR VAC For Full Report Contact: Joyce Chanetsa at [email protected]; Tel: 263 4 860320-9 or 263 11 865640, Fax 263 4860340 Elliot Vhurumuku at [email protected]; Tel: 263 4 729196 or 263 11 430397 , Fax 263 4 729196 Isaac Tarakidzwa at [email protected]; Tel 263 4 252471/3 or 263 11 412548, Fax 263 4 799214 TABLE OF CONTENTS LIST OF TABLES ............................................................................................................................... 2 LIST OF FIGURES.............................................................................................................................. 3 LIST OF APPENDICES...................................................................................................................... -

Population Census National Report 2012
Zimbabwe National Report ZIMBABWE POPULATION CENSUS 2012 Population Census Office P.O. Box CY342 Causeway Harare Tel: 04-793971-2 04-794756 E-mail: [email protected] 1 CENSUS RESULTS AT A GLANCE Male Population: 6 280 539 Female Population: 6 780 700 Total Population: 13 061 239 Annual Average Intercensal Growth Rate, 2002 –2012 (%): 1.1 Average Size of Household: 4.2 Population Density (Persons per Sq.Km): 33 2 3 Table of Contents List of Tables ...............................................................................................................................................5 Foreword.................................................................................................................................................... 10 Executive Summary ................................................................................................................................... 11 Zimbabwe Fact Sheet (Final Results).......................................................................................................... 13 Chapter 1:................................................................................................................................................... 14 Population Size and Structure.................................................................................................................. 14 Chapter 2:................................................................................................................................................... 24 Population Distribution .......................................................................................................................... -

Terms of Reference for the Procurement & Supply of Gasoline, Diesel Fuels
World Health Organization TERMS OF REFERENCE FOR THE PROCUREMENT & SUPPLY OF GASOLINE, DIESEL FUELS FOR THE UNITED NATIONS & DIPLOMATIC CORPS IN ZIMBABWE Background: The United Nations (UN) in Zimbabwe, through the World Health Organization (WHO) Local Procurement Committee will undertake the negotiated procurement of duty-free fuel (FUEL CARD, CASH, BANK TRANSFERS, BANK CARDS) for its official fleet, Staff members vehicles, generators and any operated equipment requiring fuel. This is a major operational requirement essential for delivery of services, implementation of activities benefiting various stakeholders in all Zimbabwe Provinces & Districts. The initial contract/agreement will be for a period of one (1) year with the option to renew for up to a maximum of 2 years at the discretion of WHO, subject to satisfactory performance by the contractors. Objective: The main objective of the Fuel contract/agreement is to provide the United Nations Fleet, Diplomatic Corps Fleet and Staff members with efficient, secured, convenient, continuous and steady supply of petroleum products and services, which must be economically manageable. The estimated volume of various petroleum fuel types procured by WHO Zimbabwe and participating UN agencies per year is mentioned below (this does not account for the Diplomatic Corps which is additional): Province Unleaded Petrol (Litres) Gasoil/Diesel (Litres) Harare Province 419,000 1,819,000 51,000 479,000 Bulawayo Province 101,760 Mashonaland East Province 5,500 13,000 91,000 Mashonaland West Province 71,000