Black Adherence Nodules on the Scalp Hair Shaft
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Introduction to Mycology
INTRODUCTION TO MYCOLOGY The term "mycology" is derived from Greek word "mykes" meaning mushroom. Therefore mycology is the study of fungi. The ability of fungi to invade plant and animal tissue was observed in early 19th century but the first documented animal infection by any fungus was made by Bassi, who in 1835 studied the muscardine disease of silkworm and proved the that the infection was caused by a fungus Beauveria bassiana. In 1910 Raymond Sabouraud published his book Les Teignes, which was a comprehensive study of dermatophytic fungi. He is also regarded as father of medical mycology. Importance of fungi: Fungi inhabit almost every niche in the environment and humans are exposed to these organisms in various fields of life. Beneficial Effects of Fungi: 1. Decomposition - nutrient and carbon recycling. 2. Biosynthetic factories. The fermentation property is used for the industrial production of alcohols, fats, citric, oxalic and gluconic acids. 3. Important sources of antibiotics, such as Penicillin. 4. Model organisms for biochemical and genetic studies. Eg: Neurospora crassa 5. Saccharomyces cerviciae is extensively used in recombinant DNA technology, which includes the Hepatitis B Vaccine. 6. Some fungi are edible (mushrooms). 7. Yeasts provide nutritional supplements such as vitamins and cofactors. 8. Penicillium is used to flavour Roquefort and Camembert cheeses. 9. Ergot produced by Claviceps purpurea contains medically important alkaloids that help in inducing uterine contractions, controlling bleeding and treating migraine. 10. Fungi (Leptolegnia caudate and Aphanomyces laevis) are used to trap mosquito larvae in paddy fields and thus help in malaria control. Harmful Effects of Fungi: 1. -

FUNGI Why Care?
FUNGI Fungal Classification, Structure, and Replication -Commonly present in nature as saprophytes, -transiently colonising or etiological agenses. -Frequently present in biological samples. -They role in pathogenesis can be difficult to determine. Why Care? • Fungi are a cause of nosocomial infections. • Fungal infections are a major problem in immune suppressed people. • Fungal infections are often mistaken for bacterial infections, with fatal consequences. Most fungi live harmlessly in the environment, but some species can cause disease in the human host. Patients with weakened immune function admitted to hospital are at high risk of developing serious, invasive fungal infections. Systemic fungal infections are a major problem among critically ill patients in acute care settings and are responsible for an increasing proportion of healthcare- associated infections THE IMPORTANCE OF FUNGI • saprobes • symbionts • commensals • parasites The fungi represent a ubiquitous and diverse group of organisms, the main purpose of which is to degrade organic matter. All fungi lead a heterotrophic existence as saprobes (organisms that live on dead or decaying matter), symbionts (organisms that live together and in which the association is of mutual advantage), commensals (organisms living in a close relationship in which one benefits from the relationship and the other neither benefits nor is harmed), or as parasites (organisms that live on or within a host from which they derive benefits without making any useful contribution in return; in the case of pathogens, the relationship is harmful to the host). Fungi have emerged in the past two decades as major causes of human disease, especially among those individuals who are immunocompromised or hospitalized with serious underlying diseases. -

Trichosporon Beigelii Infection Presenting As White Piedra and Onychomycosis in the Same Patient
Trichosporon beigelii Infection Presenting as White Piedra and Onychomycosis in the Same Patient Lt Col Kathleen B. Elmer, USAF; COL Dirk M. Elston, MC, USA; COL Lester F. Libow, MC, USA Trichosporon beigelii is a fungal organism that causes white piedra and has occasionally been implicated as a nail pathogen. We describe a patient with both hair and nail changes associated with T beigelii. richosporon beigelii is a basidiomycetous yeast, phylogenetically similar to Cryptococcus.1 T T beigelii has been found on a variety of mammals and is present in soil, water, decaying plants, and animals.2 T beigelii is known to colonize normal human skin, as well as the respiratory, gas- trointestinal, and urinary tracts.3 It is the causative agent of white piedra, a superficial fungal infection of the hair shaft and also has been described as a rare cause of onychomycosis.4 T beigelii can cause endo- carditis and septicemia in immunocompromised hosts.5 We describe a healthy patient with both white piedra and T beigelii–induced onychomycosis. Case Report A 62-year-old healthy man who worked as a pool maintenance employee was evaluated for thickened, discolored thumb nails (Figure 1). He had been aware of progressive brown-to-black discoloration of the involved nails for 8 months. In addition, soft, light yellow-brown nodules were noted along the shafts of several axillary hairs (Figure 2). Microscopic analysis of the hairs revealed nodal concretions along the shafts (Figure 3). No pubic, scalp, eyebrow, eyelash, Figure 1. Onychomycotic thumb nail. or beard hair involvement was present. Cultures of thumb nail clippings on Sabouraud dextrose agar grew T beigelii and Candida parapsilosis. -

Boards' Fodder
boards’ fodder Medical Mycology By Adriana Schmidt, MD, and Natalie M. Curcio, MD, MPH. (Updated July 2015*) SUPERFICIAL ORGANISM CLINICAL HISTO/KOH TREATMENT MYCOSES* Pityriasis Malessezia furfur Hypo- or hyper-pigmented Spaghetti & meatballs: Antifungal shampoos and/or versicolor macules short hyphae + yeast PO therapy Tinea nigra Hortaea werneckii (formerly Brown-black non-scaly Branching septate hyphae Topical imidazoles or palmaris Phaeoannellomyces werneckii) macules + budding yeast allylamines Black piedra Piedraia hortae Hard firm black Dark hyphae around concretions acrospores Cut hair off, PO terbinafine, White piedra Trichosporon ovoides or inkin Soft loose white Blastoconidia, imidazoles, or triazoles (formely beigelii) concretions arthroconidia Fluorescent small Microsporum Canis KOH: spores on outside spore ectothrix: M. audouinii of the hair shaft; “Cats And Dogs M. distortum Wood’s lamp --> yellow Sometimes Fight T. schoenleinii fluorescence & Growl” M. ferrugineum+/- gypseum Large spore Trichophyton spp. (T. tonsurans in North America; T. violaceum in KOH: spores within hair Topical antifungals; PO endothrix Europe, Asia, parts of Africa). shaft antifungals for T. manuum, Tinea corporis T. rubrum > T. mentag. Majocchi’s granuloma: T. rubrum capitis, unguium T. pedis Moccasin: T. rubrum, E. floccosum. Interdigital/vesicular: T. mentag T. unguium Distal lateral, proximal and proximal white subungual: T. rubrum. White superficial: T. mentag. HIV: T. rubrum SUBQ MYCOSES** ORGANISM TRANSMISSION CLINICAL HISTO/KOH TREATMENT -

Histopathology of Important Fungal Infections
Journal of Pathology of Nepal (2019) Vol. 9, 1490 - 1496 al Patholo Journal of linic gist C of of N n e o p ti a a l- u i 2 c 0 d o n s 1 s 0 a PATHOLOGY A m h t N a e K , p d of Nepal a l a M o R e d n i io ca it l A ib ss xh www.acpnepal.com oc g E iation Buildin Review Article Histopathology of important fungal infections – a summary Arnab Ghosh1, Dilasma Gharti Magar1, Sushma Thapa1, Niranjan Nayak2, OP Talwar1 1Department of Pathology, Manipal College of Medical Sciences, Pokhara, Nepal. 2Department of Microbiology, Manipal College of Medical Sciences , Pokhara, Nepal. ABSTRACT Keywords: Fungus; Fungal infections due to pathogenic or opportunistic fungi may be superficial, cutaneous, subcutaneous Mycosis; and systemic. With the upsurge of at risk population systemic fungal infections are increasingly common. Opportunistic; Diagnosis of fungal infections may include several modalities including histopathology of affected tissue Systemic which reveal the morphology of fungi and tissue reaction. Fungi can be in yeast and / or hyphae forms and tissue reactions may range from minimal to acute or chronic granulomatous inflammation. Different fungi should be differentiated from each other as well as bacteria on the basis of morphology and also clinical correlation. Special stains like GMS and PAS are helpful to identify fungi in tissue sections. INTRODUCTION Correspondence: Dr Arnab Ghosh, MD Fungal infections or mycoses may be caused by Department of Pathology, pathogenic fungi which infect healthy individuals or by Manipal College of Medical Sciences, Pokhara, Nepal. -

Two Cases of Scalp White Piedra Caused by Trichosporon Ovoides
Case TTwowo ccasesases ooff sscalpcalp wwhitehite ppiedraiedra causedcaused byby Report TTrichosporonrichosporon ovoidesovoides SSwagatawagata AA.. TTambe,ambe, SS.. RRachitaachita DDhurat,hurat, CChayahaya A.A. KKumarumar1, PPreetireeti TThakare,hakare, NNitinitin LLade,ade, HHemangiemangi Jerajani,Jerajani, MMeenakshieenakshi MathurMathur 1 Departments of Dermatology ABSTRACT and 1Microbiology, Lokmanya Tilak Municipal Medical White piedra is a superÞ cial fungal infection of the hair shaft, caused by Trichosporon beigelii. College and General Hospital, Sion Mumbai - 400 022, India We report two cases of white piedra presenting as brown palpable nodules along the hair shaft with a fragility of scalp hairs. T. beigelii was demonstrated in hair culture of both the patients Address for correspondence: and T. ovoides as a species was conÞ rmed on carbohydrate assimilation test. The Þ rst patient Dr. Swagata Arvind Tambe, responded to oral itraconazole and topical ketoconazole, with a decrease in the palpability of 19/558, Udyan Housing nodules and fragility of scalp hairs at the end of two months. Society, Nehru Nagar, Kurla (East), Key words: White piedra, Carbohydrate assimilation test, Itraconazole, Trichosporon ovoides Mumbai – 400 024, India. E-mail: [email protected] DOI: 10.4103/0378-6323.51256 PMID: 19439885 IINTRODUCTIONNTRODUCTION with fragility for 3 and 2 months, respectively. Both the patients had a history of tying wet hairs after washing. White piedra is a superficial fungal infection of Other hairy parts of the body were not similarly the hair shaft, caused by Trichosporon beigelii, also affected in both. Their family members had no similar known as tinea nodosa, trichosporonosis nodosa involvement. Both had never visited southern parts of and trichomycosis nodularis.[1] Common areas of India or used oils excessively. -

Department of Biological Sciences Redeemer's
DEPARTMENT OF BIOLOGICAL SCIENCES REDEEMER’S UNIVERSITY MCB 313 PATHOGENIC MYCOLOGY DURUGBO ERNEST UZODIMMA (Ph.D.) COURSE OUTLINE 1. Introduction 2. Structure, reproduction and classification of pathogenic Fungi Eg. Aspergillus, Trichphyton spp., Tinea spp.,Yeasts 3.Superficial systematic mycoses and antimycoses 4. Fungal infections ( Candidiasis , Histoplasmosis etc) 5. Laboratory methods of study 5. Pathology and immunology 6. Cultivation techniques in Mycology Structure, Reproduction and Classification of Pathogenic Fungi About 30% of the 100,000 known species of Fungi make a living as parasites, or pathogens , mostly of plants. E. g Cryphonectria parasitica, the Ascomycete fungus causes chestnut blight. Fusarium circinatum causes pith pine canker a diseae that threatens pine worldwide. Puccinia graminis causes black stem rust of wheat. Some of the fungi that attack food crops are toxic to humans for example certain species of the ascomycete mold Aspergillus contaminate improperly stored grain and peanuts by secreting aflatoxins which are carcinogenic. The ascomycete Claviceps purpurea which grows on rye plants forming purple structures called ergots. If diseased rye is milled into flour and consumed it causes ergotism, a condition characterized by gangrene, nervous spasms, burning sensations, hallucinations, and temporary insanity. An epidemic of this around 944 C.E, killed more than 40,000 people in France. Animals are much less susceptible to parasitic fungi than plants. Only about 50 species of fungi are known to parasitize humans and animals . Such fungal infections are mycosis . Skin mycoses includes ringworm. The ascomycetes that causes ringworm can infect almost any skin surface. Most commonly, they grow on the feet, causing the intense itching and blisters known as athlete ’s foot. -

Essential Oils of Lamiaceae Family Plants As Antifungals
biomolecules Review Essential Oils of Lamiaceae Family Plants as Antifungals Tomasz M. Karpi ´nski Department of Medical Microbiology, Pozna´nUniversity of Medical Sciences, Wieniawskiego 3, 61-712 Pozna´n,Poland; [email protected] or [email protected]; Tel.: +48-61-854-61-38 Received: 3 December 2019; Accepted: 6 January 2020; Published: 7 January 2020 Abstract: The incidence of fungal infections has been steadily increasing in recent years. Systemic mycoses are characterized by the highest mortality. At the same time, the frequency of infections caused by drug-resistant strains and new pathogens e.g., Candida auris increases. An alternative to medicines may be essential oils, which can have a broad antimicrobial spectrum. Rich in the essential oils are plants from the Lamiaceae family. In this review are presented antifungal activities of essential oils from 72 Lamiaceae plants. More than half of these have good activity (minimum inhibitory concentrations (MICs) < 1000 µg/mL) against fungi. The best activity (MICs < 100) have essential oils from some species of the genera Clinopodium, Lavandula, Mentha, Thymbra, and Thymus. In some cases were observed significant discrepancies between different studies. In the review are also shown the most important compounds of described essential oils. To the chemical components most commonly found as the main ingredients include β-caryophyllene (41 plants), linalool (27 plants), limonene (26), β-pinene (25), 1,8-cineole (22), carvacrol (21), α-pinene (21), p-cymene (20), γ-terpinene (20), and thymol (20). Keywords: Labiatae; fungi; Aspergillus; Cryptococcus; Penicillium; dermatophytes; β-caryophyllene; sesquiterpene; monoterpenes; minimal inhibitory concentration (MIC) 1. Introduction Fungal infections belong to the most often diseases of humans. -
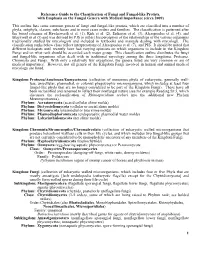
Reference Guide to the Classification of Fungi and Fungal-Like Protists, with Emphasis on the Fungal Genera with Medical Importance (Circa 2009)
Reference Guide to the Classification of Fungi and Fungal-like Protists, with Emphasis on the Fungal Genera with Medical Importance (circa 2009) This outline lists some common genera of fungi and fungal-like protists, which are classified into a number of phyla, subphyla, classes, subclasses and in most cases orders and families. The classification is patterned after the broad schemes of Hawksworth et al. (1), Kirk et al. (2), Eriksson et al. (3), Alexopoulos et al. (4), and Blackwell et al (5) and was devised by PJS to reflect his perception of the relationships of the various organisms traditionally studied by mycologists and included in textbooks and manuals dealing with mycology. The classification ranks below class reflect interpretations of Alexopoulos et al. (7), and PJS. It should be noted that different biologists until recently have had varying opinions on which organisms to include in the Kingdom Fungi and on what rank should be accorded each major group. This classification outline distributes the fungi and fungal-like organisms often dealt with in traditional mycology among the three kingdoms, Protozoa, Chromista and Fungi. With only a relatively few exceptions, the genera listed are very common or are of medical importance. However, not all genera of the Kingdom Fungi involved in human and animal medical mycology are listed. Kingdom: Protozoa/Amebozoa/Eumycetozoa (collection of numerous phyla of eukaryotic, generally wall- less, unicellular, plasmodial, or colonial phagotrophic microorganisms, which includes at least four fungal-like phyla that are no longer considered to be part of the Kingdom Fungi). These have all been reclassified and renamed to reflect their nonfungal nature (see for example Reading Sz 5, which discusses the reclassification of Rhinosporidium seeberi into the additional new Phylum Mezomycetozoea). -

Growth and Morphology of Piedraia Hortae (Brumpt) Fonseca and a R & Leao: the Causal Agent of Black Piedra
I ' i I- 77-2426 JONES, Jeanette, 1950- GROWTH AND MORPHOLOGY OF PIEDRAIA HORTAE (BRUMPT) FONSECA AND A R & LEAO: THE CAUSAL AGENT OF BLACK PIEDRA. The Ohio State University, Ph.D., 1976 Botany Xerox University Microfilms,Ann Arbor, Michigan 48106 © 1976 JEANETTE JONES ALL RIGHTS RESERVED Growth and Morphology of Piedraia hortaa (Brumpt) Fonseca and Area Leao The Causal Agent of Black Piedra Dissertation Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University hy Jeanette Jones, B. Sc., M. Sc, The Ohio State University 1976 Reading Committee Approved by J. A, Schmitt, Chairman M* 0. Garraway Adviser V, Raghavan Department of Botany R. L. Seymour C. E. Taft ••..the fungi are not degenerate organisms which are on their way out in a scheme of evolution, and so of little economic importance and scientific interest. The fungi, on the contrary, are progressive, ever changing and evolving rapidly in their own way so that they are capable of becoming readily adapted to every condition of life. We may rest assured that as Green Plants and Animals disappear one by one from the face of the globe, some of the fungi will always be present to dispose of the last remains. B. 0. Dodge (1939) ii ACKNOWLEDGEMENTS I am particularly indebted to Dr. J. A Schmitt for his guidance and support when they were needed most. A special thanks is extended to the members of the reading committee, Dr. J. A. Schmitt, Dr. M. 0. Garraway, Dr. V. Raghavan, Dr. -

Fungal Infections
Fungal infections Natural defence against fungi y Fatty acid content of the skin y pH of the skin, mucosal surfaces and body fluids y Epidermal turnover y Normal flora Predisposing factors y Tropical climate y Manual labour population y Low socioeconomic status y Profuse sweating y Friction with clothes, synthetic innerwear y Malnourishment y Immunosuppressed patients HIV, Congenital Immunodeficiencies, patients on corticosteroids, immunosuppressive drugs, Diabetes Fungal infections: Classification y Superficial cutaneous: y Surface infections eg. P.versicolor, Dermatophytosis, Candidiasis, T.nigra, Piedra y Subcutaneous: Mycetoma, Chromoblastomycosis, Sporotrichosis y Systemic: (opportunistic infection) Histoplasmosis, Candidiasis Of these categories, Dermatophytosis, P.versicolor, Candidiasis are common in daily practice Pityriasis versicolor y Etiologic agent: Malassezia furfur Clinical features: y Common among youth y Genetic predisposition, familial occurrence y Multiple, discrete, discoloured, macules. y Fawn, brown, grey or hypopigmented y Pinhead sized to large sheets of discolouration y Seborrheic areas, upper half of body: trunk, arms, neck, abdomen. y Scratch sign positive PITYRIASIS VERSICOLOR P.versicolor : Investigations y Wood’s Lamp examination: y Yellow fluorescence y KOH preparation: Spaghetti and meatball appearance Coarse mycelium, fragmented to short filaments 2-5 micron wide and up to 2-5 micron long, together with spherical, thick-walled yeasts 2-8 micron in diameter, arranged in grape like fashion. P.versicolor: Differential diagnosis y Vitiligo y Pityriasis rosea y Secondary syphilis y Seborrhoeic dermatitis y Erythrasma y Melasma Treatment P. versicolor Topical: y Ketoconazole , Clotrimazole, Miconazole, Bifonazole, Oxiconazole, Butenafine,Terbinafine, Selenium sulfide, Sodium thiosulphate Oral: y Fluconazole 400mg single dose y Ketoconazole 200mg OD x 14days yGriseofulvin is NOT effective. -

White Concretions on the Hair Shaft
PHOTO CHALLENGE White Concretions on the Hair Shaft Melinda Liu, MD; Alex G. Ortega-Loayza, MD A 35-year-old woman presented with possible nits on the hair of 1 year’s duration. She was previously evaluated by several outside medical providers and was unsuccessfully treated with topical and systemic medications for pedicu- losis. She reported sporadic scalp pruritus but denied hair loss, breakage, close contacts with similar symptoms, or recent travel outside the United States. She was otherwise healthy and was not takingcopy any medications. Physical examination revealed small 1- to 2-mm, general- ized, somewhat detachable, white concretions randomly distributed on the hair shafts. No brokennot hairs were observed. The eyebrows, eyelash hairs, and surrounding skin were normal. Potassium hydroxide mount was Doequivocal for nits. WHAT’S THE DIAGNOSIS? a. hair cast b. resistant pediculosis c. tinea capitis d. trichobacteriosis CUTIS e. white piedra PLEASE TURN TO PAGE E9 FOR THE DIAGNOSIS Dr. Liu was from the Baylor College of Medicine, Houston, Texas, and currently is from the Department of Dermatology, University of Texas Southwestern Medical Center, Dallas. Dr. Ortega-Loayza is from the Department of Dermatology, Oregon Health and Science University, Portland. The authors report no conflict of interest. Correspondence: Melinda Liu, MD, Department of Dermatology, UT Southwestern Medical Center, 5323 Harry Hines Blvd, Dallas, TX 75390-9069 ([email protected]). E8 I CUTIS® WWW.MDEDGE.COM/DERMATOLOGY Copyright Cutis 2019. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. PHOTO CHALLENGE DISCUSSION THE DIAGNOSIS: White Piedra fungal culture demonstrated a filamentous fungus casts.9,10 Thus, when a potassium hydroxide mount is that was identified as Trichosporon inkin via DNA equivocal for nits and dermoscopy demonstrates concre- A sequencing, which confirmed the diagnosis of tions that completely encircle the hair shaft, it is important to white piedra (WP).