Using an Improvement Method to Review Transfers of Care Seven Days a Week
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
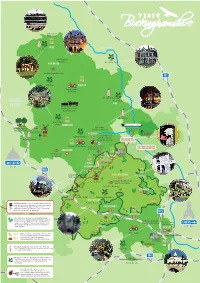
Buckinghamshire Attractions
Silverstone Race Track Stowe Milton Keynes Stowe Buckingham Old Gaol Buckingham Bletchley Park Buckingham Brewery M1 Claydon winslow Green Dragon Eco Farm Aylesbury Vale Bicester Ascot House village Wing Buckinghamshire Railway Centre Mentmore Waddesdon Manor Waddesdon Aylesbury Bernwood Royal Grebe Canal Waterside Theatre Hunting Forest Cruises Vale Brewery Aylesbury Ashridge County Museum Brill Hartwell House and Roald Dahl Magnolia Park Children’s Gallery Ickneild way Orchard View Farm Stoke Mandeville Grand union Canal Haddenham Guttman Centre XT Brewing The Chiltern Company Wendover Brewery OXFORD Princes Coombe Hill Risborough M40 Whiteleaf Chinnor and Princes Great missenden Risborough Railway chesham Lacey Green Roald Dahl Museum and Story Centre Malt The Brewery Amersham Red Kite viewing point Hughenden Manor west wycombe Buckinghamshire is one of the most filmed counties Hellfire Caves with blockbuster such Harry Potter and James Bond, The Artichoke together with the popular television series high wycombe Midsummer Murders using it’s scenic countryside and historic buildings as backdrops. M25 beaconsfield The Chilterns is an Area of Outstanding Natural Beauty ideal for walkers and bikers and an excellent Bekonscot Model viewpoint to spot Redkites. It’s the only AONB that The Rebellion Chiltern Open can be reached by the London Underground, is the Beer Company Village and Railway London 4th largest in the UK and has over 12,000 miles of Air Museum walks within it. Marlow denham The Hand Odds Farm With a thriving community of independent and Flowers food and drink providers, farmers markets Buckinghamshire and Michellin Starred restaurants, Buckinghamshire is a food lovers heaven. Stoke Park Iver Buckinghamshire has more golf courses than any other county in England. -

Aylesbury Vale Community Chest Grants April 2014 - March 2015
Aylesbury Vale Community Chest Grants April 2014 - March 2015 Amount Granted Total Cost Award Aylesbury Vale Ward Name of Organisation £ £ Date Purpose Area Buckinghamshire County Local Areas Artfully Reliable Theatre Society 1,000 1,039 Sep-14 Keyboard for rehearsals and performances Aston Clinton Wendover Aylesbury & District Table Tennis League 900 2,012 Sep-14 Wall coverings and additional tables Quarrendon Greater Aylesbury Aylesbury Astronomical Society 900 3,264 Aug-14 new telescope mount to enable more community open events and astrophotography Waddesdon Waddesdon/Haddenham Aylesbury Youth Action 900 2,153 Jul-14 Vtrek - youth volunteering from Buckingham to Aylesbury, August 2014 Vale West Buckingham/Waddesdon Bearbrook Running Club 900 1,015 Mar-15 Training and raceday equipment Mandeville & Elm Farm Greater Aylesbury Bierton with Broughton Parish Council 850 1,411 Aug-14 New goalposts and goal mouth repairs Bierton Greater Aylesbury Brill Memorial Hall 1,000 6,000 Aug-14 New internal and external doors to improve insulation, fire safety and security Brill Haddenham and Long Crendon Buckingham and District Mencap 900 2,700 Feb-15 Social evenings and trip to Buckingham Town Pantomime Luffield Abbey Buckingham Buckingham Town Cricket Club 900 1,000 Feb-15 Cricket equipment for junior section Buckingham South Buckingham Buckland and Aston Clinton Cricket Club 700 764 Jun-14 Replacement netting for existing practice net frames Aston Clinton Wendover Bucks Play Association 955 6,500 Apr-14 Under 5s area at Play in The Park event -

5 Year Housing Land Supply Position Statement June 2018
Aylesbury Vale District Council - Five year housing land supply position statement, June 2018 Purpose of this position statement 1.0 Paragraph 47-49 of the National Planning Policy Framework (NPPF, 2012) requires local planning authorities to identify and keep up-to-date a deliverable five year housing land supply against their housing requirements. Where the Council cannot demonstrate a 5 year housing land supply, there is a presumption in favour of sustainable development in line with the NPPF (para 14). Having an understanding of supply is also key to fulfilling the NPPF requirement to demonstrate the expected rate of housing delivery and how housing targets will be met (paragraph 47). 1.1 This position statement sets out the approach to meeting housing requirements in Aylesbury Vale pending the adoption of the new Local Plan (the Vale of Aylesbury Local Plan, VALP). This statement sets out how the current housing supply has been calculated, and the housing requirement target, to be used by the Council in order to apply the appropriate development plan policy tests and the tests set out in the NPPF when determining relevant planning applications in the period before VALP is adopted. 1.2 The five year housing land supply calculation is dynamic and changes as planning permissions are granted and as existing commitments are completed. Therefore it is important that any developer considering submitting a planning application should consider the latest position on the five year housing supply calculation from the Council. It is intended that the position statement is a living draft that will be regularly updated as the evidence emerges through the Local Plan preparation processes. -

Buckinghamshire and Oxfordshire Summer 2021 3-Month Construction Look Ahead
Buckinghamshire and Oxfordshire Summer 2021 3-month construction look ahead Buckinghamshire and Oxfordshire Summer 2021 This forward look covers HS2 associated work in Buckinghamshire and Oxfordshire. The document includes: • A forward look of construction activities planned in the next three months • Works to be aware of that will take place in the next 12 months, but may not yet have been confirmed The dates and information included in the forward look are subject to change as programme develops. These will be updated in the next edition of the forward look. If you have any queries about the information in this forward look, the HS2 Helpdesk is available all day, every day on 08081 434 434 or by emailing [email protected] Page 2 Buckinghamshire and Oxfordshire Contents Map 1 – Turweston to Mixbury................................................................................................ 4 Map 2 – Finmere to Twyford .................................................................................................... 7 Map 3 – Calvert ....................................................................................................................... 10 Map 4 – Quainton ................................................................................................................... 12 Map 5 – Waddesdon to Stoke Mandeville ............................................................................ 14 Map 6 – Wendover ................................................................................................................. -

This Level Site Is Occupied by a Detached Bungalow Built in the 1920S Which Remains Largely Original
This level site is occupied by a detached bungalow built in the 1920s which remains largely original. There is a drive for this from the A413. Measuring with Promap the land amounts to .9958 acres. Subject to planning there is scope for redevelopment with at least two or three houses but possibly a comprehensive development. Furthermore the gardens of adjoining houses give possible additional development land. The owners of 123 Wendover Road have instructed Christopher Pallet to seek proposals for their property as a separate transaction. The verge to the south of Arnold Close has been retained by the developers and could provide a potential further access. Please discuss with us. With a view to encouraging applicants to submit attractive offers the Executors are not intending to apply an uplift clause or ransom strip along the boundary with 123 Wendover Road. However they may decide to include such provision if offers do not meet their expectations. A ransom strip will be retained along the rear boundary. One Acre of Potential Building Land 121 Wendover Road, Stoke Mandeville, Aylesbury, Buckinghamshire HP22 5TD GUIDE PRICE £650,000 Chartered Surveyors Location Services The site fronts the A413 Wendover Road on the outskirts The existing bungalow is connected to water and electricity. of the village of Stoke Mandeville some 2¼ miles from All services are believed to be available in Wendover the centre of the County Town of Aylesbury and Road and Arnold Close. 2½ miles from the small town of Wendover. Stoke No enquiries as to the capacity and availability of Mandeville is a medium size village with a local shop/ services have been made. -
Download Original Attachment
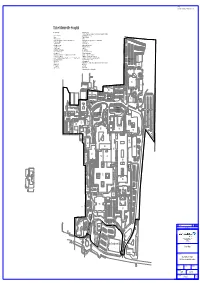
NOTES: Do not scale from drawing. Check all dimensions on site. Stoke Mandeville Hospital Building No. Legend 73 Haematology Dept. 74 Health Care Safety Team, Occupational Health, Backcare Safety Advisors & Finance 2. Gardeners Workshop 75 National Spinal Injuries Center 3 Empty 77 Man Med Pharmacy 29 Pathology Laboratories 79 Empty 36 Estates Dept. Workshops, General Stores & Sodexo Hard Services 80 Sodexo Soft Services, Property Services, General Administration 37 Estates Dept. Offices. 81 X-Ray Extension 41 Hydrotherapy Pool 83 Pathology Extension 48 Occupational Therapy 84 Florence Nightingale Hospice 49 Occupational Annex 85 Outpatients Extension 54 Floyd Auditorium 86 Maternity 55 David Brown Hall of Residence 86B Maternity Pod 56 Duke of Edinburgh Lounge 88 Day Nursery (Private Owned) 57 Ophthalmic Unit 89 Cancer Care Hematology 67 John Hampden Unit (Oxfordshire, Buckinghamshire Mental Health Trust) 90 Aston House Doctors Accommodation 68 Trust Management Offices 91 Main Entrance, Catering & Administration (PFI) 69 A & E, ITU, Out Patients, Theatres, Wards 11, 12, 20, 21, 22, 23, X-Ray Phase 1, IT 92 Wards 1 - 9, Pharmacy, Day Surgery, Endoscopy (PFI) Dept. & Clinical Administration 93 Ward 10, Medical Records & Mortuary Willows Car 69A Service Tower 94 ADL Bungalow (PFI) Park 69B Service Tower 95 Mandeville Wing - Ophthalmic Theatres, Ophthalmic Outpatinets, Ward 14 & General 70 Energy Center Administration 71 Transport Dept. 96 Renal Unit 72 Sterile Services H1 Pharmacy QC R6 Harrington House Student Accommodation Aston House -

BUCKINGHAMSHIRE POSSE COMITATUS 1798 the Posse Comitatus, P
THE BUCKINGHAMSHIRE POSSE COMITATUS 1798 The Posse Comitatus, p. 632 THE BUCKINGHAMSHIRE POSSE COMITATUS 1798 IAN F. W. BECKETT BUCKINGHAMSHIRE RECORD SOCIETY No. 22 MCMLXXXV Copyright ~,' 1985 by the Buckinghamshire Record Society ISBN 0 801198 18 8 This volume is dedicated to Professor A. C. Chibnall TYPESET BY QUADRASET LIMITED, MIDSOMER NORTON, BATH, AVON PRINTED IN GREAT BRITAIN BY ANTONY ROWE LIMITED, CHIPPENHAM, WILTSHIRE FOR THE BUCKINGHAMSHIRE RECORD SOCIETY CONTENTS Acknowledgments p,'lge vi Abbreviations vi Introduction vii Tables 1 Variations in the Totals for the Buckinghamshire Posse Comitatus xxi 2 Totals for Each Hundred xxi 3-26 List of Occupations or Status xxii 27 Occupational Totals xxvi 28 The 1801 Census xxvii Note on Editorial Method xxviii Glossary xxviii THE POSSE COMITATUS 1 Appendixes 1 Surviving Partial Returns for Other Counties 363 2 A Note on Local Military Records 365 Index of Names 369 Index of Places 435 ACKNOWLEDGMENTS The editor gratefully acknowledges the considerable assistance of Mr Hugh Hanley and his staff at the Buckinghamshire County Record Office in the preparation of this edition of the Posse Comitatus for publication. Mr Hanley was also kind enough to make a number of valuable suggestions on the first draft of the introduction which also benefited from the ideas (albeit on their part unknowingly) of Dr J. Broad of the North East London Polytechnic and Dr D. R. Mills of the Open University whose lectures on Bucks village society at Stowe School in April 1982 proved immensely illuminating. None of the above, of course, bear any responsibility for any errors of interpretation on my part. -

61/61A Aylesbury
Aylesbury - Tring - Ivinghoe - Dunstable 61/61A MONDAY TO FRIDAY From: 29 July 2018 Service number: 61 164 61A 61 61 61A 61 61A 61 61 61 61 Notes: RL sch Nsch sch Nsch Aylesbury Bus Station 0620 0730 743 905 1035 1205 1405 1550 1600 1735 1900 Aylesbury, Schools Coach Park |||||||1557 | | | Elm Farm, opp Shops ||||1044 | 1414 | | | | Bedgrove, Jansel Square | 0740 | | 1049 | 1419 | | | | Stoke Mandeville, Station Road | 0743 ||||||||| Aston Clinton, The Bell 0630 | 0756 0918 1055 1218 1425 1615 1615 1752 1911 Wendover, Clock Tower | 0750 ||||||||| RAF Halton, Main Point | 0754 ||||||||| Tring, Church Square 0638 0808 0808 0928 1105 1228 1435 1625 1625 1802 1920 New Mill, Elizabeth Drive 0641 0812 0812 0932 1109 1232 1439 1629 1629 1806 1924 Pitstone, Harlech Road 0646 0817 0817 0937 1114 1237 1444 1634 1634 1811 1929 Pitstone, opp Playing Fields 0608 0647 0818 0818 0938 1115 1238 1445 1635 1635 1812 1930 Ivinghoe, The Green 0612 0654 0823 0823 0945 1122 1245 1450 1640 1640 1817 1937 Edlesborough, Playing Fields 0621 0832 0832 0954 1131 1254 1459 1650 1650 1827 Eaton Bray, White Horse 0625 0837 0837 0958 1135 1258 1503 1654 1654 1831 Tottenhoe, Church End 0630 0844 0844 1002 1139 1302 1507 1700 1700 1837 Dunstable, Church Street 0637 0855 0852 1012 1149 1312 1517 1712 1712 1845 Dunstable, ASDA 0640 0900 0857 1017 1154 1317 1522 1717 1717 1848 SATURDAY Service number 61 61 61 61 61A 61 61 61 Aylesbury, Bus Station 0740 0905 1035 1205 1405 1535 1735 1900 Elm Farm, opp Shops ||||1414 | || Bedgrove, Jansel Square ||||1419 | || Aston Clinton, -

Covid-19 App)
EDLESBOROUGH PARISH COUNCIL In the first instance parishioners should refer to www.gov.uk/coronavirus as this has the most up to date information. Stay safe, protect Bucks We know Covid isn’t over, we know that risks remain, and whilst it feels like we’re entering a new phase in this pandemic, with the current rise in cases none of us can be sure of what lies ahead in the coming weeks and months. Please remember that even if you’ve been vaccinated, you can still catch and still spread Covid- 19, sometimes without knowing it. The Pastoral Team at St Mary’s, Eaton Bray and The Eaton Bray Good Neighbours Scheme also cover Edlesborough and Northall. If you know anyone living close to you who is not online or “internet savvy” please contact the Edlesborough Parish Clerk (01525 29358) for a printed version of this information. Email: [email protected] 01525 229358 Website: www.edlesborough-pc.gov.uk Facebook: www.facebook.com/EDANParishCouncil EDLESBOROUGH PARISH COUNCIL Here is a link to a Universal Credit guide which some parishioners may find useful https://www.jobcentrenearme.com/universal-credit/ Email: [email protected] 01525 229358 Website: www.edlesborough-pc.gov.uk Facebook: www.facebook.com/EDANParishCouncil EDLESBOROUGH PARISH COUNCIL Update from Martin Tett, Leader of Buckinghamshire Council 16 July 2021 Dear Resident, By now I think that we are all aware that on Monday (19 July), England will move to the final stage of the roadmap for unlocking and all current laws and restrictions around Covid will be lifted. -

165 Bus Time Schedule & Line Route
165 bus time schedule & line map 165 Aylesbury - Leighton Buzzard View In Website Mode The 165 bus line (Aylesbury - Leighton Buzzard) has 3 routes. For regular weekdays, their operation hours are: (1) Aylesbury: 7:20 AM - 5:10 PM (2) Leighton Buzzard: 8:45 AM - 3:45 PM (3) Wing: 2:30 PM Use the Moovit App to ƒnd the closest 165 bus station near you and ƒnd out when is the next 165 bus arriving. Direction: Aylesbury 165 bus Time Schedule 51 stops Aylesbury Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 7:20 AM - 5:10 PM West Street, Leighton Buzzard 7 Waterborne Walk, Leighton Buzzard Tuesday 7:20 AM - 5:10 PM Tesco, Leighton Buzzard Wednesday 7:20 AM - 5:10 PM Stoke Road, Linslade Thursday 7:20 AM - 5:10 PM 22 New Road, Leighton Buzzard Friday 7:20 AM - 5:10 PM Old Road, Linslade Saturday 9:40 AM - 4:40 PM 15 Soulbury Road, Leighton Buzzard Southcourt Road, Linslade Southcourt Road, Leighton Buzzard 165 bus Info Railway Bridge, Linslade Direction: Aylesbury Stops: 51 Tollgate House, Wing Trip Duration: 52 min Line Summary: West Street, Leighton Buzzard, Ascott House, Wing Tesco, Leighton Buzzard, Stoke Road, Linslade, Old Road, Linslade, Southcourt Road, Linslade, Railway Well Lane, Wing Bridge, Linslade, Tollgate House, Wing, Ascott House, Wing, Well Lane, Wing, Soulbury Turn, Wing, Soulbury Turn, Wing Crossroads, Cublington, Hay Barn Business Park, Warwick Drive, Wing Aston Abbotts, The Green, Aston Abbotts, Wingrave Road, Aston Abbotts, Crossroads, Wingrave, Crossroads, Cublington Winslow Road, Wingrave, Parsonage -

50 Bus Time Schedule & Line Route
50 bus time schedule & line map 50 Aylesbury - Elm Farm - Wendover - Halton View In Website Mode The 50 bus line (Aylesbury - Elm Farm - Wendover - Halton) has 2 routes. For regular weekdays, their operation hours are: (1) Aylesbury: 6:55 AM - 6:36 PM (2) Halton: 7:40 AM - 6:40 PM Use the Moovit App to ƒnd the closest 50 bus station near you and ƒnd out when is the next 50 bus arriving. Direction: Aylesbury 50 bus Time Schedule 29 stops Aylesbury Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 6:55 AM - 6:36 PM Main Point, Halton Tuesday 6:55 AM - 6:36 PM Trinity Church, Halton Wednesday 6:55 AM - 6:36 PM Veterinary Surgery, Halton Thursday 6:55 AM - 6:36 PM Portal Road, Wendover Civil Parish Friday 6:55 AM - 6:36 PM The Rose & Crown Ph, Wendover Saturday 8:12 AM - 5:12 PM Tring Road Shops, Wendover B4009, Wendover Clock Tower, Wendover 20 Aylesbury Road, Wendover 50 bus Info Direction: Aylesbury Health Centre, Wendover Stops: 29 Trip Duration: 26 min Perry Street, Wendover Line Summary: Main Point, Halton, Trinity Church, Addington Cottages, Wendover Halton, Veterinary Surgery, Halton, The Rose & Crown Ph, Wendover, Tring Road Shops, Wendover, Nursing Home, World's End Clock Tower, Wendover, Health Centre, Wendover, Perry Street, Wendover, Nursing Home, World's End, Castle Park Road, Wendover Castle Park Road, Wendover, The Village Gate, World's End, Church Lane, Weston Turville, The The Village Gate, World's End Chandos Arms Ph, Weston Turville, Marroway, Weston Turville, Weston Turville Turn, Stoke Church Lane, Weston -

Aylesbury Vale Parish Notice of Uncontested Election
NOTICE OF UNCONTESTED ELECTION Buckinghamshire Council (Aylesbury Vale Area) Election of Parish Councillors for Adstock on 6 May 2021 I Nick Graham, being the Returning Officer at the above election, report that the persons whose names appear below were duly elected Parish Councillors for Adstock. Name of Candidate Home Address Description (if any) CORNISH (address in Buckinghamshire) Chris FRASER-SMITH (address in Buckinghamshire) Neil James MURPHY (address in Buckinghamshire) Marianne Eleanor RANDALL (address in Buckinghamshire) Douglas James SALVER (address in Buckinghamshire) Paul Ralph STONE (address in Buckinghamshire) Jon WALKER (address in Buckinghamshire) Simon John Dated Friday 9 April 2021 Nick Graham Returning Officer Printed and published by the Returning Officer, The Gateway, Gatehouse Road, Aylesbury, HP19 8FF NOTICE OF UNCONTESTED ELECTION Buckinghamshire Council (Aylesbury Vale Area) Election of Parish Councillors for Akeley on 6 May 2021 I Nick Graham, being the Returning Officer at the above election, report that the persons whose names appear below were duly elected Parish Councillors for Akeley. Name of Candidate Home Address Description (if any) CLARKE The Old School, The Square, Chris Richard Akeley, Buckingham, MK18 5HP COXALL Inleys, 1 Church Hill, Akeley, Debs Buckingham, MK18 5HA GEORGE Honeysuckle Cottage, Chapel Cara Isabelle Louise Lane, Akeley, Bucks, MK18 5HU GOODGER 29 Manor Road, Akeley, Paul Leslie George Buckingham, MK18 5HQ HOCKLEY The Cottage, Main Street, Akeley, John Edward Bucks, MK18 5HR HOLLAND