The RUNX1 Database
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Functions of the Mineralocorticoid Receptor in the Hippocampus By
Functions of the Mineralocorticoid Receptor in the Hippocampus by Aaron M. Rozeboom A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Cellular and Molecular Biology) in The University of Michigan 2008 Doctoral Committee: Professor Audrey F. Seasholtz, Chair Professor Elizabeth A. Young Professor Ronald Jay Koenig Associate Professor Gary D. Hammer Assistant Professor Jorge A. Iniguez-Lluhi Acknowledgements There are more people than I can possibly name here that I need to thank who have helped me throughout the process of writing this thesis. The first and foremost person on this list is my mentor, Audrey Seasholtz. Between working in her laboratory as a research assistant and continuing my training as a graduate student, I spent 9 years in Audrey’s laboratory and it would be no exaggeration to say that almost everything I have learned regarding scientific research has come from her. Audrey’s boundless enthusiasm, great patience, and eager desire to teach students has made my time in her laboratory a richly rewarding experience. I cannot speak of Audrey’s laboratory without also including all the past and present members, many of whom were/are not just lab-mates but also good friends. I also need to thank all the members of my committee, an amazing group of people whose scientific prowess combined with their open-mindedness allowed me to explore a wide variety of interests while maintaining intense scientific rigor. Outside of Audrey’s laboratory, there have been many people in Ann Arbor without whom I would most assuredly have gone crazy. -

And EZH2-Regulated Gene, Has Differential Roles in AR-Dependent and -Independent Prostate Cancer
www.impactjournals.com/oncotarget/ Oncotarget, Vol. 6, No.4 RUNX1, an androgen- and EZH2-regulated gene, has differential roles in AR-dependent and -independent prostate cancer Ken-ichi Takayama1,2, Takashi Suzuki3, Shuichi Tsutsumi4, Tetsuya Fujimura5, Tomohiko Urano1,2, Satoru Takahashi6, Yukio Homma5, Hiroyuki Aburatani4 and Satoshi Inoue1,2,7 1 Department of Anti-Aging Medicine, The University of Tokyo, Bunkyo-ku, Tokyo, Japan 2 Department of Geriatric Medicine, The University of Tokyo, Bunkyo-ku, Tokyo, Japan 3 Department of Pathology, Tohoku University Graduate School of Medicine, Sendai, Miyagi, Japan 4 Genome Science Division, Research Center for Advanced Science and Technology (RCAST), The University of Tokyo, Meguro-ku, Tokyo, Japan 5 Department of Urology, Graduate School of Medicine, The University of Tokyo, Bunkyo-ku, Tokyo, Japan 6 Department of Urology, Nihon University School of Medicine, Itabashi-ku, Tokyo, Japan 7 Division of Gene Regulation and Signal Transduction, Research Center for Genomic Medicine, Saitama Medical University, Hidaka, Saitama, Japan Correspondence to: Satoshi Inoue, email: [email protected] Keywords: RUNX1, androgen receptor, EZH2, prostate cancer Received: October 02, 2014 Accepted: December 09, 2014 Published: December 10, 2014 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. ABSTRACT Androgen receptor (AR) signaling is essential for the development of prostate cancer. Here, we report that runt-related transcription factor (RUNX1) could be a key molecule for the androgen-dependence of prostate cancer. We found RUNX1 is a target of AR and regulated positively by androgen. -

Mutational Landscape and Clinical Outcome of Patients with De Novo Acute Myeloid Leukemia and Rearrangements Involving 11Q23/KMT2A
Mutational landscape and clinical outcome of patients with de novo acute myeloid leukemia and rearrangements involving 11q23/KMT2A Marius Billa,1,2, Krzysztof Mrózeka,1,2, Jessica Kohlschmidta,b, Ann-Kathrin Eisfelda,c, Christopher J. Walkera, Deedra Nicoleta,b, Dimitrios Papaioannoua, James S. Blachlya,c, Shelley Orwicka,c, Andrew J. Carrolld, Jonathan E. Kolitze, Bayard L. Powellf, Richard M. Stoneg, Albert de la Chapelleh,i,2, John C. Byrda,c, and Clara D. Bloomfielda,c aThe Ohio State University Comprehensive Cancer Center, Columbus, OH 43210; bAlliance for Clinical Trials in Oncology Statistics and Data Center, The Ohio State University Comprehensive Cancer Center, Columbus, OH 43210; cDivision of Hematology, Department of Internal Medicine, The Ohio State University Comprehensive Cancer Center, Columbus, OH 43210; dDepartment of Genetics, University of Alabama at Birmingham, Birmingham, AL 35294; eNorthwell Health Cancer Institute, Zucker School of Medicine at Hofstra/Northwell, Lake Success, NY 11042; fDepartment of Internal Medicine, Section on Hematology & Oncology, Wake Forest Baptist Comprehensive Cancer Center, Winston-Salem, NC 27157; gDepartment of Medical Oncology, Dana-Farber/Partners Cancer Care, Boston, MA 02215; hHuman Cancer Genetics Program, Comprehensive Cancer Center, The Ohio State University, Columbus, OH 43210; and iDepartment of Cancer Biology and Genetics, Comprehensive Cancer Center, The Ohio State University, Columbus, OH 43210 Contributed by Albert de la Chapelle, August 28, 2020 (sent for review July 17, 2020; reviewed by Anne Hagemeijer and Stefan Klaus Bohlander) Balanced rearrangements involving the KMT2A gene, located at patterns that include high expression of HOXA genes and thereby 11q23, are among the most frequent chromosome aberrations in contribute to leukemogenesis (14–16). -

Figure S17 Figure S16
immune responseregulatingcellsurfacereceptorsignalingpathway ventricular cardiacmuscletissuedevelopment t cellactivationinvolvedinimmuneresponse intrinsic apoptoticsignalingpathway single organismalcelladhesion cholesterol biosyntheticprocess myeloid leukocytedifferentiation determination ofadultlifespan response tointerferongamma muscle organmorphogenesis endothelial celldifferentiation brown fatcelldifferentiation mitochondrion organization myoblast differentiation response toprotozoan amino acidtransport leukocyte migration cytokine production t celldifferentiation protein secretion response tovirus angiogenesis Scrt1 Tcf25 Dpf1 Sap30 Ing2 Zfp654 Sp9 Zfp263 Mxi1 Hes6 Zfp395 Rlf Ppp1r13l Snapc1 C030039L03Rik Hif1a Arrb1 Glis3 Rcor2 Hif3a Fbxo21 Dnajc21 Rest Sirt6 Foxj1 Kdm5b Ankzf1 Sos2 Plscr1 Jdp2 Rbbp8 Etv4 Msh5 Mafg Tsc22d3 Nupr1 Ddit3 Cebpg Zfp790 Atf5 Cebpb Atf3 Trim21 Irf9 Irf2 Tbx21 Stat2 Stat1 Zbp1 Irf1 aGOslimPos Ikzf3 Oasl1 Irf7 Trim30a Dhx58 Txk Rorc Rora Nr1d2 Setdb2 Vdr Vax2 Nr1d1 Foxs1 Eno1 Thap3 Nfkbil1 Edf1 Srebf1 Lbr Tead1 Zfp608 Pcx Ift57 Ssbp4 Stat3 Mxd1 Pml Ssh2 Chd7 Maf Cic Bcl3 Prkdc Mbd5 Ppfibp2 Foxp2 Tal2 Mlf1 Bcl6b Zfp827 Ikzf2 Phtf2 Bmyc Plagl2 Nfkb2 Nfkb1 Tox Nrip1 Utf1 Klf3 Plagl1 Nfkbib Spib Nfkbie Akna Rbpj Ncoa3 Id1 Tnp2 Gata3 Gata1 Pparg Id2 Epas1 Zfp280b Commons Pathway Erg GO MSigDB KEGG Hhex WikiPathways SetGene Databases Batf Aff3 Zfp266 gene modules other (hypergeometric TF, from Figure Trim24 Zbtb5 Foxo3 Aebp2 XPodNet -protein-proteininteractionsinthepodocyteexpandedbySTRING Ppp1r10 Dffb Trp53 Enrichment -

Inhibition of HIF1` Signaling: a Grand Slam for MDS Therapy?
VIEWS IN THE SPOTLIGHT Inhibition of HIF1` Signaling: A Grand Slam for MDS Therapy? Jiahao Chen and Ulrich Steidl Summary: The recent focus on genomics in myelodysplastic syndromes (MDS) has led to important insights and revealed a daunting genetic heterogeneity, which is presenting great challenges for clinical treatment and preci- sion oncology approaches in MDS. Hayashi and colleagues show that multiple mutations frequently found in MDS activate HIF1α signaling, which they also found to be suffi cient to induce overt MDS in mice. Furthermore, both genetic and pharmacologic inhibition of HIF1α suppressed MDS development with only mild effects on normal hematopoiesis, implicating HIF1α signaling as a promising therapeutic target to tackle the heterogeneity of MDS. Cancer Discov; 8(11); 1355–7. ©2018 AACR . See related article by Hayashi et al., p. 1438 (5). Myelodysplastic syndromes (MDS) are a heterogeneous In this issue, Hayashi and colleagues found that target group of hematologic disorders characterized by ineffi cient genes activated by HIF1α signaling were highly expressed in hematopoiesis that manifests as bone marrow (BM) dysplasia a published cohort of 183 patients with MDS compared with and peripheral blood cytopenias, and increased risk of leuke- healthy controls ( 5 ). IHC confi rmed an increased frequency mic transformation ( 1 ). The median survival of patients with of HIF1α-expressing cells in MDS samples at different stages MDS is 4.5 years, with a signifi cantly worse survival of< 1 year (low-, intermediate-, and high-risk) -
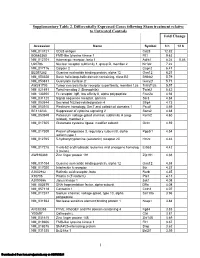
Supplementary Table 2
Supplementary Table 2. Differentially Expressed Genes following Sham treatment relative to Untreated Controls Fold Change Accession Name Symbol 3 h 12 h NM_013121 CD28 antigen Cd28 12.82 BG665360 FMS-like tyrosine kinase 1 Flt1 9.63 NM_012701 Adrenergic receptor, beta 1 Adrb1 8.24 0.46 U20796 Nuclear receptor subfamily 1, group D, member 2 Nr1d2 7.22 NM_017116 Calpain 2 Capn2 6.41 BE097282 Guanine nucleotide binding protein, alpha 12 Gna12 6.21 NM_053328 Basic helix-loop-helix domain containing, class B2 Bhlhb2 5.79 NM_053831 Guanylate cyclase 2f Gucy2f 5.71 AW251703 Tumor necrosis factor receptor superfamily, member 12a Tnfrsf12a 5.57 NM_021691 Twist homolog 2 (Drosophila) Twist2 5.42 NM_133550 Fc receptor, IgE, low affinity II, alpha polypeptide Fcer2a 4.93 NM_031120 Signal sequence receptor, gamma Ssr3 4.84 NM_053544 Secreted frizzled-related protein 4 Sfrp4 4.73 NM_053910 Pleckstrin homology, Sec7 and coiled/coil domains 1 Pscd1 4.69 BE113233 Suppressor of cytokine signaling 2 Socs2 4.68 NM_053949 Potassium voltage-gated channel, subfamily H (eag- Kcnh2 4.60 related), member 2 NM_017305 Glutamate cysteine ligase, modifier subunit Gclm 4.59 NM_017309 Protein phospatase 3, regulatory subunit B, alpha Ppp3r1 4.54 isoform,type 1 NM_012765 5-hydroxytryptamine (serotonin) receptor 2C Htr2c 4.46 NM_017218 V-erb-b2 erythroblastic leukemia viral oncogene homolog Erbb3 4.42 3 (avian) AW918369 Zinc finger protein 191 Zfp191 4.38 NM_031034 Guanine nucleotide binding protein, alpha 12 Gna12 4.38 NM_017020 Interleukin 6 receptor Il6r 4.37 AJ002942 -

RUNX1 Together with a Compendium of Hematopoietic Regulators, Chromatin Modifiers and Basal Transcr
Leukemia (2014) 28, 770–778 OPEN & 2014 Macmillan Publishers Limited All rights reserved 0887-6924/14 www.nature.com/leu ORIGINAL ARTICLE CBFB–MYH11/RUNX1 together with a compendium of hematopoietic regulators, chromatin modifiers and basal transcription factors occupies self-renewal genes in inv(16) acute myeloid leukemia A Mandoli1, AA Singh1, PWTC Jansen2, ATJ Wierenga3,4, H Riahi1, G Franci5, K Prange1, S Saeed1, E Vellenga3, M Vermeulen2, HG Stunnenberg1 and JHA Martens1 Different mechanisms for CBFb–MYH11 function in acute myeloid leukemia with inv(16) have been proposed such as tethering of RUNX1 outside the nucleus, interference with transcription factor complex assembly and recruitment of histone deacetylases, all resulting in transcriptional repression of RUNX1 target genes. Here, through genome-wide CBFb–MYH11-binding site analysis and quantitative interaction proteomics, we found that CBFb–MYH11 localizes to RUNX1 occupied promoters, where it interacts with TAL1, FLI1 and TBP-associated factors (TAFs) in the context of the hematopoietic transcription factors ERG, GATA2 and PU.1/SPI1 and the coregulators EP300 and HDAC1. Transcriptional analysis revealed that upon fusion protein knockdown, a small subset of the CBFb–MYH11 target genes show increased expression, confirming a role in transcriptional repression. However, the majority of CBFb–MYH11 target genes, including genes implicated in hematopoietic stem cell self-renewal such as ID1, LMO1 and JAG1, are actively transcribed and repressed upon fusion protein knockdown. Together these results suggest an essential role for CBFb–MYH11 in regulating the expression of genes involved in maintaining a stem cell phenotype. Leukemia (2014) 28, 770–778; doi:10.1038/leu.2013.257 Keywords: CBFb–MYH11; RUNX1; histone acetylation; acute myeloid leukemia; inv(16) INTRODUCTION Heterozygous Cbfb-Myh11 knock-in mice are embryonic lethal, Core-binding transcription factors (CBFs) have roles in stem cell with definitive hematopoiesis blocked at the stem-cell level. -

A KMT2A-AFF1 Gene Regulatory Network Highlights the Role of Core Transcription Factors and Reveals the Regulatory Logic of Key Downstream Target Genes
Downloaded from genome.cshlp.org on October 7, 2021 - Published by Cold Spring Harbor Laboratory Press Research A KMT2A-AFF1 gene regulatory network highlights the role of core transcription factors and reveals the regulatory logic of key downstream target genes Joe R. Harman,1,7 Ross Thorne,1,7 Max Jamilly,2 Marta Tapia,1,8 Nicholas T. Crump,1 Siobhan Rice,1,3 Ryan Beveridge,1,4 Edward Morrissey,5 Marella F.T.R. de Bruijn,1 Irene Roberts,3,6 Anindita Roy,3,6 Tudor A. Fulga,2,9 and Thomas A. Milne1,6 1MRC Molecular Haematology Unit, MRC Weatherall Institute of Molecular Medicine, Radcliffe Department of Medicine, University of Oxford, Oxford, OX3 9DS, United Kingdom; 2MRC Weatherall Institute of Molecular Medicine, Radcliffe Department of Medicine, University of Oxford, Oxford, OX3 9DS, United Kingdom; 3MRC Molecular Haematology Unit, MRC Weatherall Institute of Molecular Medicine, Department of Paediatrics, University of Oxford, Oxford, OX3 9DS, United Kingdom; 4Virus Screening Facility, MRC Weatherall Institute of Molecular Medicine, John Radcliffe Hospital, University of Oxford, Oxford, OX3 9DS, United Kingdom; 5Center for Computational Biology, Weatherall Institute of Molecular Medicine, University of Oxford, John Radcliffe Hospital, Oxford OX3 9DS, United Kingdom; 6NIHR Oxford Biomedical Research Centre Haematology Theme, University of Oxford, Oxford, OX3 9DS, United Kingdom Regulatory interactions mediated by transcription factors (TFs) make up complex networks that control cellular behavior. Fully understanding these gene regulatory networks (GRNs) offers greater insight into the consequences of disease-causing perturbations than can be achieved by studying single TF binding events in isolation. Chromosomal translocations of the lysine methyltransferase 2A (KMT2A) gene produce KMT2A fusion proteins such as KMT2A-AFF1 (previously MLL-AF4), caus- ing poor prognosis acute lymphoblastic leukemias (ALLs) that sometimes relapse as acute myeloid leukemias (AMLs). -

Mechanistic Insights Into the Effect of RUNX1/ETO Knockdown in T(8;21) AML
Mechanistic insights into the effect of RUNX1/ETO knockdown in t(8;21) AML Anna Pickin A thesis submitted to the University of Birmingham for the degree of DOCTOR OF PHILOSOPHY Institute of Biomedical Research Birmingham Centre for Genomic Biology College of Medical and Dental Sciences University of Birmingham September 2016 1 University of Birmingham Research Archive e-theses repository This unpublished thesis/dissertation is copyright of the author and/or third parties. The intellectual property rights of the author or third parties in respect of this work are as defined by The Copyright Designs and Patents Act 1988 or as modified by any successor legislation. Any use made of information contained in this thesis/dissertation must be in accordance with that legislation and must be properly acknowledged. Further distribution or reproduction in any format is prohibited without the permission of the copyright holder. ABSTRACT The mutation of transcription factor genes is a main cause for acute myeloid leukaemia. RUNX1/ETO, the product of the t(8;21) chromosomal translocation, subverts normal blood cell development by impairing myeloid differentiation. RUNX1/ETO knockdown alleviates this block, with a global reprogramming of transcription factor binding and initiation of myeloid differentiation. Co-depletion of the myeloid transcription factor C/EBPα with RUNX1/ETO suppressed this differentiation response. Furthermore, C/EBPα overexpression largely phenocopied the effect of RUNX1/ETO knockdown. Our data show that low levels of C/EBPα are critical to the maintenance of t(8;21) AML and that C/EBPα drives the response to RUNX1/ETO depletion. To examine how changes in transcription factor binding impact on the activity of cis- regulatory elements we mapped genome wide promoter-distal-element interactions in a t(8;21) AML cell line, via Capture HiC, and found that hundreds of interactions were altered by RUNX1/ETO knockdown. -

Progesterone Receptor-A Isoform Interaction with RUNX Transcription Factors Controls
bioRxiv preprint doi: https://doi.org/10.1101/2021.06.17.448908; this version posted June 20, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 1 Progesterone receptor-A isoform interaction with RUNX transcription factors controls 2 chromatin remodelling at promoters during ovulation 3 Authors: Dinh DT 1 (*), Breen J 2, Nicol B 3, Smith KM 1, Nicholls M 1, Emery A 1, 4 Wong YY 1, Barry SC 1, Yao HHC 3, Robker RL 1, Russell DL 1 (*) 5 Affiliations: 6 1. Robinson Research Institute, Adelaide Medical School, University of Adelaide, Australia 7 2. South Australian Genomics Centre (SAGC), South Australian Health and Medical 8 Research Institute (SAHMRI), Adelaide, South Australia, Australia 9 3. Reproductive Developmental Biology Group, National Institute of Environmental Health 10 Sciences, Research Triangle Park, NC 27709, USA 11 12 Summary: 13 Progesterone receptor (PGR) plays diverse roles in reproductive tissues and thus coordinates 14 mammalian fertility. In the ovary, acutely induced PGR is the key determinant of ovulation 15 through transcriptional control of a unique set of genes that culminates in follicle rupture. 16 However, the molecular mechanisms for PGR’s specialised function in ovulation is poorly 17 understood. To address this, we assembled a detailed genomic profile of PGR action through 18 combined ATAC-seq, RNA-seq and ChIP-seq analysis in wildtype and isoform-specific PGR 19 null mice. -

Stage-Specific Action of Runx1 and GATA3 Controls Silencing of PU.1 Expression in Mouse Pro–Tcells
ARTICLE Stage-specific action of Runx1 and GATA3 controls silencing of PU.1 expression in mouse pro–Tcells Hiroyuki Hosokawa1,2,3,MariaKoizumi1, Kaori Masuhara1, Maile Romero-Wolf3,TomoakiTanaka4, Toshinori Nakayama5,and Ellen V. Rothenberg3 Downloaded from http://rupress.org/jem/article-pdf/218/8/e20202648/1418720/jem_20202648.pdf by California Institute Of Technology user on 28 June 2021 PU.1 (encoded by Spi1), an ETS-family transcription factor with many hematopoietic roles, is highly expressed in the earliest intrathymic T cell progenitors but must be down-regulated during T lineage commitment. The transcription factors Runx1 and GATA3 have been implicated in this Spi1 repression, but the basis of the timing was unknown. We show that increasing Runx1 and/or GATA3 down-regulates Spi1 expression in pro–T cells, while deletion of these factors after Spi1 down-regulation reactivates its expression. Leveraging the stage specificities of repression and transcription factor binding revealed an unconventional but functional site in Spi1 intron 2. Acute Cas9-mediated deletion or disruption of the Runx and GATA motifs in this element reactivates silenced Spi1 expression in a pro–T cell line, substantially more than disruption of other candidate elements, and counteracts the repression of Spi1 in primary pro–T cells during commitment. Thus, Runx1 and GATA3 work stage specifically through an intronic silencing element in mouse Spi1 to control strength and maintenance of Spi1 repression during T lineage commitment. Introduction PU.1, encoded by Spi1, is an E twenty-six (ETS)–family tran- T cells develop from multipotent precursors in the thymus, scription factor with multiple roles in the development and where microenvironmental Notch signaling educates progeni- function of myeloid and lymphoid hematopoietic lineages tors to become T cells (Hosokawa and Rothenberg, 2021; Radtke (Carotta et al., 2010; Rothenberg et al., 2019; Singh et al., 1999). -

Maintenance of Mammary Epithelial Phenotype by Transcription Factor Runx1 Through Mitotic Gene Bookmarking Joshua Rose University of Vermont
University of Vermont ScholarWorks @ UVM Graduate College Dissertations and Theses Dissertations and Theses 2019 Maintenance Of Mammary Epithelial Phenotype By Transcription Factor Runx1 Through Mitotic Gene Bookmarking Joshua Rose University of Vermont Follow this and additional works at: https://scholarworks.uvm.edu/graddis Part of the Biochemistry Commons, and the Genetics and Genomics Commons Recommended Citation Rose, Joshua, "Maintenance Of Mammary Epithelial Phenotype By Transcription Factor Runx1 Through Mitotic Gene Bookmarking" (2019). Graduate College Dissertations and Theses. 998. https://scholarworks.uvm.edu/graddis/998 This Thesis is brought to you for free and open access by the Dissertations and Theses at ScholarWorks @ UVM. It has been accepted for inclusion in Graduate College Dissertations and Theses by an authorized administrator of ScholarWorks @ UVM. For more information, please contact [email protected]. MAINTENANCE OF MAMMARY EPITHELIAL PHENOTYPE BY TRANSCRIPTION FACTOR RUNX1 THROUGH MITOTIC GENE BOOKMARKING A Thesis Presented by Joshua Rose to The Faculty of the Graduate College of The University of Vermont In Partial Fulfillment of the Requirements for the Degree of Master of Science Specializing in Cellular, Molecular, and Biomedical Sciences January, 2019 Defense Date: November 12, 2018 Thesis Examination Committee: Sayyed Kaleem Zaidi, Ph.D., Advisor Gary Stein, Ph.D., Advisor Seth Frietze, Ph.D., Chairperson Janet Stein, Ph.D. Jonathan Gordon, Ph.D. Cynthia J. Forehand, Ph.D. Dean of the Graduate College ABSTRACT Breast cancer arises from a series of acquired mutations that disrupt normal mammary epithelial homeostasis and create multi-potent cancer stem cells that can differentiate into clinically distinct breast cancer subtypes. Despite improved therapies and advances in early detection, breast cancer remains the leading diagnosed cancer in women.