Lightburn Hospital
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
GLASGOW WEST END U3A January 2021 Newsletter
GLASGOW WEST END U3A January 2021 Newsletter Dear All Happy New Year to you all. 2021 has got off to a shaky start but hopefully it will improve. We just want a vaccine… The weather has been lovely though a bit treacherous underfoot in places. The hospital grounds at Gartnavel Royal have been well-gritted and are ideal for a sunny winter walk. Bingham’s Pond provided much entertainment for children when most of it was frozen. Bit too much excitement for me, I prefer to be on firmer ground. GWEU3A continues to be busy on Zoom/Facebook/WhatsApp. We had a lovely Christmas Event by Fool’s Gold in December which all enjoyed. The David Hume Institute Focus Group on what we found important to happiness during lockdown, leading on to Equality and Fairness, proved very popular and stimulating. A number of you walked for Shelter with a pal in December which was worthwhile exercise. Coffee and Chat continues to be popular and a good way to meet members. The small groups are continuing very well with a new French group starting up. Edith Fleming is getting musicians together to play and listen to classical music. If you wish to join them please indicate through the website in the usual way. After the Focus Group a number of people expressed an interest in being part of a Current Affairs Group. This would require members to be unbiased politically, and would require a structure and format a bit like the Focus group. If you are interested in further discussion about such a group please email me at [email protected] and I will try to facilitate it. -
Total Sickness Benefit Data – Figures 1-9 Updated from Glasgow Profile
Scottish Observatory for Work and Health University of Glasgow Health-related Worklessness in Scotland Profile June 2011 Judith Brown Joel Smith David Webster James Arnott Ivan Turok Ewan Macdonald Richard Mitchell Contact: Judith Brown Public Health & Health Policy 1 Lilybank Gardens University of Glasgow Glasgow G12 8RZ [email protected] 1 Summary & Key Findings Health-related worklessness in Scotland Profile 1. This profile provides detailed information on total sickness-related benefit claimants (incapacity benefit, IB and Employment Support Allowance, ESA claimants) from 2000 to 2009, ESA claimants from 2009 and ESA claimants by medical condition for 2010 (broken down by age, duration of claim, stage of claim and ethnicity). 2. The profile contains data for Scotland, Glasgow City, North Lanarkshire, South Lanarkshire, East Dunbartonshire, East Renfrewshire, Inverclyde, Renfrewshire, West Dunbartonshire. 3. The percent of the working age population (WAP) claiming IB in Glasgow City decreased from 18.8% in 2000 to 14.4% by 2007. Following the introduction of ESA in October 2008, the WAP in receipt of total sickness-related benefit has continued to follow the general linear decline observed for IB but the rate is not falling as steeply. By 2009, 13.5% of the WAP in Glasgow were claiming sickness benefit compared to 9.1% in Scotland. Similar trends are observed in the other geographies. 4. The rate of on flow decreased in Scotland and Glasgow City prior to the introduction of ESA. From 2008 there have been small increases in IB/ESA on flow rates. By 2009, total sickness benefit was in excess of the level observed for 2005 with the rate of on flow currently at 3.9% in Glasgow. -

Ebook Download Bishopbriggs 1910 : Lanarkshire Sheet 1.15 Ebook, Epub
BISHOPBRIGGS 1910 : LANARKSHIRE SHEET 1.15 PDF, EPUB, EBOOK Gilbert Torrance Bell | none | 01 Feb 1998 | Alan Godfrey Maps | 9780850549546 | English | Co Durham, United Kingdom Bishopbriggs 1910 : Lanarkshire Sheet 1.15 PDF Book Neil Storey. United Kingdom and many other countries See details. You can scroll down to find more maps of this location. Seller Image. Condition Used - Very Good. If your order is a non-stock item, the delivery timescale on that item will show as working days on the product details. Published by Robinson Glass silverer preparing mirrors. Calum's Road. More information about this seller Contact this seller 1. View basket. The Suspicions of Mr. The map links up sheet 30 Calton Hill to the east and 35 Edinburgh Castle to the south. It shows in great detail houses, railway tracks, churches, mills, signposts, cranes, pathways, etc and includes historical notes of the area. The reason for having such a seal made is unknown, but it is possible that John Geddes, manager of the works in , may have bought a consignment of claret for bottling HA 1. Stock photo. Lanarkshire Sheet I. Item location:. Learn More - opens in a new window or tab Any international postage is paid in part to Pitney Bowes Inc. Trusted seller, fast delivery and easy returns. Looking for an Agent? Remember me? Published by Arcturus Publishing Ltd. Seller Inventory x Cycling Map Folding Maps. The encryption keys are held on state-of-the-art, tamper proof systems in the same family as those used to secure VeriSign's Global Root certificate, making them all but impossible to extract. -
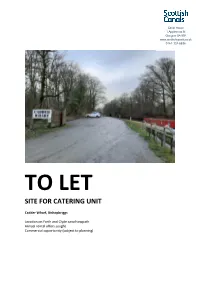
Cadder Wharf, Bishopbriggs
Canal House 1 Applecross St Glasgow G4 9SP www.scottishcanals.co.uk 0141-332-6936 TO LET SITE FOR CATERING UNIT Cadder Wharf, Bishopbriggs Location on Forth and Clyde canal towpath Annual rental offers sought Commercial opportunity (subject to planning) Location Cadder Wharf is located just off the A803, Kirkintilloch Road, in Cadder, near to the picturesque Cadder Parish Church. The Forth and Clyde Canal is a popular route for walkers and cyclists, and Scottish Canals offers six moorings at this location. Set in a beautiful, wooded location between Lambhill and Kirkintilloch, Cadder is a hamlet in the district of the town of Bishopbriggs, 7km north of Glasgow City Centre. Cadder was the site of a Roman Fort on the route of the Antonine Wall. To the north, remains of the wall and associated Roman Fort can be found. Description The exact location of the catering unit at Cadder Wharf will be subject to negotiation and agreement with Scottish Canals, depending on the size of the unit proposed. There will also be the potential to link in to the existing electricity and water supplies, subject to agreement with Scottish Canals and relevant utility providers. Use Interested parties should contact the local planning office for advice and information on suitable uses. The planning office at East Dunbartonshire Council can be contacted on 0300 123 4510 or [email protected]. Scheduled Monument Consent may be required for the siting of a catering unit at this location. For further advice and information, please contact Historic Environment Scotland on 0131 668 8716 or [email protected]. -

0/2, 59 Raeberry Street, North Kelvinside, Glasgow, G20 6EQ.Indd
0/2, 59 Raeberry Street NORTH KELVINSIDE, GLASGOW, G20 6EQ 0141 404 5474 0/2, 59 Raeberry Street North Kelvinside, Glasgow, G20 6EQ Situated in North Kelvinside, this fl at is in a upgraded electrics and lighting) throughout highly desirable West End location and is with a fresh, contemporary theme. The just a short distance from a fi ne selection of apartment has been successfully and cleverly amenities on Great Western Road and Byres designed to off er contemporary living, within Road, together with the wonderful, nearby this popular development. Off ering bright Botanic Gardens. The property is also close living space, the easily-kept accommodation to Kelvinbridge underground and Glasgow extends to a welcoming entrance hall with University. There are good road links to the a storage recess. Immediately impressive nearby Clyde Tunnel, Clydeside Expressway ‘dual-aspect’ lounge/bedroom area. This and M8 motorway network. zone is open-plan to a well equipped and newly fi tted kitchen, with a good range This beautifully appointed, ground fl oor, of fl oor and wall mounted units and a studio apartment is located within the complementary worktop. It further benefi ts desirable West End of Glasgow, which has from an integrated oven, hob, extractor hood, excellent amenities on its doorstep. The washing machine and fridge/freezer. property off ers fl exible accommodation and its attractive position makes it an ideal choice There is a small dressing room/study area off for a young professional, working in the city the lounge. This allows access (via a sliding or commuting further afi eld. -

Twentyci Property & Homemover Report
TwentyCi Property & Homemover Report – Q3 2017 Information embargoed until Wednesday 4th October 2017 at 00:01 Welcome to the latest TwentyCi Property & Homemover Report, a quarterly review of the UK property market. As a life event data company, TwentyCi has exclusive access to more than 29 billion qualified data points across the whole of the property sector – for both property purchases and rental. In addition to tracking sales momentum, this ‘state of the nation’ report provides unique insight into the people behind the numbers, creating a picture of the demographic, regional and socio-economic factors impacting the housing market. With a 99.6% view of both the property sales and rental markets, the TwentyCi Property & Homemover Report is the most comprehensive factual source of home moving data available. Key take-outs for Q3 2017 • Overall the volatile market is starting to stabilise with exchanges up 15.2% year-on-year and house prices increasing by 1.5% for the year. However London experiences lower growth in exchanges than the rest of the UK at 9% year-on-year, and prices drop by 8.4% in the Capital – one of the key reasons behind the overall fall in price for the market. • While the majority of market activity is for properties under £250k and with sub £50k household incomes, the biggest growth in transactions this quarter has been among buyers in higher income bands purchasing higher value properties. • Online-only estate agents’ market share increases by 19% this quarter. All data is based on Q3 2017 versus Q3 2016 year-on-year comparisons unless otherwise stated. -

Guest Room Leaflet
Guest room locations Locations: Bield, Hanover (Scotland) & Trust Please find a list of the locations where guest bedrooms are available. For booking, and for specific details of the accommodation and facilities provided at each location, please contact the individual development. Telephone Council Area Development number Landlord Aberdeen Aberdeen - Ashley Grove, Great Western Road, AB10 6WE 01224 575 159 Hanover Aberdeen - Bridge of Dee Court, Holburn Street, AB10 7HG 01224 572 741 Hanover Aberdeen - Rosewell Gardens, AB15 6HZ 01224 324 089 Hanover Aberdeen - Strachan Mill Court, Leadside Road, AB25 1TX 01224 647 515 Hanover Aberdeenshire Banchory - Hanover Court, Station Road, AB31 5ZA 01330 822 921 Hanover Banff - Airlie Gardens, Low Street, AB45 1AZ 01261 815 796 Hanover Banff - Doo'cot View, St Combs Court, AB45 1GD 01261 815 946 Hanover Huntly - Granary Street, AB54 8AR 01466 793 728 Hanover Inverbervie - Hanover Court, DD10 0TR 01561 361 188 Hanover Inverurie - Hanover Court, Cuninghill Road, AB51 3WD 01467 624 179 Hanover Lumsden - Hanover Court, Main Street, AB54 4JF 01464 861 796 Hanover Macduff - Doune Court, Church Street, AB44 1UR 01261 832 906 Hanover Peterhead - Strawberry Bank, Eden Drive, AB42 2AA 01779 479 918 Hanover Stonehaven - Hanover Court, David Street, AB39 2FD 01569 764 595 Hanover Stonehaven - Turners Court, Ironfield Lane, AB39 2AE 01569 765 595 Hanover Tarves - Hanover Court, New Road, AB41 7LG 01651 851 559 Hanover Angus Brechin - South Port, Union Street, DD9 6HS 01356 624247 Bield Forfar - Kirkriggs Court, -

National Retailers.Xlsx
THE NATIONAL / SUNDAY NATIONAL RETAILERS Store Name Address Line 1 Address Line 2 Address Line 3 Post Code M&S ABERDEEN E51 2-28 ST. NICHOLAS STREET ABERDEEN AB10 1BU WHS ST NICHOLAS E48 UNIT E5, ST. NICHOLAS CENTRE ABERDEEN AB10 1HW SAINSBURYS E55 UNIT 1 ST NICHOLAS CEN SHOPPING CENTRE ABERDEEN AB10 1HW RSMCCOLL130UNIONE53 130 UNION STREET ABERDEEN, GRAMPIAN AB10 1JJ COOP 204UNION E54 204 UNION STREET X ABERDEEN AB10 1QS SAINSBURY CONV E54 SOFA WORKSHOP 206 UNION STREET ABERDEEN AB10 1QS SAINSBURY ALF PL E54 492-494 UNION STREET ABERDEEN AB10 1TJ TESCO DYCE EXP E44 35 VICTORIA STREET ABERDEEN AB10 1UU TESCO HOLBURN ST E54 207 HOLBURN STREET ABERDEEN AB10 6BL THISTLE NEWS E54 32 HOLBURN STREET ABERDEEN AB10 6BT J&C LYNCH E54 66 BROOMHILL ROAD ABERDEEN AB10 6HT COOP GT WEST RD E46 485 GREAT WESTERN ROAD X ABERDEEN AB10 6NN TESCO GT WEST RD E46 571 GREAT WESTERN ROAD ABERDEEN AB10 6PA CJ LANG ST SWITIN E53 43 ST. SWITHIN STREET ABERDEEN AB10 6XL GARTHDEE STORE 19-25 RAMSAY CRESCENT GARTHDEE ABERDEEN AB10 7BL SAINSBURY PFS E55 GARTHDEE ROAD BRIDGE OF DEE ABERDEEN AB10 7QA ASDA BRIDGE OF DEE E55 GARTHDEE ROAD BRIDGE OF DEE ABERDEEN AB10 7QA SAINSBURY G/DEE E55 GARTHDEE ROAD BRIDGE OF DEE ABERDEEN AB10 7QA COSTCUTTER 37 UNION STREET ABERDEEN AB11 5BN RS MCCOLL 17UNION E53 17 UNION STREET ABERDEEN AB11 5BU ASDA ABERDEEN BEACH E55 UNIT 11 BEACH BOULEVARD RETAIL PARK LINKS ROAD, ABERDEEN AB11 5EJ M & S UNION SQUARE E51 UNION SQUARE 2&3 SOUTH TERRACE ABERDEEN AB11 5PF SUNNYS E55 36-40 MARKET STREET ABERDEEN AB11 5PL TESCO UNION ST E54 499-501 -

Open Space Strategy Consultative Draft
GLASGOW OPEN SPACE STRATEGY CONSULTATIVE DRAFT Prepared For: GLASGOW CITY COUNCIL Issue No 49365601 /05 49365601 /05 49365601 /05 Contents 1. Executive Summary 1 2. Glasgu: The Dear Green Place 11 3. What should open space be used for? 13 4. What is the current open space resource? 23 5. Place Setting for improved economic and community vitality 35 6. Health and wellbeing 59 7. Creating connections 73 8. Ecological Quality 83 9. Enhancing natural processes and generating resources 93 10. Micro‐Climate Control 119 11. Moving towards delivery 123 Strategic Environmental Assessment Interim Environment Report 131 Appendix 144 49365601 /05 49365601 /05 1. Executive Summary The City of Glasgow has a long tradition in the pursuit of a high quality built environment and public realm, continuing to the present day. This strategy represents the next steps in this tradition by setting out how open space should be planned, created, enhanced and managed in order to meet the priorities for Glasgow for the 21st century. This is not just an open space strategy. It is a cross‐cutting vision for delivering a high quality environment that supports economic vitality, improves the health of Glasgow’s residents, provides opportunities for low carbon movement, builds resilience to climate change, supports ecological networks and encourages community cohesion. This is because, when planned well, open space can provide multiple functions that deliver numerous social, economic and environmental benefits. Realising these benefits should be undertaken in a way that is tailored to the needs of the City. As such, this strategy examines the priorities Glasgow has set out and identifies six cross‐cutting strategic priority themes for how open space can contribute to meeting them. -
Fare4all? Report of the Enquiry Into Public Transport in Glasgow
Fare4All? Report of the Enquiry into Public Transport in Glasgow March 2006 Contents Fare4All? Steering Group 3 Fare4All? Key Findings 4 Fare4All? Suggestions for Improvements 5 1. Fare4All? 6 2. The Work of Fare4All? 7 3. Some Background to Bus Policy and Provision 8 Glasgow – A City Perspective Some Facts on the Communities who need to use Public Transport 4. Key Findings of the Fare4All? Survey 11 5. Perspectives of Older People 13 6. Perspectives of Parents with Children 14 7. Perspectives of People with Learning Disabilities 15 8. The Impact of Transport on Community Life: A Profile of North Glasgow 16 9. Fare4All? Transport Summit 18 10. Suggestions for Improvement 21 11. References 22 2 Fare4All? Steering Group The Fare4All? Steering Group is chaired by Paul Martin MSP. The members are: Allan Comrie Strathclyde Passenger Transport Executive Arlene Cooke North Glasgow Healthy Living Community Frank Creighton Healthy Castlemilk Irene Forrest North Area Transport Association John Halliday Strathclyde Passenger Transport Executive Fran Lundie Glasgow City Council Community Safety Department Agnes McGroarty West of Scotland Seniors’ Forum Niall McGrogan NHS Greater Glasgow Helen McNeil Glasgow Council for Voluntary Services Marie Montgomery Age Concern Jim Thompson Fair Deal Jess Thomson The Friends of the Victoria Kate Munro Community Engagement Manager, NHS Greater Glasgow Dan Harley Community Engagement Manager, NHS Greater Glasgow Mark McAllister Community Engagement Manager, NHS Greater Glasgow The content of this report reflects the views of the Fare4All? Steering Group or individual contributors and not necessarily those of any named organisation. This report is also available in large print and on-line. -

Cardowan Moss Is a Beezer Ae a Place
Scottish Scottish Lowlands Lowlands Easterhouse For more information please contact: A Beezer ae a Place Forestry Commission Scotland Cardowan Moss is a beezer ae a place. Cardowan Scottish Lowlands Forest District There’s bonnie flooers, lowpin puddocks Five Sisters House and swallows swallaein midgies. There’s Five Sisters Business Park even a china hingin aboot haufway doon Moss West Calder the path. Ye’ll no get much chat oot ae EH558PNCardowan Moss him though – the big yin’s made fae iron. Tel: 01555 660190 email:[email protected] Bishop Loch Todds Well Map 2 in a series of 5 Lochend Burn Map 2 in a series of 5 Callander Cardowan Moss STIRLINGSTIRLING R Teith Water Voles and Iron Men Dunblane R Forth WEST Alloa DUNBARTOONSHIRE Explore this network of Stirling A907 © Crown copyright and database right [2013]. well-managed trails around Ordnance Survey Licence number [100021242]. 9 A985 A875 EAST M876 M9 A811 DUNBARTONSHIRE 3 Cardowan Moss A809 8 7 A8 M80 2 1 Denny 1 and you’ll 8 6 Kilsyth 7 5 A891 4 3 find more 6 Falkirk A82 A803 M80 A801 than 5 FALKIRK West Maryston 31 Cumbernauld 4 A73 1 3 Mo Roghainn Carr Domhainn INVERCLYDE 30 beautiful M8 3 M73 A761 M8 2 2a 3 A89 3a Carr, no boglach, domhainn a bh’ ann uaireigin. 26 17 1/13 Easterhouse woodland. 15 10 4 29 25 19 M8 22 8/2 Airdrie 5 Ach an-diugh: sgaoilteachd chraobhan, flùraichean 1 A8 You might 2 3 4/1 6 Paisley 2 A7 4 ioma-dhathte, agus gille iarainn ’nan àrainn. -

Glasgow City Health and Social Care Partnership Health Contacts
Glasgow City Health and Social Care Partnership Health Contacts January 2017 Contents Glasgow City Community Health and Care Centre page 1 North East Locality 2 North West Locality 3 South Locality 4 Adult Protection 5 Child Protection 5 Emergency and Out-of-Hours care 5 Addictions 6 Asylum Seekers 9 Breast Screening 9 Breastfeeding 9 Carers 10 Children and Families 12 Continence Services 15 Dental and Oral Health 16 Dementia 18 Diabetes 19 Dietetics 20 Domestic Abuse 21 Employability 22 Equality 23 Health Improvement 23 Health Centres 25 Hospitals 29 Housing and Homelessness 33 Learning Disabilities 36 Maternity - Family Nurse Partnership 38 Mental Health 39 Psychotherapy 47 NHS Greater Glasgow and Clyde Psychological Trauma Service 47 Money Advice 49 Nursing 50 Older People 52 Occupational Therapy 52 Physiotherapy 53 Podiatry 54 Rehabilitation Services 54 Respiratory Team 55 Sexual Health 56 Rape and Sexual Assault 56 Stop Smoking 57 Volunteering 57 Young People 58 Public Partnership Forum 60 Comments and Complaints 61 Glasgow City Community Health & Care Partnership Glasgow Health and Social Care Partnership (GCHSCP), Commonwealth House, 32 Albion St, Glasgow G1 1LH. Tel: 0141 287 0499 The Management Team Chief Officer David Williams Chief Officer Finances and Resources Sharon Wearing Chief Officer Planning & Strategy & Chief Social Work Officer Susanne Miller Chief Officer Operations Alex MacKenzie Clincial Director Dr Richard Groden Nurse Director Mari Brannigan Lead Associate Medical Director (Mental Health Services) Dr Michael Smith