A Meta-Analysis of Monoamine Depletion St
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Preparing for Your 5-HIAA Urine Test
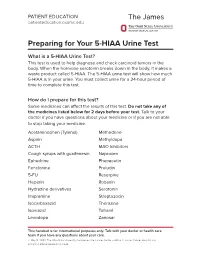
PATIENT EDUCATION patienteducation.osumc.edu Preparing for Your 5-HIAA Urine Test What is a 5-HIAA Urine Test? This test is used to help diagnose and check carcinoid tumors in the body. When the hormone serotonin breaks down in the body, it makes a waste product called 5-HIAA. The 5-HIAA urine test will show how much 5-HIAA is in your urine. You must collect urine for a 24-hour period of time to complete this test. How do I prepare for this test? Some medicines can affect the results of this test.Do not take any of the medicines listed below for 2 days before your test. Talk to your doctor if you have questions about your medicine or if you are not able to stop taking your medicine. Acetaminophen (Tylenol) Methedrine Aspirin Methyldopa ACTH MAO Inhibitors Cough syrups with guaifenesin Naproxen Ephedrine Phenacetin Fenclonine Preludin 5-FU Reserpine Heparin Robaxin Hydrazine derivatives Serotonin Imipramine Streptozocin Isocarboxazid Thorazine Isoniazid Tofranil Levodopa Zanosar This handout is for informational purposes only. Talk with your doctor or health care team if you have any questions about your care. © May 14, 2020. The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute. There are certain foods and drinks that you should not eat or drink before this test. Do not eat or drink any of the items below for 4 days before the test or during the test. Avocados Grapefruit Bananas Honeydew Coffee/Tea Kiwi Cantaloupe Pineapple Dates Plantains Eggplant Plums Tomatoes / tomato products Nuts (walnuts, pecans, hickory nuts, butternuts) • Do not drink alcoholic beverages for 2 days before or during the test. -

付表 ⅠA 指定を受けた医薬の有効成分 Annex ⅠA Designated
付表ⅠA 指定を受けた医薬の有効成分 Annex ⅠA Designated Pharmaceutical Active Ingredients 号(Sub-heading) 品名 Description 2818.30 アルゲルドラート algeldrate 2833.22 アルスルフ alusulf 2842.10 アルマシラート almasilate 2842.10 シマルドラート simaldrate 2842.90 硫酸アルマドラ ート almadrate sulfate 2842.90 アルマガート almagate 2842.90 カルバルドラード carbaldrate 2842.90 ヒドロタルシト hydrotalcite 2842.90 マガルドラート magaldrate 2843.30 オーラノフィン auranofin 2843.30 金チオグリカニド aurothioglycanide 2843.30 金チオりんご酸ナトリウム sodium aurothiomalate 2843.30 金チオ硫酸ナトリウム sodium aurotiosulfate 2843.90 カルボプラチン carboplatin 2843.90 シスプラチン cisplatin 2843.90 デキソルマプラチン dexormaplatin 2843.90 エンロプラチン enloplatin 2843.90 イプロプラチン iproplatin 2843.90 ロバプラチン lobaplatin 2843.90 ミボプラチン miboplatin 2843.90 ネダプラチン nedaplatin 2843.90 オルマプラチン ormaplatin 2843.90 オキサリプラチン oxaliplatin 2843.90 セブリプラチン sebriplatin 2843.90 スピロプラチン spiroplatin 2843.90 ゼニプラチン zeniplatin 2844.40 アルツモマブ altumomab 2844.40 塩化セシウム(131Cs) cesium (131 Cs) chloride 2844.40 クロルメロドリン(197Hg) chlormerodrin (197 Hg) 2844.40 シアノコバラミン(57Co) cyanocobalamin (57 Co) 2844.40 シアノコバラミン(58Co) cyanocobalamin (58 Co) 2844.40 シアノコバラミン(60Co) cyanocobalamin (60 Co) 2844.40 エチオダイズド油(131I) ethiodized oil (131 I) 2844.40 くえん酸第二鉄(59Fe)注射液 ferric (59 Fe) citrate in 2844.40 フィブリノゲン(125I) fibrinogen (125 I) 2844.40 フルデオキシグルコー ス(18F) fludeoxyglucose ( 18 F) 2844.40 フルオロドパ(18F) fluorodopa (18 F) 2844.40 くえん酸ガリウム(67Ga) gallium (67 Ga) citrate 2844.40 金コロイド(198Au) gold (198 Au), colloidal 2844.40 イオベングアン(131I) iobenguane (131 I) 2844.40 よう化人血清アルブミン(125I) iodinated (125 I) human serum albumin 2844.40 よう化人血清アルブミン(131I) iodinated -

Datasheet Inhibitors / Agonists / Screening Libraries a DRUG SCREENING EXPERT
Datasheet Inhibitors / Agonists / Screening Libraries A DRUG SCREENING EXPERT Product Name : Fenchlonine Catalog Number : T1447 CAS Number : 7424-00-2 Molecular Formula : C9H10CINO2 Molecular Weight : 199.63 Apprearence : Solid Melting Point : >240°C Description: Fenclonine is a selective and irreversible inhibitor of tryptophan hydroxylase, a rate-limiting enzyme in the biosynthesis of serotonin (5-HYDROXYTRYPTAMINE). Fenclonine acts pharmacologically to deplete endogenous levels of serotonin. Storage: 2 years -80°C in solvent; 3 years -20°C powder; DMSO 2 mg/mL (10 mM) Solubility Water Insoluble ( < 1 mg/ml refers to the product slightly soluble or insoluble ) Receptor (IC50) Hydroxylases In vivo Activity 4-Chloro-DL-phenylalanine(PCPA) markedly attenuates MCT(monocrotaline)-induced pulmonary vascular remodeling and lung inflammation, inhibits the expression of Tph-1 and SERT and suppresses the expression of MMP-2/-9, TIMP-1/-2, interleukin-1β (IL-1β), tumor necrosis factor-α (TNF-α) and intercellular adhesion molecule-1 (ICAM-1). PCPA inhibits 5-HT by suppressing Tph-1, regulating SERT and the serotonin downstream signaling pathway[1]. Animal Experiment Animal Model: Sprague-Dawley (SD) rats Reference 1. Bai Y, et al. Int J Mol Med. 2014, 33(2):373-382. FOR RESEARCH PURPOSES ONLY. NOT FOR DIAGNOSTIC OR THERAPEUTIC USE. Information for product storage and handling is indicated on the product datasheet. Targetmol products are stable for long term under the recommended storage conditions. Our products may be shipped under different conditions as many of them are stable in the short-term at higher or even room temperatures. We ensure that the product is shipped under conditions that will maintain the quality of the reagents. -

Ratio of Phosphate to Amino Acids
National Institute for Health and Care Excellence Final Neonatal parenteral nutrition [D10] Ratio of phosphate to amino acids NICE guideline NG154 Evidence reviews February 2020 Final These evidence reviews were developed by the National Guideline Alliance which is part of the Royal College of Obstetricians and Gynaecologists FINAL Error! No text of specified style in document. Disclaimer The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian. Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties. NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government, Scottish Government, and Northern Ireland Executive. -

Pharmaceuticals Appendix
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ADAPALENE 106685-40-9 ABANOQUIL 90402-40-7 ADAPROLOL 101479-70-3 ABECARNIL 111841-85-1 ADEMETIONINE 17176-17-9 ABLUKAST 96566-25-5 ADENOSINE PHOSPHATE 61-19-8 ABUNIDAZOLE 91017-58-2 ADIBENDAN 100510-33-6 ACADESINE 2627-69-2 ADICILLIN 525-94-0 ACAMPROSATE 77337-76-9 ADIMOLOL 78459-19-5 ACAPRAZINE 55485-20-6 ADINAZOLAM 37115-32-5 ACARBOSE 56180-94-0 ADIPHENINE 64-95-9 ACEBROCHOL 514-50-1 ADIPIODONE 606-17-7 ACEBURIC ACID 26976-72-7 ADITEREN 56066-19-4 ACEBUTOLOL 37517-30-9 ADITOPRIME 56066-63-8 ACECAINIDE 32795-44-1 ADOSOPINE 88124-26-9 ACECARBROMAL 77-66-7 ADOZELESIN 110314-48-2 ACECLIDINE 827-61-2 ADRAFINIL 63547-13-7 ACECLOFENAC 89796-99-6 ADRENALONE 99-45-6 ACEDAPSONE 77-46-3 AFALANINE 2901-75-9 ACEDIASULFONE SODIUM 127-60-6 AFLOQUALONE 56287-74-2 ACEDOBEN 556-08-1 AFUROLOL 65776-67-2 ACEFLURANOL 80595-73-9 AGANODINE 86696-87-9 ACEFURTIAMINE 10072-48-7 AKLOMIDE 3011-89-0 ACEFYLLINE CLOFIBROL 70788-27-1 -

The Activation of Α1-Adrenoceptors Is Implicated in the Antidepressant-Like Effect of Creatine in the Tail Suspension Test
CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector Progress in Neuro-Psychopharmacology & Biological Psychiatry 44 (2013) 39–50 Contents lists available at SciVerse ScienceDirect Progress in Neuro-Psychopharmacology & Biological Psychiatry journal homepage: www.elsevier.com/locate/pnp The activation of α1-adrenoceptors is implicated in the antidepressant-like effect of creatine in the tail suspension test Mauricio P. Cunha, Francis L. Pazini, Ágatha Oliveira, Luis E.B. Bettio, Julia M. Rosa, Daniele G. Machado, Ana Lúcia S. Rodrigues ⁎ Department of Biochemistry, Center of Biological Sciences, Universidade Federal de Santa Catarina, 88040-900, Florianópolis, SC, Brazil article info abstract Article history: The antidepressant-like activity of creatine in the tail suspension test (TST) was demonstrated previously by Received 5 September 2012 our group. In this study we investigated the involvement of the noradrenergic system in the Received in revised form 8 January 2013 antidepressant-like effect of creatine in the mouse TST. In the first set of experiments, creatine administered Accepted 18 January 2013 by i.c.v. route (1 μg/site) decreased the immobility time in the TST, suggesting the central effect of this com- Available online 26 January 2013 pound. The anti-immobility effect of peripheral administration of creatine (1 mg/kg, p.o.) was prevented by the pretreatment of mice with α-methyl-p-tyrosine (100 mg/kg, i.p., inhibitor of tyrosine hydroxylase), Keywords: α α Antidepressant prazosin -

Tyrosine Hydroxylase Inhibition in Substantia Nigra Decreases Movement Frequency
Molecular Neurobiology (2019) 56:2728–2740 https://doi.org/10.1007/s12035-018-1256-9 Tyrosine Hydroxylase Inhibition in Substantia Nigra Decreases Movement Frequency Michael F. Salvatore1 & Tamara R. McInnis1 & Mark A. Cantu1 & Deana M. Apple2 & Brandon S. Pruett3,4 Received: 23 May 2018 /Accepted: 17 July 2018 /Published online: 28 July 2018 # Springer Science+Business Media, LLC, part of Springer Nature 2018 Abstract Reduced movement frequency or physical activity (bradykinesia) occurs with high prevalence in the elderly. However, loss of striatal tyrosine hydroxylase (TH) in aging humans, non-human primates, or rodents does not reach the ~ 80% loss threshold associated with bradykinesia onset in Parkinson’s disease. Moderate striatal dopamine (DA) loss, either following TH inhibition or decreased TH expression, may not affect movement frequency. In contrast, moderate DA or TH loss in the substantia nigra (SN), as occurs in aging, is of similar magnitude (~ 40%) to nigral TH loss at bradykinesia onset in Parkinson’sdisease.Inaged rats, increased TH expression and DA in SN alone increases movement frequency, suggesting aging-related TH and DA loss in the SN contributes to aging-related bradykinesia or decreased physical activity. To test this hypothesis, the SN was targeted with bilateral guide cannula in young (6 months old) rats, in a within-subjects design, to evaluate the impact of nigral TH inhibition on movement frequency and speed. The TH inhibitor, α-methyl-p-tyrosine (AMPT) reduced nigral DA (~ 40%) 45–150 min following infusion, without affecting DA in striatum, nucleus accumbens, or adjacent ventral tegmental area. Locomotor activity in the open-field was recorded up to 3 h following nigral saline or AMPT infusion in each test subject. -

Pharmaceutical Appendix to the Tariff Schedule 2
Harmonized Tariff Schedule of the United States (2007) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2007) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. ABACAVIR 136470-78-5 ACIDUM LIDADRONICUM 63132-38-7 ABAFUNGIN 129639-79-8 ACIDUM SALCAPROZICUM 183990-46-7 ABAMECTIN 65195-55-3 ACIDUM SALCLOBUZICUM 387825-03-8 ABANOQUIL 90402-40-7 ACIFRAN 72420-38-3 ABAPERIDONUM 183849-43-6 ACIPIMOX 51037-30-0 ABARELIX 183552-38-7 ACITAZANOLAST 114607-46-4 ABATACEPTUM 332348-12-6 ACITEMATE 101197-99-3 ABCIXIMAB 143653-53-6 ACITRETIN 55079-83-9 ABECARNIL 111841-85-1 ACIVICIN 42228-92-2 ABETIMUSUM 167362-48-3 ACLANTATE 39633-62-0 ABIRATERONE 154229-19-3 ACLARUBICIN 57576-44-0 ABITESARTAN 137882-98-5 ACLATONIUM NAPADISILATE 55077-30-0 ABLUKAST 96566-25-5 ACODAZOLE 79152-85-5 ABRINEURINUM 178535-93-8 ACOLBIFENUM 182167-02-8 ABUNIDAZOLE 91017-58-2 ACONIAZIDE 13410-86-1 ACADESINE 2627-69-2 ACOTIAMIDUM 185106-16-5 ACAMPROSATE 77337-76-9 -

Induced Catecholamine Depletion in Patients with Seasonal Affective Disorder in Summer Remission Raymond W
Effects of Alpha-Methyl-Para-Tyrosine- Induced Catecholamine Depletion in Patients with Seasonal Affective Disorder in Summer Remission Raymond W. Lam, M.D., Edwin M. Tam, M.D.C.M., Arvinder Grewal, B.A., and Lakshmi N. Yatham, M.B.B.S. Noradrenergic and dopaminergic mechanisms have been the control diphenhydramine session. The AMPT session proposed for the pathophysiology of seasonal affective resulted in higher depression ratings with all nine patients disorder (SAD). We investigated the effects of having significant clinical relapse, compared with two catecholamine depletion using ␣-methyl-para-tyrosine patients during the diphenhydramine session. All patients (AMPT), an inhibitor of tyrosine hydroxylase, in patients returned to baseline scores after drug discontinuation. with SAD in natural summer remission. Nine drug-free Catecholamine depletion results in significant clinical patients with SAD by DSM-IV criteria, in summer relapse in patients with SAD in the untreated, summer- remission for at least eight weeks, completed a double-blind, remitted state. AMPT-induced depressive relapse may be a crossover study. Behavioral ratings and serum HVA and trait marker for SAD, and/or brain catecholamines may MHPG levels were obtained for 3-day sessions during play a direct role in the pathogenesis of SAD. which patients took AMPT or an active control drug, [Neuropsychopharmacology 25:S97–S101, 2001] diphenhydramine.The active AMPT session significantly © 2001 American College of Neuropsychopharmacology. reduced serum levels of HVA and MHPG compared with Published by Elsevier Science Inc. KEY WORDS: Seasonal affective disorder; Alpha-methyl- pattern, with full remission of symptoms (or a switch para-tyrosine; Catecholamines; Dopamine; Noradrenaline; into hypomania/mania) during spring/summer. -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0 -

PHARMACEUTICAL APPENDIX to the HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2008) (Rev
Harmonized Tariff Schedule of the United States (2008) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2008) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. ABACAVIR 136470-78-5 ACIDUM GADOCOLETICUM 280776-87-6 ABAFUNGIN 129639-79-8 ACIDUM LIDADRONICUM 63132-38-7 ABAMECTIN 65195-55-3 ACIDUM SALCAPROZICUM 183990-46-7 ABANOQUIL 90402-40-7 ACIDUM SALCLOBUZICUM 387825-03-8 ABAPERIDONUM 183849-43-6 ACIFRAN 72420-38-3 ABARELIX 183552-38-7 ACIPIMOX 51037-30-0 ABATACEPTUM 332348-12-6 ACITAZANOLAST 114607-46-4 ABCIXIMAB 143653-53-6 ACITEMATE 101197-99-3 ABECARNIL 111841-85-1 ACITRETIN 55079-83-9 ABETIMUSUM 167362-48-3 ACIVICIN 42228-92-2 ABIRATERONE 154229-19-3 ACLANTATE 39633-62-0 ABITESARTAN 137882-98-5 ACLARUBICIN 57576-44-0 ABLUKAST 96566-25-5 ACLATONIUM NAPADISILATE 55077-30-0 ABRINEURINUM 178535-93-8 ACODAZOLE 79152-85-5 ABUNIDAZOLE 91017-58-2 ACOLBIFENUM 182167-02-8 ACADESINE 2627-69-2 ACONIAZIDE 13410-86-1 ACAMPROSATE -
Adipocytes As a New Source of Catecholamine Production
CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector FEBS Letters 585 (2011) 2279–2284 journal homepage: www.FEBSLetters.org Adipocytes as a new source of catecholamine production ⇑ Peter Vargovic a, , Jozef Ukropec b, Marcela Laukova a, Susannah Cleary d, Bernhard Manz c, Karel Pacak d, Richard Kvetnansky a a Laboratory of Stress Research, Institute of Experimental Endocrinology, Slovak Academy of Sciences, Vlarska 3, 83306 Bratislava, Slovakia b Diabetes and Metabolic Research Laboratory, Institute of Experimental Endocrinology, Slovak Academy of Sciences, Vlarska 3, 83306 Bratislava, Slovakia c LDN Labor Diagnostika Nord, D-48531 Nordhorn, Germany d Section on Medical Neuroendocrinology, NICHD, NIH, Bethesda, MD, USA article info abstract Article history: Catecholamines are an important regulator of lipolysis in adipose tissue. Here we show that rat adi- Received 2 February 2011 pocytes, isolated from mesenteric adipose tissue, express genes of catecholamine biosynthetic Revised 28 April 2011 enzymes and produce catecholamines de novo. Administration of tyrosine hydroxylase inhibitor, Accepted 1 June 2011 alpha-methyl-p-tyrosine, in vitro significantly reduced concentration of catecholamines in isolated Available online 16 June 2011 adipocytes. We hypothesize that the sympathetic innervation of adipose tissues is not the only Edited by Laszlo Nagy source of catecholamines, since adipocytes also have the capacity to produce both norepinephrine and epinephrine. Ó 2011 Federation of European Biochemical Societies. Published by Elsevier B.V. All rights reserved. Keywords: Adipocyte Endogenous catecholamine Catecholamine biosynthetic enzyme Gene expression 1. Introduction catecholamine biosynthesis. PNMT mRNA and immunoreactive protein were found in the adipose tissue in neuron-like cells of Adipose tissue is a specialized organ serving several functions PNMT-overexpressing transgenic mice but not in wild types [10].