The Management of the Contracted First Web Space
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

14-Anatomy of Forearm
FOREARM By : Prof.Saeed Abulmakarem. Dr. Sanaa Al-Sharawy OBJECTIVES §At the end of this lecture, the student should able to : §List the names of the Flexors Group of Forearm (superficial & deep muscles). §Identify the common flexor origin of flexor muscles and their innervation & movements. §Identify supination & poronation and list the muscles produced these 2 movements. §List the names of the Extensor Group of Forearm (superficial & deep muscles). §Identify the common extensor origin of extensor musles and their innervation & movements. n The forearm extends from elbow to wrist. n It posses two bones radius laterally & Ulna medially. n The two bones are connected together by the interosseous membrane. n This membrane allows movement of Pronation and Supination while the two bones are connected together. n Also it gives origin for the deep muscles. § The forearm is Fascial Compartments of the Forearm enclosed in a sheath of deep fascia, which is attached to the posterior border of the ulna . §This fascial sheath, together with the interosseous membrane & fibrous intermuscular septa, divides the forearm into compartments, each having its own muscles, nerves, and blood supply. These muscles: 8 FLEXOR GROUP § Act on the elbow & wrist joints and those of the fingers. § Form fleshy masses in the proximal part and become tendinous in the distal part of the forearm. •Arranged in three groups: I-Superficial: 4 Ø Pronator teres Ø Flexor carpi radialis Ø Palmaris longus III- Deep: 3 Ø Flexor carpi ulnaris Ø Flexor digitorum profundus II-Intermediate: 1 Ø Flexor pollicis longus Ø Ø Flexor digitorum superficialis Pronator quadratus n Superficial Flexors: n They arise - more or less- from the common flexor origin (front of medial epicondyle). -

And Thoracic Outlet Syndrome
• Palpatory diagnosis and manipulative management of carpal tunnel syndrome: Part 2. 'Double crush' and thoracic outlet syndrome BENJAMIN M. SUCHER, DO 1( The physician treating carpal nificant. Ultimately, palpatory assessment was tunnel syndrome needs to be aware of the instrumental in guiding the author with initial or possible concomitant occurrence of thoracic subsequent methods (or both) of effective treat outlet syndrome, the so-called double crush syn ment. Palpatory monitoring was the key to clinical drome. Palpation is used to differentiate carpal management in all cases. tunnel syndrome from thoracic outlet syn drome. Such palpatory examination assists Methods the physician in planning the initial treat Patients with CTS were assessed as previously described.? ment, including osteopathic manipulation They all underwent electrodiagnostic testing, which and self-stretching maneuvers, targeted specif included a minimum of median and ulnar distal motor ically at the most clinically significant patho and sensory conduction studies. Needle electromyograms logic region. Supplemental physical medicine and more extensive conduction studies were also per formed if not done previously, or as clinically indicated. modalities such as ultrasound may enhance They were treated according to the outlined protocols the treatment response. Some illustrative for osteopathic manipulation and self-stretching exer cases are reported. cises.B,9 Palpatory assessment routinely included axial rota (Key words: Carpal tunnel syndrome, osteo tion. When restriction was noted for this motion, treat pathic manipulation, thoracic outlet syn ment included the "opponens roll"? technique. As a drome, double crush syndrome) self-stretch maneuver, the thumb is abducted with slight extension and rotated laterally (Figure 1). The primary The initial presentation of carpal tunnel syn limitations or precautions to this new self-stretch involve advanced degenerative changes in the first carpometacarpal drome (CTS) often is a diagnostic challenge, espe joint and bilateral CTS. -

Small Muscles of the Hand
By the name of Allah Small muscles of the hand Revision: The palmar aponeurosis is triangular in shape with apex and base. It is divided into 4 bands that radiate to the medial four fingers. Dupuytren’s Contracture: • A localized thickening and shortening of palmar aponeurosis that limits hand function (it is permanent) • Fibrosis pulls the ring finger then the little finger into partial flexion at the MCP joints, followed by flexion of their proximal interphalangeal joints • Usual treatment: Treated by surgical excision of fibrous bands followed by physiotherapy. Alternative treatment: Injection of the enzyme Collagenase into the contracted bands of the fibrous tissue. Keep in mind: • When the muscle Isn’t functioning: It is Relaxed. While it is in action: It is contracted. • Contraction DIFFERS from contracture. Contracture means permanent shortening. 18 th \Mar\2012 1 Small muscles of the hand: Arranged in five groups + 1 muscle, as the following: 1- Thenar muscles: (three in number) each moves the thumb according to its name: • Flexor pollicis brevis: assists the flexor pollicis longus in the flexion of MCP joint of the thumb. • Abductor pollicis brevis: abduction of the thumb. • Opponens pollicis: pulls the thumb medially and forward across the palm (as in counting fingers, shown in the figure below). All supplied by median nerve. 2- Hypothenar muscles: (three in number) each moves the little finger according to its name: • Flexor digiti minimi. • Abductor digit minimi. • Opponens digiti minimi. All supplied by deep branch of ulnar nerve. Only the thumb and little finger got opponens muscles, the Dr said it is because of the long distance between the two fingers ☺ 3- Adductor pollicis muscle: • It has got two heads: horizontal( transverse) and Oblique. -

Extensor Pollicis Longus Superficialis and Extensor Indicis Superficialis, Can They Be Considered As a New Anatomical Variation in the Long Extensors of Fingers?
Int. J. Curr. Res. Med. Sci. (2016). 2(12): 27-32 International Journal of Current Research in Medical Sciences ISSN: 2454-5716 www.ijcrims.com Volume 2, Issue 12 -2016 Case study DOI: http://dx.doi.org/10.22192/ijcrms.2016.02.12.005 Extensor pollicis longus superficialis and extensor indicis superficialis, can they be considered as a new anatomical variation in the long extensors of fingers? Ahmed Farid Al-Neklawy, M.D. Anatomy and Embryology Department, Faculty of Medicine, Ain Shams University, Cairo, Egypt E-mail: [email protected], Tel: 00201001850336 Running title: Two extra muscles for thumb and index fingers Abstract Background: Variations of anomalies of hand extensors have been described by many authors. These anomalies are often discovered during routine surgical procedures and cadaveric dissections. Being aware of such anomalies is important to the physician in order to avoid unintentional damage to healthy tendons during surgical procedures. In addition, accessory tendons have the potential to be used in the surgical repair or replacement of damaged tendons. We reported a cadaveric case with bilateral two additional superficial extensors to the thumb and index fingers with unique features. The names of extensor pollicis longus superficialis (EPL-S) and extensor indicis superficialis(EI-S) were proposed. Methods: A female cadaver was used in this study. Bilateral dissection of the forearm and wrist was done. Results: Two extra muscles were observed in the superficial group of the extensors of the forearm. They were situated between extensor carpi radialis brevis and extensor digitorum muscles. Both muscles originated from the common extensor origin. -

Section 1 Upper Limb Anatomy 1) with Regard to the Pectoral Girdle
Section 1 Upper Limb Anatomy 1) With regard to the pectoral girdle: a) contains three joints, the sternoclavicular, the acromioclavicular and the glenohumeral b) serratus anterior, the rhomboids and subclavius attach the scapula to the axial skeleton c) pectoralis major and deltoid are the only muscular attachments between the clavicle and the upper limb d) teres major provides attachment between the axial skeleton and the girdle 2) Choose the odd muscle out as regards insertion/origin: a) supraspinatus b) subscapularis c) biceps d) teres minor e) deltoid 3) Which muscle does not insert in or next to the intertubecular groove of the upper humerus? a) pectoralis major b) pectoralis minor c) latissimus dorsi d) teres major 4) Identify the incorrect pairing for testing muscles: a) latissimus dorsi – abduct to 60° and adduct against resistance b) trapezius – shrug shoulders against resistance c) rhomboids – place hands on hips and draw elbows back and scapulae together d) serratus anterior – push with arms outstretched against a wall 5) Identify the incorrect innervation: a) subclavius – own nerve from the brachial plexus b) serratus anterior – long thoracic nerve c) clavicular head of pectoralis major – medial pectoral nerve d) latissimus dorsi – dorsal scapular nerve e) trapezius – accessory nerve 6) Which muscle does not extend from the posterior surface of the scapula to the greater tubercle of the humerus? a) teres major b) infraspinatus c) supraspinatus d) teres minor 7) With regard to action, which muscle is the odd one out? a) teres -
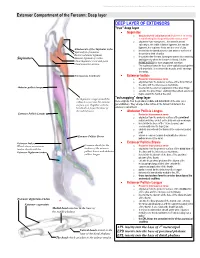
Extensor Compartment of the Forearm: Deep Layer
This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. Extensor Compartment of the Forearm: Deep layer DEEP LAYER OF EXTENSORS "true" deep layer Supinator o deep branch of radial nerve which pierces it on its way to transforming into the posterior interosseous nerve o originates from everywhere... the lateral humeral epicondyle, the radial collateral ligament, the annular ligament, the supinator fossa and the crest of ulna Attachments of the Supinator to the o inserts into the lateral posterior and anterior surfaces of Epicondyle of humerus the proximal third of radius Radial collateral ligament o it supinates the forearm, turning the arm to face anteriorly Annular ligament of radius Supinator and superiorly when the forearm is flexed. It is the Ulnar Supinator crest and fossa PRIME MOVER for slow unopposed suination Ulnar posterior surface o The supinator forms the floor of the cubital fossa together with brachialis. It is a sheet-like muscle, and it envelops the radius. Interosseous membrane Extensor Indicis o Posterior interosseous nerve o originates from the posterior surface of the distal third of the ulna, and the interosseous membrane Abductor pollicis longus o inserts into the extensor expansion of the index finger o extends the index finger, enabling independent extension o helps extend the hand at the wrist "outcropping" deep layer the Supinator wraps around the radius to insert into the anterior these originate from the proximal, middle and distal thirds of the ulna (as a surface of it. -
Structural Kinesiology Class 19 Clearing Scars
STRUCTURAL KINESIOLOGY CLASS 19 With John Maguire WHAT WE WILL COVER IN THIS CLASS How to test and clear scars using three approaches: Upper Limb Muscles • Stroking • Teres Major • Oil & Stretch • Coracobrachialis • Figure 8’s • Brachiordialis • Triceps • Opponens Policis 2 CLEARING SCARS About 75% of scars cause an indicator change when Circuit Located (CL’ed). This means there is some energy block through the scar tissue and it has lost its ability to properly transmit chi. Testing to find out if a scar needs clearing: 1. While either you or the person being tested touches the scar, test a previously strong IM. If the scar CL’s, showing indicator weakening, one of the three procedures on the following pages may help. 2. If there is no IM change, touch the frontal eminences and recheck the scar to see if it is hidden. 3. Injury Recall Technique (IRT) may be needed if an accident was involved, which was covered in Class 1. 3 SCAR CORRECTIONS To determine which corrections to use, CL the scar and state: 1. “Stroking” (test) 2. “Oil and Stretch” (test) 3. “Figure 8’s” (test) The one which strengthens the indicator muscle (IM) is the one to use. 4 STROKING SCAR CORRECTION Stroking: 1. Lightly stroke across the scar to find the weakening direction. 2. Find the phase of breath which strengthens (usually the inhalation). 3. Stroke several times in the weaken direction with the strong breath. Work the full length of the scar. 4. Ask if there is a strong emotion related to the scar and if so, have the person hold their frontal eminences and think about the emotion while the correction is being made. -

Deep Dry Needling of the Arm and Hand Muscles 8
Deep dry needling of the arm and hand muscles 8 César Fernández-de-las-Peñas Javier González Iglesias Christian Gröbli Ricky Weissmann CHAPTER CONTENT conditions. Symptoms in the upper quadrant, including the neck, shoulder, arm, forearm, or Introduction . 107 hand not related to an acute trauma or underly- Clinical relevance of TrPs in arm ing systemic diseases, can be provoked by trigger and hand pain syndromes . 108 points (TrPs). In fact, there are several neck and Dry needling of the arm and hand muscles . 108 shoulder muscles with referred pain pattern being perceived throughout the upper extremity, e.g. Coracobrachialis muscle. 108 the scalenes, subclavius, pectoralis minor, supra- Biceps brachii muscle (short head) . 109 spinatus, infraspinatus, subscapularis, pectoralis Triceps brachii muscle (lower portion) . 109 major, latissimus dorsi, serratus posterior supe- Anconeus muscle . 110 rior and serratus anterior muscles ( Simons et al. Brachialis muscle . 110 1999 ). For instance, Qerama et al. (2009) dem- Brachioradialis muscle . 111 onstrated that 49% of individuals with normal electrophysiological findings in the median nerve, Supinator muscle . 111 but with symptoms mimicking carpal tunnel syn- Wrist and fi nger extensor muscles. 112 drome, presented with active TrPs in the infra- Pronator teres muscle . 113 spinatus muscle with paresthesia and referred Wrist and fi nger fl exor muscles . 113 pain to the arm and fingers. In the same study, Flexor pollicis longus, extensor pollicis patients with mild electrophysiological signs of longus, and abductor pollicis longus . 114 carpal tunnel syndrome exhibited a significantly Extensor indicis muscle . 115 higher occurrence of infraspinatus muscle TrPs in the symptomatic arm as compared with patients Adductor pollicis, opponens pollicis, with moderate to severe electrophysiological fl exor pollicis brevis, and abductor pollicis brevis muscles . -

Axis Scientific Hand Model with Deep Layers A-105873
Axis Scientific Hand Model with Deep Layers A-105873 17. Abductor Digiti Minimi Muscle 03. Abductor Pollicis Brevis 01. Palmar Aponeurosis Muscle 03. Abductor Pollicis Brevis Muscle 06. Adductor 18. Flexor Digiti Minimi Brevis Muscle Pollicis Muscle 02. Palmaris Brevis Muscle 11. Ulnar Nerve 21. Palmar Interosseous 12. Ulnar Artery Muscles 22. Palmar 07. Tendon of Palmaris Metacarpal Longus Arteries 20. Deep Palmar (Arterial) Arch 19. Opponens Digiti 04. Flexor Pollicis Brevis Muscle Minimi Muscle 05. Opponens Pollicis Muscle 18. Flexor Digiti Minimi Brevis Muscle 10. Lumbrical 28. Dorsal Interosseous Muscles Muscles 16. Superficial 26. Dorsal Venous Network Palmar Branch of 23. Superficial Branch of Palmar Nerve Radial Artery 25. Radial Artery 24. Dorsal Branch of Ulnar Nerve 27. Extensor Digitorum Tendon 14. 08. Transverse 13. Superficial Median 15. Common Carpal Palmar Arch Nerve Palmar Digital Ligament Nerves and Arteries 07. Tendon 09. Flexor Digitorum of Palmaris Superficialis Tendons Longus 15. Common Palmar Digital 01. Palmar Aponeurosis Nerves and Arteries 16. Superficial Palmar 02. Palmaris Brevis Muscle Branch of Radial Artery 03. Abductor Pollicis Brevis Muscle 17. Abductor Digiti Minimi Muscle 18. Flexor Digiti 04. Flexor Pollicis Brevis Muscle Minimi Brevis Muscle 19. Opponens Digiti 05. Opponens Pollicis Muscle Minimi Muscle 06. Adductor Pollicis Muscle 20. Deep Palmar (Arterial) Arch 07. Tendon of Palmaris Longus 21. Palmar Interosseous Muscles 08. Transverse Carpal Ligament 22. Palmar Metacarpal Arteries 09. Flexor Digitorum Superficialis 23. Superficial Branch of Tendons Palmar Nerve 10. Lumbrical Muscle 24. Dorsal Branch of Ulnar Nerve 11. Ulnar Nerve 25. Radial Artery 26. Dorsal Venous 12. Ulnar Artery Network of Hand 13. -

Upper Limb : Muscles "Revision" Anatomy Team 434
Upper Limb : Muscles "Revision" Anatomy Team 434 Color Index: If you have any complaint or ▪ Important Points suggestion please don’t ▪ Helping notes hesitate to contact us on: [email protected] ▪ Explanation Muscles of shoulder region Muscle ORIGIN INSERTION ACTION NERVE Lateral 1/3 of clavicle + Deltoid tuberosity of Deltoid acromion and spine of Major abductor of the arm humerus scapula Axillary nerve Greater tuberosity of Teres minor Laterally rotates the arm humerus Lateral border of scapula Adducts at the shoulder and Teres major Bicipital groove of humerus Lower subscapular nerve medially rotates the arm Abducts the arm 0-15o, and Supraspinatus Supraspinous fossa Greater tuberosity of assists deltoid for 15-90o Suprascapular nerve humerus Infraspinatus Infraspinous fossa Laterally rotates the arm Lesser tuberosity of Upper and lower Subscapularis Subscapular fossa Medially rotates the arm humerus subscapular nerves All the pictures are taken from [ http://teachmeanatomy.info/ ] .. Muscles of pectoral region Muscle ORIGIN INSERTION ACTION NERVE -Sternum, -Adduct and medially rotate the Medial and Pectoralis -Upper 6 costal cartilages humerus Lateral lip of bicipital groove lateral pectoral major -Aponeurosis of external -The clavicular head also nerves oblique muscle performs flexion -Depression of shoulder Pectoralis 3rd, 4th, & 5th ribs close Medial pectoral Coracoid process -Draw the ribs upward & minor to their costal cartilages nerve outwards during deep inspiration Steadies or fixes the clavicle 1st rib at its costal Subclavian groove at the inferior Nerve to Subclavius during movement of the shoulder cartilage surface of middle 1/3 of clavicle subclavius joint -Draws the scapula forward -Rotates scapula outwards in Serratus Ventral aspect of the medial border Long thoracic Upper eight ribs raising the arm above 90 degree. -

* the Function of Extensor Digitorum
Forearm Arteries and nerves Revision: ☻The function of extensor digitorum : It extends the medial 4 fingers and the wrist. ☻The 4 tendons of the extensor digitorum flatten over the proximal phalanges of the medial 4 fingers to form extensor expansion (extensor hood) in some books. ☻The extensor expansion divides into 3 divisions: •One is central •Two are laterals. ☻Extensor expansion receives: • interosseous muscle on each side(palmar interossei and dorsal interossei) • Lumbrical(worm-like) muscle on the lateral side. ☻The function of extensor expansion when these small muscles attached to it : 1- flexion of matacarpophalangeal (MCP) joints. 2- extension of interphalangeal joints Main function : writing position Arteries: Brachial artery divides at opposite neck of radius into two branches: 1-ulnar artery (larger) 2- radial artery (smaller) ulnar ☻They both reach the wrist. artery Ulnar artery (larger): ☻It passes above flexor retinaculum and divides into 2 branches: 1-superfecial branch (larger) Radial 2- deep branch (smaller) artery ☻Both of them will go to the hand. From medial to lateral pisiform (insertion of flexor carpi ulnaris) >>> ulnar nerve>>> ulnar artery Radial artery (smaller): ☻It is located on the floor of snuffbox. ☻In the snuffbox it divides into : 1-small superficial branch. 2- large deep branch. Palmar arches: Palm is supplied by a connection between vessels called ( anastomosis ) 1- superficial palmar arch. 2- deep palmer arch. Superficial palmer arch: ☻It is contributed from: 1-(mainly) superficial branch of ulnar artery (direct continuation of it). 2- smaller superficial branch of radial artery. ☻It is located at the distal level of the hyper extended thumb. -

Anatomical Variations of the Abductor Pollicis Longus: a Pilot Study P
Folia Morphol. Vol. 79, No. 4, pp. 817–822 DOI: 10.5603/FM.a2019.0134 O R I G I N A L A R T I C L E Copyright © 2020 Via Medica ISSN 0015–5659 journals.viamedica.pl Anatomical variations of the abductor pollicis longus: a pilot study P. Karauda1, Ł. Olewnik1, M. Podgórski2, M. Polguj1, K. Ruzik1, B. Szewczyk3, M. Topol1 1Department of Normal and Clinical Anatomy, Interfaculty Chair of Anatomy and Histology, Medical University of Lodz, Poland 2Department of Diagnostic Imaging, Polish Mother’s Memorial Hospital Research Institute, Lodz, Poland 3Department of Clinical Morphology, Medical University of Lodz, Poland [Received: 12 October 2019; Accepted: 3 November 2019] Background: The abductor pollicis longus (APL) originates from the lateral part of the dorsal surface of the body of the ulna below the insertion of the anconeus muscle, from the interosseous membrane, and from the middle third of the dorsal surface of the body of the radius. However, the number of its accessory bands and their insertion vary considerably. Materials and methods: Fifty upper limbs (2 paired, 31 male, 19 female) were obtained from adult Caucasian cadavers, and fixed in 10% formalin solution before examination. Results: The APL muscle was present in all specimens. The muscles were divided into three main categories, with type II and III being dived into subtypes. Type I was characterised by a single distal attachment, with the tendon inserting to the base of the I metacarpal bone. Type II was characterised by a bifurcated distal attachment, with the main tendon inserting to the base of the first metacarpal bone; this type was divided into three subtypes (a–c).