Initial Assessment of London Bus Driver Mortality from Covid-19
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Simply the Best Buses in Britain
Issue 100 | November 2013 Y A R N A N I S V R E E R V S I A N R N Y A onThe newsletter stage of Stagecoach Group CELEBRATING THE 100th EDITION OF STAGECOACH GROUP’S STAFF MAGAZINE Continental Simply the best coaches go further MEGABUS.COM has buses in Britain expanded its network of budget services to Stagecoach earns host of awards at UK Bus event include new European destinations, running STAGECOACH officially runs the best services in Germany buses in Britain. for the first time thanks Stagecoach Manchester won the City Operator of to a new link between the Year Award at the recent 2013 UK Bus Awards, London and Cologne. and was recalled to the winner’s podium when it was In addition, megabus.com named UK Bus Operator of the Year. now also serves Lille, Ghent, Speaking after the ceremony, which brought a Rotterdam and Antwerp for number of awards for Stagecoach teams and individuals, the first time, providing even Stagecoach UK Bus Managing Director Robert more choice for customers Montgomery said: “Once again our companies and travelling to Europe. employees have done us proud. megabus.com has also “We are delighted that their efforts in delivering recently introduced a fleet top-class, good-value bus services have been recognised of 10 left-hand-drive 72-seat with these awards.” The Stagecoach Manchester team receiving the City Van Hool coaches to operate Manchester driver John Ward received the Road Operator award. Pictured, from left, are: Operations Director on its network in Europe. -

English Counties
ENGLISH COUNTIES See also the Links section for additional web sites for many areas UPDATED 23/09/21 Please email any comments regarding this page to: [email protected] TRAVELINE SITES FOR ENGLAND GB National Traveline: www.traveline.info More-detailed local options: Traveline for Greater London: www.tfl.gov.uk Traveline for the North East: https://websites.durham.gov.uk/traveline/traveline- plan-your-journey.html Traveline for the South West: www.travelinesw.com Traveline for the West & East Midlands: www.travelinemidlands.co.uk Black enquiry line numbers indicate a full timetable service; red numbers imply the facility is only for general information, including requesting timetables. Please note that all details shown regarding timetables, maps or other publicity, refer only to PRINTED material and not to any other publications that a county or council might be showing on its web site. ENGLAND BEDFORDSHIRE BEDFORD Borough Council No publications Public Transport Team, Transport Operations Borough Hall, Cauldwell Street, Bedford MK42 9AP Tel: 01234 228337 Fax: 01234 228720 Email: [email protected] www.bedford.gov.uk/transport_and_streets/public_transport.aspx COUNTY ENQUIRY LINE: 01234 228337 (0800-1730 M-Th; 0800-1700 FO) PRINCIPAL OPERATORS & ENQUIRY LINES: Grant Palmer (01525 719719); Stagecoach East (01234 220030); Uno (01707 255764) CENTRAL BEDFORDSHIRE Council No publications Public Transport, Priory House, Monks Walk Chicksands, Shefford SG17 5TQ Tel: 0300 3008078 Fax: 01234 228720 Email: [email protected] -
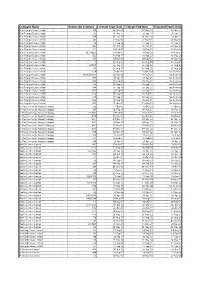
Operators Route Contracts
Company Name Routes On Contract Contract Start Date Contract End Date Extended Expiry Date Blue Triangle Buses Limited 300 06-Mar-10 07-Dec-18 03-Mar-17 Blue Triangle Buses Limited 193 01-Oct-11 28-Sep-18 28-Sep-18 Blue Triangle Buses Limited 364 01-Nov-14 01-Nov-19 29-Oct-21 Blue Triangle Buses Limited 147 07-May-16 07-May-21 05-May-23 Blue Triangle Buses Limited 376 17-Sep-16 17-Sep-21 15-Sep-23 Blue Triangle Buses Limited 346 01-Oct-16 01-Oct-21 29-Sep-23 Blue Triangle Buses Limited EL3 18-Feb-17 18-Feb-22 16-Feb-24 Blue Triangle Buses Limited EL1/NEL1 18-Feb-17 18-Feb-22 16-Feb-24 Blue Triangle Buses Limited EL2 18-Feb-17 18-Feb-22 16-Feb-24 Blue Triangle Buses Limited 101 04-Mar-17 04-Mar-22 01-Mar-24 Blue Triangle Buses Limited 5 26-Aug-17 26-Aug-22 23-Aug-24 Blue Triangle Buses Limited 15/N15 26-Aug-17 26-Aug-22 23-Aug-24 Blue Triangle Buses Limited 115 26-Aug-17 26-Aug-22 23-Aug-24 Blue Triangle Buses Limited 674 17-Oct-15 16-Oct-20 See footnote Blue Triangle Buses Limited 649/650/651 02-Jan-16 01-Jan-21 See footnote Blue Triangle Buses Limited 687 30-Apr-16 30-Apr-21 See footnote Blue Triangle Buses Limited 608 03-Sep-16 03-Sep-21 See footnote Blue Triangle Buses Limited 646 03-Sep-16 03-Sep-21 See footnote Blue Triangle Buses Limited 648 03-Sep-16 03-Sep-21 See footnote Blue Triangle Buses Limited 652 03-Sep-16 03-Sep-21 See footnote Blue Triangle Buses Limited 656 03-Sep-16 03-Sep-21 See footnote Blue Triangle Buses Limited 679 03-Sep-16 03-Sep-21 See footnote Blue Triangle Buses Limited 686 03-Sep-16 03-Sep-21 See footnote -

London and the South East of England: 15 July 2016
OFFICE OF THE TRAFFIC COMMISSIONER (LONDON AND THE SOUTH EAST OF ENGLAND) NOTICES AND PROCEEDINGS PUBLICATION NUMBER: 2359 PUBLICATION DATE: 15 July 2016 OBJECTION DEADLINE DATE: 05 August 2016 Correspondence should be addressed to: Office of the Traffic Commissioner (London and the South East of England) Hillcrest House 386 Harehills Lane Leeds LS9 6NF Telephone: 0300 123 9000 Fax: 0113 249 8142 Website: www.gov.uk/traffic-commissioners The public counter at the above office is open from 9.30am to 4pm Monday to Friday The next edition of Notices and Proceedings will be published on: 29/07/2016 Publication Price £3.50 (post free) This publication can be viewed by visiting our website at the above address. It is also available, free of charge, via e-mail. To use this service please send an e-mail with your details to: [email protected] Remember to keep your bus registrations up to date - check yours on https://www.gov.uk/manage-commercial-vehicle-operator-licence-online NOTICES AND PROCEEDINGS Important Information All correspondence relating to public inquiries should be sent to: Office of the Traffic Commissioner (London and the South East of England) Ivy House 3 Ivy Terrace Eastbourne BN21 4QT The public counter at the Eastbourne office is open for the receipt of documents between 9.30am and 4pm Monday Friday. There is no facility to make payments of any sort at the counter. General Notes Layout and presentation – Entries in each section (other than in section 5) are listed in alphabetical order. Each entry is prefaced by a reference number, which should be quoted in all correspondence or enquiries. -

The Go-Ahead Group Plc Annual Report and Accounts 2019 1 Stable Cash Generative
Annual Report and Accounts for the year ended 29 June 2019 Taking care of every journey Taking care of every journey Regional bus Regional bus market share (%) We run fully owned commercial bus businesses through our eight bus operations in the UK. Our 8,550 people and 3,055 buses provide Stagecoach: 26% excellent services for our customers in towns and cities on the south FirstGroup: 21% coast of England, in north east England, East Yorkshire and East Anglia Arriva: 14% as well as in vibrant cities like Brighton, Oxford and Manchester. Go-Ahead’s bus customers are the most satisfied in the UK; recently Go-Ahead: 11% achieving our highest customer satisfaction score of 92%. One of our National Express: 7% key strengths in this market is our devolved operating model through Others: 21% which our experienced management teams deliver customer focused strategies in their local areas. We are proud of the role we play in improving the health and wellbeing of our communities through reducing carbon 2621+14+11+7+21L emissions with cleaner buses and taking cars off the road. London & International bus London bus market share (%) In London, we operate tendered bus contracts for Transport for London (TfL), running around 157 routes out of 16 depots. TfL specify the routes Go-Ahead: 23% and service frequency with the Mayor of London setting fares. Contracts Metroline: 18% are tendered for five years with a possible two year extension, based on Arriva: 18% performance against punctuality targets. In addition to earning revenue Stagecoach: 13% for the mileage we operate, we have the opportunity to earn Quality Incentive Contract bonuses if we meet these targets. -

Operations Review
OPERATIONS REVIEW SINGAPORE PUBLIC TRANSPORT SERVICES (BUS & RAIL) • TAXI AUTOMOTIVE ENGINEERING SERVICES • INSPECTION & TESTING SERVICES DRIVING CENTRE • CAR RENTAL & LEASING • INSURANCE BROKING SERVICES OUTDOOR ADVERTISING Public Transport Services The inaugural On-Demand Public Bus ComfortDelGro Corporation Limited is Services trial, where SBS Transit operated a leading provider of land transport and five bus routes – three in the Joo Koon area related services in Singapore. and two in the Marina-Downtown area – for 2.26 the LTA ended in June 2019. Conducted REVENUE Scheduled Bus during off-peak hours on weekdays, (S$BILLION) SBS Transit Ltd entered into its fourth year commuters could book a ride with an app of operating under the Bus Contracting and request to be picked up and dropped Model (BCM) in 2019, where the provision off at any bus stop within the defined areas. of bus services and the corresponding It was concluded by the LTA that such bus standards are all determined by the Land services were not cost-effective due to Transport Authority (LTA). Under this model, the high technology costs required in the Government retains the fare revenue scaling up. and owns all infrastructure and operating assets such as depots and buses. A major highlight in 2019 was SBS Transit’s active involvement in the three-month long 17,358 Bus routes in Singapore are bundled into public trial of driverless buses on Sentosa TOTAL OPERATING 14 bus packages. Of these, SBS Transit Island with ST Engineering. Operated as an FLEET SIZE operated nine. During the year, it continued on-demand service, visitors on the island to be the biggest public bus operator with could book a shuttle ride on any of the a market share of 61.1%. -
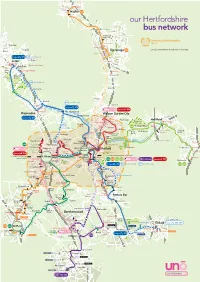
Uno Herts Network Map MASTER A3 UH Zone
Sainsbury’s Hitchin Walsworth Waitrose Road Queens St Asda Hitchin 635 Park St London Rd A602 A1(M) our Hertfordshire A602 Sainsbury’s Lister Hosptal bus network A602 Martins Way A1(M) Stevenage Old Town L y High St n t University of Hertfordshire o n Fairlands Way W zone 1 a Barnfield y Tesco Stevenage Monkswood Way Stopsley 635 zone 2 is everywhere else shown on this map Biscot Asda Stevenage North Hertfordshire College school days only 610 612 Stevenage FC Wigmore A602 A602 Luton Tesco B roa Luton NON STOP dw ate The Mall London Luton Airport r Cres Park Town A1(M) Matalan New Luton Airport Parkway Town Knebworth London Rd Capability Knebworth Stockwood Park Green B653 612 school days only Luton Hoo East Hyde Oaklands A1081 A1(M) L Welwyn NON STOP ut on R d Batford 612 school days only Sainsbury’s Lower Luton Rd Digswell 610 Station Rd Waitrose 601 653 Harpenden High St Wheathampstead Harpenden St Albans Rd l Welwyn Garden City l i Bro Marford Rd ck H Marshalls Heath s wood Ln Oaklands College e A1(M) 610 h B653 T H e Panshanger Hertford ro n Panshanger Welwyn Garden sw Hertford East o Park A414 City od R Cromer d 612 d Road Hertford h R Hyde Ln Green g Broadwater Hertingfordbury London Rd A1081 u 641 North Gascoyne school days only ro Peartree Way o High St b n Hall Grove ta HCC County Hall S Ho s Birch Green Hertford wland Cole Bullocks Lane Heath en Ln Stanborough Chequers Gre New QEII Green Sandridge rs Lakes Rd Ware pe Hospital London Rd oo C Mill tford Rd Cavan Drive Hatfield Ave Green Her St Albans Rd Jersey Farm Tesco Sandringham -

Somerset, England
Fleet Lists - Somerset, England This is our list of current open top buses in Somerset, England BATH - Bath Bus Company Ltd. (City Sightseeing Bath / Tootbus) [RATP Dev / Extrapolitan Sightseeing Group] Buses used for sightseeing tours under the Tootbus brand or City Sightseeing franchise. Fleet List FLEET NO REG NO CHASSIS / BODY LAYOUT LIVERY PREVIOUS KNOWN OWNER(S) 272 EU05 VBG (w) Volvo B7L / Ayats Bravo 1 City PO55/24F BATH NAVIGATOURS / BATH BUS COMPANY (red & black with large white New as part open top, 5/05 Tudor rose) 273 EU05 VBJ (w) Volvo B7L / Ayats Bravo 1 City PO55/24F Bath CitySightseeing / BATH BUS COMPANY (red with yellow flash) New as part open top, 5/05 274 EU05 VBK (w) Volvo B7L / Ayats Bravo 1 City PO55/24F CitySightseeing / BATH BUS COMPANY (red & black) New as part open top, 6/05 301 PN10 FNR Volvo B9TL / Optare Visionaire O51/31F CitySightseeing Bath (red with yellow flash and multicoloured graphics) (withdrawn, Transferred from Windsor to Bath, 2/18; transferred c.2/18) from Bath to Windsor, ?/14; new as open top, 4/10 374 EU05 VBM (w) Volvo B7L / Ayats Bravo 1 City O55/24F BATH BUS COMPANY SIGHTSEEING Serving Bath Since 1997 (red/cream) New as open top, 7/05 381 EU04 CPV (w) Volvo B7L / Ayats Bravo 1 City O55/24F Bath CitySightseeing / BATH BUS COMPANY (red with yellow flash) New as open top, 6/04 617 LJ07 XEU Volvo B9TL / East Lancs Visionaire PO49/31F Bath CitySightseeing (red with yellow flash & multicoloured graphics) Original London Sightseeing Tour Ltd. -

How We Support Britain's Economy and Communities
How we support Britain’s economy and communities stagecoach.com We carry We employ almost 24,000 people around 2.5 Welcome million customers a day Our transport services play a vital role in keeping Britain moving We operate 8,300 buses, coaches and trams For four decades, Stagecoach transport services have The new research carried out by Cebr has now also revealed transported billions of people, helped to build strong local the wider transport benefits associated with Stagecoach, which economies and provided a greener way to travel. As the demonstrate how we contribute towards making the nation more UK’s biggest bus and coach operator, our operations serve active, delivering cleaner air, reducing congestion on our roads communities in major cities including London, Manchester, and making our communities safer. Liverpool, Newcastle, Hull, Sheffield, Oxford and Cambridge * as well as inter-urban and rural locations, such as Cumbria Stagecoach internal data and Lincolnshire. We connect people with jobs, skills and training, bring customers to our high streets and draw families, friends For over 25 years Cebr has supplied We create vital and communities together, supporting the country’s independent economic forecasting and Jobs economic growth and reducing social deprivation. analysis to hundreds of private firms Our economic impact employment and public organisations. Cebr was This new report published by Stagecoach and the commissioned by Stagecoach Group Centre for Economics and Business Research (Cebr) to assess the economic and social contribution of its We pay our way …that’s analyses the significant impact that Stagecoach makes, not transport services to the UK economy. -

Doing Transport Differently
Doing Transport Differently How to access public transport – a guide for everyone with lived experience of disabilty or health conditions Doing Transport Differently How to access public transport – a guide for everyone with lived experience of disabilty or health conditions Doing Transport Differently How to access public transport – a guide for everyone with lived experience of disabilty or health conditions How to use this guide Where should I start? This guide is aimed at people with If you’re not yet using public transport lived experience of disability or health for whatever reason and want to know conditions and at those advising or what’s possible, go to section two. working with them. Using a question For an overview of the law as it relates and answer approach to enable different to transport, go to section two. people with different travel needs to dip To begin planning a journey, short or into it in different ways, it will show you long, go to section three. how far access to public transport has For information and advice on using improved and how to make use of it. buses or coaches, go to section four. For information and advice on using trains, go to section five. For information and advice on underground trains, go to section six. For information and advice on light rail and tramways, ferries and other forms of transport, go to section seven. The resources section includes both useful websites and useful phone numbers to keep with you when you travel. 2 Contents Contents Foreword – Genevieve Barr 6 Foreword – Sir Bert Massie -
A Green Bus for Every Journey
A Green Bus For Every Journey Case studies showing the range of low emission bus technologies in use throughout the UK European engine Bus operators have invested legislation culminating significant sums of money and in the latest Euro VI requirements has seen committed time and resources the air quality impact of in working through the early new buses dramatically challenges on the path to improve but, to date, carbon emissions have not been successful introduction. addressed in bus legislation. Here in Britain, low carbon Investment has been made in new bus technologies and emission buses have been under refuelling infrastructure, and even routing and scheduling development for two decades or have been reviewed in some cases to allow trials and more, driven by strong Government learning of the most advanced potential solutions. policy. Manufacturers, bus operators A number of large bus operators have shown clear and fuel suppliers are embracing leadership by embedding low carbon emission buses into the change, aware that to maintain their sustainability agenda to drive improvements into the their viability, buses must be amongst environmental performance of their bus fleet. the cleanest and most carbon-efficient vehicles on the road. Almost 4,000 There have, of course, been plenty of hurdles along the Low Carbon Emission Buses (LCEB) are way; early hybrid and electric buses experienced initial now operating across the UK, with 40% of reliability issues like any brand new technology, but buses sold in 2015 meeting the low carbon through open collaboration the technology has rapidly requirements. These buses have saved over advanced and is now achieving similar levels of reliability 55,000 tonnes of greenhouse gas emissions as that employed in gas buses and conventional diesel (GHG) per annum compared with the equivalent buses, with warranties extending and new business number of conventional diesel buses. -

On Stage Issue
The newsletter of Stagecoach Group Issue 110 | July 2015 STAGE ON page 2 page 6 INSIDE Memorial award | Greener together megabus.com continues European expansion megabus.com has revealed record advance ticket sales on its new network of domestic coach services in Italy as well as launching two new international routes. More than 30,000 customers purchased tickets during the first week of sales in Italy – higher than the initial sales on any of the company’s other networks in Europe. megabus.com services now link 13 destinations across Italy and passengers have been snapping up bargain fares from just €1 (plus 50 cents booking fee). The major new network of inter-city coach services covers Rome, Milan, Florence, Venice, Naples, Turin, Bologna, Verona, Padua, Siena, Genoa, Sarzana (La Spezia) and Pisa. megabus.com has also created around 100 new jobs through the opening of new bases near Milan megabus.com vehicles at the launch of the new Italian domestic network in Florence and in Florence. In addition, megabus.com recently launched its first base in France, where it has created 35 jobs between London and Milan via Lille, Paris, Lyon from customers has been fantastic. at a depot located near Lyon, from which a new and Turin. “The new routes between London and Milan, and international route now operates between megabus.com Managing Director Edward between Barcelona and Cologne are great news Barcelona, Perpignan, Montpellier, Avignon, Lyon, Hodgson said: “These latest routes mark even for our customers who now have access to even Mulhouse, Freiburg, Karlsruhe, Heidelberg, more expansion of our services in Europe.