Macula Society Imaging Cases for 2012 MONDAY , J UNE 11, 2012 Imaging and Case Study Conference
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Read PDF Edition
THE MEDICARE APPEALS PROCESS P. 16 • RESEARCH BRIEFS P. 60 OCTA AND GLAUCOMA P. 62 • THE LATEST TECHNOLOGY AND DRUGS P. 70 WILLS EYE RESIDENT CASE SERIES P. 77 Review of Ophthalmology Vol. XXV, No. 5 • May 2019 • Charting Your Own Course • The Questionable Cataract • EHR Glaucoma Own Course • The Issues • Uveitic 2019 • Charting Your No. 5 • May Review of Ophthalmology Vol. XXV, MAMAYY 22019019 reviewofophthalmology.comreviewofophthalmology.com CHARTING YOUR OWN COURSE Experts share tips on how to go solo, but note that there are many challenges to overcome as well. P. 20 ALSO INSIDE: • EHR: Room for Improvement? P. 32 • The Questionable Cataract: Who Decides? P. 40 • How to Manage Uveitic Glaucoma P. 48 • Strong Moves for Weak Zonules P. 54 001_rp0519_fc.indd 1 4/16/19 10:03 AM +3.25 D RP0519_J & J Surgical.indd 1 4/5/19 9:57 AM REVIEW NEWS Volume XXV • No. 5 • May 2019 Calcium Intake and Age- Related Macular Degeneration In a recently published study, a secondary the association between calcium in- analysis of patients enrolled in the take and AMD have produced mixed Age-Related Eye Disease Study was results. Findings from the Blue conducted to determine whether an Mountains Eye Study show that Emily Chew, MD Emily Chew, association exists between dietary and calcium may be an important factor supplementary calcium intake and in limiting AMD development/pro- age-related macular degeneration. gression.1 Conversely, fi ndings from Emily Chew, MD, director of the di- the Nutrition Examination Survey vision of epidemiology and clinical ap- suggest that increased calcium in- plications at the National Eye Institute take is harmful in terms of macular at the National Institutes of Health, degeneration.2 However, Dr. -
Emily Y. Chew, M.D
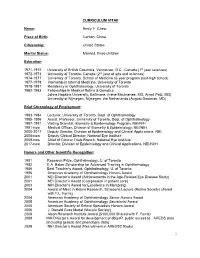
CURRICULUM VITAE Name: Emily Y. Chew Place of Birth: Canton, China Citizenship: United States Marital Status: Married, three children Education 1971-1972 University of British Columbia, Vancouver, B.C., Canada (1st year sciences) 1972-1973 University of Toronto, Canada (2nd year of arts and sciences) 1974-1977 University of Toronto, School of Medicine (6-year program post-high school) 1977-1978 Internship in Internal Medicine, University of Toronto 1978-1981 Residency in Ophthalmology, University of Toronto 1982-1983 Fellowships in Medical Retina & Genetics Johns Hopkins University, Baltimore, (Irene Maumenee, MD, Arnall Patz, MD) University of Nijmegen, Nijmegen, the Netherlands (August Deutman, MD) Brief Chronology of Employment: 1983-1984 Lecturer, University of Toronto, Dept. of Ophthalmology 1985-1986 Assist. Professor, University of Toronto, Dept. of Ophthalmology 1987-1991 Visiting Scientist, Biometry & Epidemiology Program, NEI/NIH 1991-now Medical Officer, Division of Biometry & Epidemiology, NEI/NIH 2000-2017 Deputy Director, Division of Epidemiology and Clinical Applications, NEI. 2008-now Deputy Clinical Director, National Eye Institute 2009-now Chief of Clinical Trials Branch, National Eye Institute 2017-now Director, Division of Epidemiology and Clinical Applications, NEI/NIIH Honors and Other Scientific Recognition: 1981 Research Prize, Ophthalmology, U. of Toronto 1982 E.A. Baker Scholarship for Advanced Training in Ophthalmology 1986 Best Teacher’s Award, Ophthalmology, U. of Toronto 1996 American Academy of Ophthalmology Honors Award 2001 NEI Director’s Award (Achievements in the Age-Related Eye Disease Study) 2001 NEI Director’s Award (Compassion in patient care) 2003 NIH Director’s Award for Excellence in Mentoring 2004 Award of Merit in Retina Research, Schepens Lecture (Retina Society) shared with F.L. -
Contributing Lecturers
2019 CONTINUING EDUCATION PROGRAM June 14, 15 & 16 CONTRIBUTING LECTURERS Emily Chew, MD Emily Chew is the Director of the Division of Epidemiology and Clinical Applications (DECA), at the National Eye Institute, the National Institutes of Health in Bethesda, Maryland. She is also the Chief of the Clinical Trials Branch. Emily received her medical degree and her ophthalmology training at the U. of Toronto, School of Medicine, in Toronto, Canada. She completed her fellowship in Medical Retina at the Wilmer Eye Institute, the Johns Hopkins Medical Institutes and the U. of Nijmegen, the Netherlands Her research interest includes designing and conducting phase I/II clinical trials and epidemiologic studies in chronic retinovascular diseases such as age-related macular degeneration, diabetic retinopathy, the leading causes of blindness in the US. She also studies rare diseases such as ocular manifestation of von Hippel-Lindau Disease and others. She works extensively in large multi-centered trials headed by the staff of DECA including the diabetic studies, the Age-Related Eye Disease Study and the Age-Related Eye Disease Study 2, which she chairs. She also chairs the Actions to Control Cardiovascular Risk in Diabetes (ACCORD) Eye Study in participants with type 2 diabetes, working in collaboration with NHLBI and NIDDK colleagues. Emily Chew is the director of the clinical program in the Macular Telangiectasia Project (Mac Tel Project) which is an international study conducted in 22 clinics in 7 countries along with four basic science laboratories. She chairs the current international study, known as the AMD Ryan Initiative Study (ARIS), which evaluates the natural course of early AMD. -

The Evolving Management of Diabetic Retinopathy: Lessons from Wisconsin and Beyond
The Evolving Management of Diabetic Retinopathy: Lessons from Wisconsin and Beyond AuthorBlock: Lloyd P. Aiello1,2 1Joslin Diabetes Center, Boston, Massachusetts, United States; 2Ophthalmology, Harvard Medical School, Boston, Massachusetts, United States; DisclosureBlock: Lloyd P. Aiello, KalVista Code C (Consultant), KalVista Code I (Personal Financial Interest), Novo Nordisk Code C (Consultant), Optos Code R (Recipient) Presentation Description Less than 50 years ago, diabetic retinopathy was a severe blindng disease with few therapeutic options and often poor outcomes. The advent of laser photocoagulation ushered in a new era where severe visual loss from proliferative diabetic retinopathy (PDR) and diabetic macular edema (DME) could be averted in the majority of patients. However, some degree of visual loss was still frequent and laser photocoagulation destroyed areas of retina leading to side effects and complications. The discovery that VEGF played a central role in both PDR and DME led to development of VEGF inhibitors and a revolution in the care of diabetic eye disease. As a result, visual loss was further reduced, previously unseen magnitudes of visual improvement were realized, and amelioration nonproliferative diabetic retinopathy severity was also observed. The clinical benefit in various patient cohorts and therapeutic differences between VEGF inhibitors have also been evaluated. These and numerous other developing therapies contiunue to make the clinical care of diabetic eye disease one of the longest and most rapidly evolving areas in ophthalmology. Throughout these many remarkable advancements, the fundamental robust understanding of the natural history and epidemiology of diabetic retinopathy provided by the Klein's and others have supported and guided the many clinical trial evaluations of these therapies. -

Print This Issue
January 2011 National Institutes of Health • Department of Health and Human Services • newsinhealth.nih.gov Inside News: 3 Protein Shapes... 4 Dialysis and Kidney Patients... College Drinking... Dietary Supplements Your Aging Eyes “You might find you’re holding your book farther away to read it. You How You See as Time Goes By might even start thinking your arms You may barely notice the changes just aren’t long enough,” says Dr. at first. Maybe you’ve found Emily Chew, a clinical researcher at yourself reaching more NIH’s National Eye Institute. “A good often for your glasses to and simple treatment for presbyopia see up close. You might is reading glasses.” have trouble adjusting to Cloudy areas in the lens, called glaring lights or reading cataracts, are another common eye when the light is dim. You problem that comes with age. may even have put on blue More than 22 million Ameri- socks thinking they were cans have cataracts. By age black. These are some of 80, more than half of us the normal changes to will have had them. Some your eyes and vision as cataracts stay small and have you age. little effect on eyesight, but As more Americans others become large and head toward retirement interfere with vision. Symp- and beyond, scientists toms include blurriness, expect the number of people with of disability in older adults,” says Dr. difficulty seeing well at night, lights age-related eye problems to rise Cynthia Owsley, an eye researcher at that seem too bright and faded color dramatically. You can’t prevent all the University of Alabama at Birming- vision. -

ARMD from Spinach to Injection
1/19/17 Risk Factors determined by the Mayo Clinic • Age. Your risk of macular degeneraon increases as you age, especially aer age 50. Macular ARMD degeneraon is most common in people older than 65. • Family history of macular degenera6on. If someone in your family had macular degeneraon, you're more likely to develop macular degeneraon. From Spinach to Injec9on • Race. Macular degeneraon is more common in whites (Caucasians) than it is in other races. • Smoking. Smoking cigareTes increases your risk of macular degeneraon. • Obesity. Being severely overweight increases the chance that early or intermediate macular degeneraon will progress to the more severe form of the disease. • Diet. A diet that includes few fruits and vegetables may increase the risk of macular degeneraon. • High blood pressure. Diseases that affect the circulatory system, such as high blood pressure or high cholesterol, may increase the risk of macular degeneraon. Steven M. Newman, O.D., C.N.S. • Inflammaon. Your immune system can cause swelling of your body 9ssues, which may Board Cer9fied Optometric Physician increase the risk of macular degeneraon. Florida Board of Optometry • Cardiovascular disease. If you have had diseases that affected your heart and blood vessels (cardiovascular disease), you may be at higher risk of macular degeneraon Board Cer9fied Nutri9on Specialist American College of Nutri8on ARMD gene9cs Hippocrates – Alternate complement pathway – ARMS2/HTRA1 – HDL cholesterol pathway “He who does not know – Extracellular matrix – Angiogenesis pathway food, how can he – Vitamin D pathway understand the diseases of man?” 1 1/19/17 Our body was designed to absorb nutrients the old fashioned way…by eang natural foods rich in an9oxidants. -

Resources-Doctor-AMD-AREDS2
Resources-Doctor-AMD-AREDS2 Study Title: Lutein + Zeaxanthin and Omega-3 Fatty Acids for Age-Related Macular Degeneration Study Authors(s): National Eye Institute/National Institute of Health, Lead Investigator: Dr. Emily Chew Journal: Journal of American Medical Association May 15, 2013 – Vol 309, No. 19 Sponsor: NEI/NIH, Study Meds were provided by Alcon, Bausch & Lomb, DSM and Pfizer Study Objective: 1. To determine whether adding lutein + Zeaxanthin decreases the risk of developing advanced AMD 2. To determine whether DHA + EPA decreases the risk of developing advanced AMD 3. To determine whether Lutein + Zeaxanthin + EPA + DHA decreases the risk of developing advanced AMD 4. Evaluate the effect of eliminating beta carotene from the AREDS formulation 5. Evaluate the effect of lowering zinc doses in the AREDS formulation • Design and Participants: Multi-center, randomized, double-masked, placebo-controlled phase 3 study 4203 participants aged 50 to 85 years at risk for progression to advanced AMD with bilateral large drusen or large drusen in 1 eye and advanced AMD in the fellow eye • Study Design: Participants were randomized to receive: 1. Lutein (10mg) + Zeaxanthin (2mg) 2. DHA (350mg) + EPA (650mg) 3. Lutein + Zeaxanthin + EPA + DHA 4. Placebo All Participants took one of the following: 1. Original AREDS formulation 2. Original AREDS formulation eliminating Beta-Carotene 3. Original AREDS formula with lowered zinc 25mg 4. Original AREDS formula without Beta-Carotene and lowered zinc Primary Outcome: Development of advanced AMD. The unit of analyses used was by eye. Results: Median follow-up was 5 years with 1940 study eyes. • 31% Progression to advanced AMD for placebo • 29% progression to advanced AMD for Lutein + Zeaxanthin • 31% progression to advanced AMD for DHA+EPA • 30% progression to advanced AMD for Lutein + Zeaxanthin + DHA+EPA • Null effect of beta carotene elimination or lower-dose zinc on progression to advanced AMD. -
No Slide Title
Use of Antioxidant Vitamins and Minerals in Age-Related Eye Diseases Emily Chew, M.D. National Eye Institute/National Institutes of Health Age-Related Eye Diseases Cataract AMD Sclera Retina Cornea Macula Iris Lens Cortical Cataract Normal Retina Macula Advanced AMD Neovascular AMD or Central Geographic Atrophy Importance of potential prevention age-related cataract & macular degeneration with vitamins/mineral Cataract Surgery • highly successful, huge expense Age-related macular degeneration • lack of successful treatment for the majority of cases (atrophic) Rationale for use of vitamins in age-related cataract & macular degeneration Oxidative stress • generated through photo oxidation and metabolic processes • results in reactive oxygen intermediates: free radicals, hydrogen peroxide, or singlet oxygen Rationale for use of vitamins in age-related cataract & macular degeneration • Data from animal models, in vitro experiments • Observational human data • Controlled clinical trials Studies of Cataract and Nutrition Observational studies • Cross-sectional studies • Case-control studies Controlled clinical trials Cataract: Observational Studies Cross-Sectional Studies Baltimore Longitudinal Study on Aging Nutritional Factors in Eye Disease Study Beaver Dam Eye Study Inconsistent associations with vitamins Cataract: Observational Studies Case-Control Studies of Vitamin Use India-US Case Control Study of Cataract Plasma antioxidant index (protective) Lens Opacities Case-Control Study Dietary C,E, and carotene (protective) Italian American -

Brief BIO Sketch.4.2013.Photo
Brief BIO sketch: Emily Y. Chew, M.D. Emily Chew is the Deputy Director of the Division of Epidemiology and Clinical Applications (DECA), at the National Eye Institute, the National Institutes of Health in Bethesda, Maryland. She is also the Chief of the Clinical Trials Branch within the Division. Emily completed a 6-year combined undergraduate and medical degree. She received her medical degree and her ophthalmology training at the U. of Toronto, School of Medicine, in Toronto, Canada. She completed her fellowship in Medical Retina at the Wilmer Eye Institute, the Johns Hopkins Medical Institutes and the U. of Nijmegen, the Netherlands, in medical retina. Her research interest includes phase I/II clinical trials and epidemiologic studies in retinovascular diseases such as age-related macular degeneration, diabetic retinopathy, ocular diseases of von Hippel-Lindau Disease and others. She worked extensively in large multi-centered trials headed by the staff of DECA including the Early Treatment Diabetic Retinopathy Study, the Age-Related Eye Disease Study and the Age-Related Eye Disease Study 2, which she chairs. She also chairs the Actions to Control Cardiovascular Risk in Diabetes (ACCORD) Eye Study in participants with type 2 diabetes, working in collaboration with colleagues at the National Heart, Lung, and Blood Institute/NIH. Emily is also the director of the clinical program in the Macular Telangiectasia Project (Mac Tel Project) which is an international study conducted in 22 clinics in 7 countries along with 4 basic science laboratories. Emily is also the director of the medical retina fellowship at the NEI. Along with the team in the Clinical Trials Branch, she provides the clinical training as well as education in conducting clinical trials. -

The Meet Our New Doctors
the LIGHT 2013 Fall PIPE IN THIS ISSUE: Making the Switch pg. 4-6 Meet our WOA! pg. 6 new Doctors The Results are in pg. 7-8 Diagnostic Dilemma pg. 9-11 pg. 2-3 THE NEWSLETTER OF The next issue of the Light Pipe will be digital. If Georgia Retina does not have your current email on file, please go to garetina.com/light-pipe-newsletter and fill out the form or call us at 404-255-9096. Meet Our New Doctors treatments for macular degeneration, diabetic retinopathy, optical coherence tomography, retinal vascular disease, cystoid macular edema, and the management of complicated retinal detachments. He has also been a sub- investigator in more than twenty clinical trials. He is a member of the American Academy of Ophthalmology, the Association for Research in Vision and Ophthalmology, and the American Society of Retina Specialists. In his spare time, he enjoys playing sports, breakdancing, snowboarding and spending time with his family, especially his baby niece Aubrey. Hyung Cho, M.D. Dr. Cho practices at the Georgia Retina offices in Conyers and Stockbridge. Dr. Cho, a board-certified ophthalmologist, graduated with honors from Dartmouth College. He completed his medical school and ophthalmology residency at the Albert Einstein Krishna Mukkamala, M.D. College of Medicine and Montefiore Medical Center in New York City. He was elected to Dr. Krishna Mukkamala grew up in Virginia serve as Chief Resident during his final year of Beach, VA where he was valedictorian at an residency. He went on to complete a two-year International Baccalaureate high school and medical and surgical retina fellowship at Tufts was active in the local community. -

Mcgill OPHTHALMOLOGY CLINICAL DAY 2017 Medical And
McGill University Department of Ophthalmology McGILL OPHTHALMOLOGY CLINICAL DAY 2017 Medical and Surgical Retina Intercontinental Hotel 360, rue St. Antoine West Montreal, Quebec Friday, June 2, 2017 Organizing Committee: Hady Saheb, MD, MPH, Chair, McGill Clinical Day Jill Rothberg, Senior Administrative Coordinator Scientific Committee: Leonard A. Levin, MD, PhD, FRCSC, Chair, McGill Department of Ophthalmology Mahshad Darvish, MDCM, MBA, FRCSC John Galic, MD, FRCSC Événement durable McGill McGill Sustainable Event Bronze Certification Cette activité s'adresse aux médecins ophtalmologistes, résidents en ophtalmologie, et étudiants en médecine. La présente activité est une activité de formation collective agréée (section 1) au sens que lui donne le programme de Maintien du certificat (MDC) du Collège royal des médecins et chirurgiens du Canada, approuvée par la direction du Développement professionnel continu (DDPC) de la Fédération des médecins spécialistes du Québec. Vous pouvez déclarer un maximum de 7,80 heures pour l’activité globale. Les crédits sont calculés automatiquement dans MAINPORT. Une participation à cette activité donne droit à une attestation de présence. Les participants doivent réclamer un nombre d’heures conforme à la durée de leur participation. En vertu d'une entente conclue entre le Collège royal des médecins et chirurgiens du Canada et l'American Medical Association (AMA), les médecins peuvent convertir les crédits obtenus au titre du programme de MDC du Collège royal en crédits de catégorie 1 de l'AMA PRAMC. Vous trouverez l'information sur le processus de conversion des crédits du programme de MDC du Collège royal en crédits de l'AMA à l’adresse www.ama-assn.org/go/internationalcme Cette activité de formation est admissible aux allocations de ressourcement prévues à l’annexe 44. -

Ophthalmology Education
FROM THE CHAIR 2016 Educational Program Highlights Ophthalmology Education REGULARLY RECURRING EVENTS 2016 CONFERENCES AND EVENTS Mondays 7 am Weekly Difficult Case Review Conference Dear Colleagues, 7 am Weekly Vitreoretinal Case Discussion Tuesdays 8 am Weekly Electroretinogram and Electrophysiology Case Review I am proud to introduce our 10 am Glaucoma Research Conference (Monthly: 1st Tuesday) department’s calendar of 8 am Comparative Ocular Pathology Rounds educational conferences and Wednesdays (2x Monthly: 2nd, 4th Wednesday) events. The rapidly changing landscape of vision care and science involves 7 am Weekly Grand Rounds discovering and adopting new technologies, diagnostics, procedures and Fridays 8 am Weekly Retina Workout therapeutics to address eye disease. SPECIAL CONFERENCES AND EVENTS With the ultimate goal of improving vision-related quality of life, our highly January 22, 2016 Visiting Professor Brian Link, PhD, Medical College of Wisconsin accomplished clinical and research faculty create and share relevant Visiting Professor Julian Perry, MD, Cleveland Clinic; and information with diverse audiences. Topics range from basic medical February 26, 2016 Conference: Oculoplastics 2016: Updates and Pearls knowledge to vision research on the edge of imaginable. This overview Spring Vision Science Research Symposium with Keynote Speaker represents a sampling of our programs for medical students, residents, April 1, 2016 Dale Gregerson, PhD, University of Minnesota fellows, scientists-in-training, allied health professionals, practitioners, April 21, 2016 Saving Sight Session: Telemedicine, Yao Liu, MD basic scientists, patients and friends. McPherson Endowed Lecture, Keynote Speaker Pawan Sinha, PhD, April 28, 2016 Welcome! Please join us for a conference or event in the near future. Massachusetts Institute of Technology Visiting Professor Kathryn Colby, MD, PhD, Chair, Department May 27, 2016 of Ophthalmology and Visual Sciences, University of Chicago Visiting Professor Joseph Carroll, PhD, FARVO, Advanced Ocular June 3, 2016 Terri L.