Effect of Omega-3 Fatty Acids, Lutein/Zeaxanthin, Or Other Nutrient
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Read PDF Edition
THE MEDICARE APPEALS PROCESS P. 16 • RESEARCH BRIEFS P. 60 OCTA AND GLAUCOMA P. 62 • THE LATEST TECHNOLOGY AND DRUGS P. 70 WILLS EYE RESIDENT CASE SERIES P. 77 Review of Ophthalmology Vol. XXV, No. 5 • May 2019 • Charting Your Own Course • The Questionable Cataract • EHR Glaucoma Own Course • The Issues • Uveitic 2019 • Charting Your No. 5 • May Review of Ophthalmology Vol. XXV, MAMAYY 22019019 reviewofophthalmology.comreviewofophthalmology.com CHARTING YOUR OWN COURSE Experts share tips on how to go solo, but note that there are many challenges to overcome as well. P. 20 ALSO INSIDE: • EHR: Room for Improvement? P. 32 • The Questionable Cataract: Who Decides? P. 40 • How to Manage Uveitic Glaucoma P. 48 • Strong Moves for Weak Zonules P. 54 001_rp0519_fc.indd 1 4/16/19 10:03 AM +3.25 D RP0519_J & J Surgical.indd 1 4/5/19 9:57 AM REVIEW NEWS Volume XXV • No. 5 • May 2019 Calcium Intake and Age- Related Macular Degeneration In a recently published study, a secondary the association between calcium in- analysis of patients enrolled in the take and AMD have produced mixed Age-Related Eye Disease Study was results. Findings from the Blue conducted to determine whether an Mountains Eye Study show that Emily Chew, MD Emily Chew, association exists between dietary and calcium may be an important factor supplementary calcium intake and in limiting AMD development/pro- age-related macular degeneration. gression.1 Conversely, fi ndings from Emily Chew, MD, director of the di- the Nutrition Examination Survey vision of epidemiology and clinical ap- suggest that increased calcium in- plications at the National Eye Institute take is harmful in terms of macular at the National Institutes of Health, degeneration.2 However, Dr. -
Emily Y. Chew, M.D
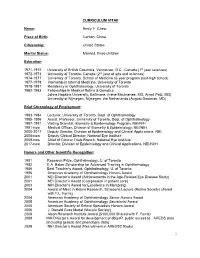
CURRICULUM VITAE Name: Emily Y. Chew Place of Birth: Canton, China Citizenship: United States Marital Status: Married, three children Education 1971-1972 University of British Columbia, Vancouver, B.C., Canada (1st year sciences) 1972-1973 University of Toronto, Canada (2nd year of arts and sciences) 1974-1977 University of Toronto, School of Medicine (6-year program post-high school) 1977-1978 Internship in Internal Medicine, University of Toronto 1978-1981 Residency in Ophthalmology, University of Toronto 1982-1983 Fellowships in Medical Retina & Genetics Johns Hopkins University, Baltimore, (Irene Maumenee, MD, Arnall Patz, MD) University of Nijmegen, Nijmegen, the Netherlands (August Deutman, MD) Brief Chronology of Employment: 1983-1984 Lecturer, University of Toronto, Dept. of Ophthalmology 1985-1986 Assist. Professor, University of Toronto, Dept. of Ophthalmology 1987-1991 Visiting Scientist, Biometry & Epidemiology Program, NEI/NIH 1991-now Medical Officer, Division of Biometry & Epidemiology, NEI/NIH 2000-2017 Deputy Director, Division of Epidemiology and Clinical Applications, NEI. 2008-now Deputy Clinical Director, National Eye Institute 2009-now Chief of Clinical Trials Branch, National Eye Institute 2017-now Director, Division of Epidemiology and Clinical Applications, NEI/NIIH Honors and Other Scientific Recognition: 1981 Research Prize, Ophthalmology, U. of Toronto 1982 E.A. Baker Scholarship for Advanced Training in Ophthalmology 1986 Best Teacher’s Award, Ophthalmology, U. of Toronto 1996 American Academy of Ophthalmology Honors Award 2001 NEI Director’s Award (Achievements in the Age-Related Eye Disease Study) 2001 NEI Director’s Award (Compassion in patient care) 2003 NIH Director’s Award for Excellence in Mentoring 2004 Award of Merit in Retina Research, Schepens Lecture (Retina Society) shared with F.L. -

Identification of Distinct Ph- and Zeaxanthin-Dependent Quenching
RESEARCH ARTICLE Identification of distinct pH- and zeaxanthin-dependent quenching in LHCSR3 from Chlamydomonas reinhardtii Julianne M Troiano1†, Federico Perozeni2†, Raymundo Moya1, Luca Zuliani2, Kwangyrul Baek3, EonSeon Jin3, Stefano Cazzaniga2, Matteo Ballottari2*, Gabriela S Schlau-Cohen1* 1Department of Chemistry, Massachusetts Institute of Technology, Cambridge, United States; 2Department of Biotechnology, University of Verona, Verona, Italy; 3Department of Life Science, Hanyang University, Seoul, Republic of Korea Abstract Under high light, oxygenic photosynthetic organisms avoid photodamage by thermally dissipating absorbed energy, which is called nonphotochemical quenching. In green algae, a chlorophyll and carotenoid-binding protein, light-harvesting complex stress-related (LHCSR3), detects excess energy via a pH drop and serves as a quenching site. Using a combined in vivo and in vitro approach, we investigated quenching within LHCSR3 from Chlamydomonas reinhardtii. In vitro two distinct quenching processes, individually controlled by pH and zeaxanthin, were identified within LHCSR3. The pH-dependent quenching was removed within a mutant LHCSR3 that lacks the residues that are protonated to sense the pH drop. Observation of quenching in zeaxanthin-enriched LHCSR3 even at neutral pH demonstrated zeaxanthin-dependent quenching, which also occurs in other light-harvesting complexes. Either pH- or zeaxanthin-dependent quenching prevented the formation of damaging reactive oxygen species, and thus the two *For correspondence: quenching processes may together provide different induction and recovery kinetics for [email protected] (MB); photoprotection in a changing environment. [email protected] (GSS-C) †These authors contributed equally to this work Competing interests: The Introduction authors declare that no Sunlight is the essential source of energy for most photosynthetic organisms, yet sunlight in excess competing interests exist. -

Identification of 1 Distinct Ph- and Zeaxanthin-Dependent Quenching in LHCSR3 from Chlamydomonas Reinhardtii
Identification of 1 distinct pH- and zeaxanthin-dependent quenching in LHCSR3 from chlamydomonas reinhardtii The MIT Faculty has made this article openly available. Please share how this access benefits you. Your story matters. Citation Troiano, Julianne M. et al. “Identification of 1 distinct pH- and zeaxanthin-dependent quenching in LHCSR3 from chlamydomonas reinhardtii.” eLife, 10 (January 2021): e60383 © 2021 The Author(s) As Published 10.7554/eLife.60383 Publisher eLife Sciences Publications, Ltd Version Final published version Citable link https://hdl.handle.net/1721.1/130449 Terms of Use Creative Commons Attribution 4.0 International license Detailed Terms https://creativecommons.org/licenses/by/4.0/ RESEARCH ARTICLE Identification of distinct pH- and zeaxanthin-dependent quenching in LHCSR3 from Chlamydomonas reinhardtii Julianne M Troiano1†, Federico Perozeni2†, Raymundo Moya1, Luca Zuliani2, Kwangyrul Baek3, EonSeon Jin3, Stefano Cazzaniga2, Matteo Ballottari2*, Gabriela S Schlau-Cohen1* 1Department of Chemistry, Massachusetts Institute of Technology, Cambridge, United States; 2Department of Biotechnology, University of Verona, Verona, Italy; 3Department of Life Science, Hanyang University, Seoul, Republic of Korea Abstract Under high light, oxygenic photosynthetic organisms avoid photodamage by thermally dissipating absorbed energy, which is called nonphotochemical quenching. In green algae, a chlorophyll and carotenoid-binding protein, light-harvesting complex stress-related (LHCSR3), detects excess energy via a pH drop and serves as a quenching site. Using a combined in vivo and in vitro approach, we investigated quenching within LHCSR3 from Chlamydomonas reinhardtii. In vitro two distinct quenching processes, individually controlled by pH and zeaxanthin, were identified within LHCSR3. The pH-dependent quenching was removed within a mutant LHCSR3 that lacks the residues that are protonated to sense the pH drop. -
Contributing Lecturers
2019 CONTINUING EDUCATION PROGRAM June 14, 15 & 16 CONTRIBUTING LECTURERS Emily Chew, MD Emily Chew is the Director of the Division of Epidemiology and Clinical Applications (DECA), at the National Eye Institute, the National Institutes of Health in Bethesda, Maryland. She is also the Chief of the Clinical Trials Branch. Emily received her medical degree and her ophthalmology training at the U. of Toronto, School of Medicine, in Toronto, Canada. She completed her fellowship in Medical Retina at the Wilmer Eye Institute, the Johns Hopkins Medical Institutes and the U. of Nijmegen, the Netherlands Her research interest includes designing and conducting phase I/II clinical trials and epidemiologic studies in chronic retinovascular diseases such as age-related macular degeneration, diabetic retinopathy, the leading causes of blindness in the US. She also studies rare diseases such as ocular manifestation of von Hippel-Lindau Disease and others. She works extensively in large multi-centered trials headed by the staff of DECA including the diabetic studies, the Age-Related Eye Disease Study and the Age-Related Eye Disease Study 2, which she chairs. She also chairs the Actions to Control Cardiovascular Risk in Diabetes (ACCORD) Eye Study in participants with type 2 diabetes, working in collaboration with NHLBI and NIDDK colleagues. Emily Chew is the director of the clinical program in the Macular Telangiectasia Project (Mac Tel Project) which is an international study conducted in 22 clinics in 7 countries along with four basic science laboratories. She chairs the current international study, known as the AMD Ryan Initiative Study (ARIS), which evaluates the natural course of early AMD. -

Level of Xanthophyll, Lutein and Zeaxanthin in Selected Thai Fruits Determined by HPLC
2012 International Conference on Nutrition and Food Sciences IPCBEE vol. 39 (2012) © (2012) IACSIT Press, Singapore Level of Xanthophyll, Lutein and Zeaxanthin in Selected Thai Fruits Determined by HPLC Nittaya Khonsarn 1 and Siriporn Lawan 2 1Department of biotechnology, Faculty of Technology, Mahasarakham University, Thailand 2 Department of Food technology, Faculty of Technology, Mahasarakham University, Thailand Abstract. In this study 12 selected Thai summer fruits were determined xanthophyll, lutein and zeaxanthin content by high performance liquid chromatography (HPLC). The result shown that there were xanthophyll in 11 kinds of selected fruits except banana. The highest of average xanthophyll level was found in cantaloupe (1.31±0.07 mg/100g edible portion), meanwhile barbados cherry was the second (1.18±0.03 mg/100g edible portion). Among fruits analysed, lutein content was the highest in papaya (23.74±0.46 mg/100g edible portion), follow by cantaloupe (21.82±1.60 mg/100g edible portion). Whereas lutein was not detected in star gooseberry, java apple, dragon fruit, guava, salak plum, water melon, banana and satol. Cantaloupe was the highest source of zeaxanthin (1.72±0.07 mg/100g edible portion), zeaxanthin was not however detected in star gooseberry, java apple, dragon fruit, salak plum, banana and satol. These results are suggested that some kinds of summer fruits including papaya and cantaloupe, have potential as rich sources of xanthophyll, lutein and zeaxanthin for consumer health. Keywords: Xanthophyll, Lutein, Zeaxanthin, Thai Fruit, HPLC. 1. Introduction Xanthophyll, lutein and zeaxanthin are some kinds of carotenoid that not only play important role in organic pigments in fruits and vegetables but also important in the prevention of various diseases associated with oxidative stress. -

The Evolving Management of Diabetic Retinopathy: Lessons from Wisconsin and Beyond
The Evolving Management of Diabetic Retinopathy: Lessons from Wisconsin and Beyond AuthorBlock: Lloyd P. Aiello1,2 1Joslin Diabetes Center, Boston, Massachusetts, United States; 2Ophthalmology, Harvard Medical School, Boston, Massachusetts, United States; DisclosureBlock: Lloyd P. Aiello, KalVista Code C (Consultant), KalVista Code I (Personal Financial Interest), Novo Nordisk Code C (Consultant), Optos Code R (Recipient) Presentation Description Less than 50 years ago, diabetic retinopathy was a severe blindng disease with few therapeutic options and often poor outcomes. The advent of laser photocoagulation ushered in a new era where severe visual loss from proliferative diabetic retinopathy (PDR) and diabetic macular edema (DME) could be averted in the majority of patients. However, some degree of visual loss was still frequent and laser photocoagulation destroyed areas of retina leading to side effects and complications. The discovery that VEGF played a central role in both PDR and DME led to development of VEGF inhibitors and a revolution in the care of diabetic eye disease. As a result, visual loss was further reduced, previously unseen magnitudes of visual improvement were realized, and amelioration nonproliferative diabetic retinopathy severity was also observed. The clinical benefit in various patient cohorts and therapeutic differences between VEGF inhibitors have also been evaluated. These and numerous other developing therapies contiunue to make the clinical care of diabetic eye disease one of the longest and most rapidly evolving areas in ophthalmology. Throughout these many remarkable advancements, the fundamental robust understanding of the natural history and epidemiology of diabetic retinopathy provided by the Klein's and others have supported and guided the many clinical trial evaluations of these therapies. -

Print This Issue
January 2011 National Institutes of Health • Department of Health and Human Services • newsinhealth.nih.gov Inside News: 3 Protein Shapes... 4 Dialysis and Kidney Patients... College Drinking... Dietary Supplements Your Aging Eyes “You might find you’re holding your book farther away to read it. You How You See as Time Goes By might even start thinking your arms You may barely notice the changes just aren’t long enough,” says Dr. at first. Maybe you’ve found Emily Chew, a clinical researcher at yourself reaching more NIH’s National Eye Institute. “A good often for your glasses to and simple treatment for presbyopia see up close. You might is reading glasses.” have trouble adjusting to Cloudy areas in the lens, called glaring lights or reading cataracts, are another common eye when the light is dim. You problem that comes with age. may even have put on blue More than 22 million Ameri- socks thinking they were cans have cataracts. By age black. These are some of 80, more than half of us the normal changes to will have had them. Some your eyes and vision as cataracts stay small and have you age. little effect on eyesight, but As more Americans others become large and head toward retirement interfere with vision. Symp- and beyond, scientists toms include blurriness, expect the number of people with of disability in older adults,” says Dr. difficulty seeing well at night, lights age-related eye problems to rise Cynthia Owsley, an eye researcher at that seem too bright and faded color dramatically. You can’t prevent all the University of Alabama at Birming- vision. -

Vitamins a and E and Carotenoids
Fat-Soluble Vitamins & Micronutrients: Vitamins A and E and Carotenoids Vitamins A (retinol) and E (tocopherol) and the carotenoids are fat-soluble micronutrients that are found in many foods, including some vegetables, fruits, meats, and animal products. Fish-liver oils, liver, egg yolks, butter, and cream are known for their higher content of vitamin A. Nuts and seeds are particularly rich sources of vitamin E (Thomas 2006). At least 700 carotenoids—fat-soluble red and yellow pigments—are found in nature (Britton 2004). Americans consume 40–50 of these carotenoids, primarily in fruits and vegetables (Khachik 1992), and smaller amounts in poultry products, including egg yolks, and in seafoods (Boylston 2007). Six major carotenoids are found in human serum: alpha-carotene, beta-carotene, beta-cryptoxanthin, lutein, trans-lycopene, and zeaxanthin. Major carotene sources are orange-colored fruits and vegetables such as carrots, pumpkins, and mangos. Lutein and zeaxanthin are also found in dark green leafy vegetables, where any orange coloring is overshadowed by chlorophyll. Trans-Lycopene is obtained primarily from tomato and tomato products. For information on the carotenoid content of U.S. foods, see the 1998 carotenoid database created by the U.S. Department of Agriculture and the Nutrition Coordinating Center at the University of Minnesota (http://www.nal.usda.gov/fnic/foodcomp/Data/car98/car98.html). Vitamin A, found in foods that come from animal sources, is called preformed vitamin A. Some carotenoids found in colorful fruits and vegetables are called provitamin A; they are metabolized in the body to vitamin A. Among the carotenoids, beta-carotene, a retinol dimer, has the most significant provitamin A activity. -

Vitamin a Compounds in Mothers and Infants at Birth
University of Nebraska Medical Center DigitalCommons@UNMC Theses & Dissertations Graduate Studies Spring 5-7-2016 Vitamin A Compounds in Mothers and Infants at Birth Jenna M. Paseka University of Nebraska Medical Center Follow this and additional works at: https://digitalcommons.unmc.edu/etd Part of the Medical Nutrition Commons Recommended Citation Paseka, Jenna M., "Vitamin A Compounds in Mothers and Infants at Birth" (2016). Theses & Dissertations. 90. https://digitalcommons.unmc.edu/etd/90 This Thesis is brought to you for free and open access by the Graduate Studies at DigitalCommons@UNMC. It has been accepted for inclusion in Theses & Dissertations by an authorized administrator of DigitalCommons@UNMC. For more information, please contact [email protected]. VITAMIN A COMPOUNDS IN MOTHERS AND INFANTS AT BIRTH by Jenna M. Paseka, RD, LMNT A THESIS Presented to the Faculty of the University of Nebraska Graduate College in Partial Fulfillment of the Requirements for the Degree of Master of Science Medical Sciences Interdepartmental Area Graduate Program (Medical Nutrition) Under the Supervision of Professor Corrine K. Hanson University of Nebraska Medical Center Omaha, Nebraska April 2016 Advisory Committee: Ann Anderson Berry, MD Glenda Woscyna, MS With Assistance from: Elizabeth Lyden, MS i ACKNOWLEDGEMENTS I would like to express my sincere appreciation and thanks to my advisor Corrine Hanson. Your expertise and guidance throughout this process has been invaluable to me. The advice and encouragement you provided to me enabled me to strengthen my research abilities and support my journey of completing my thesis. I would also like to extend my gratitude to my committee members Ann Anderson Berry and Glenda Woscyna. -

ARMD from Spinach to Injection
1/19/17 Risk Factors determined by the Mayo Clinic • Age. Your risk of macular degeneraon increases as you age, especially aer age 50. Macular ARMD degeneraon is most common in people older than 65. • Family history of macular degenera6on. If someone in your family had macular degeneraon, you're more likely to develop macular degeneraon. From Spinach to Injec9on • Race. Macular degeneraon is more common in whites (Caucasians) than it is in other races. • Smoking. Smoking cigareTes increases your risk of macular degeneraon. • Obesity. Being severely overweight increases the chance that early or intermediate macular degeneraon will progress to the more severe form of the disease. • Diet. A diet that includes few fruits and vegetables may increase the risk of macular degeneraon. • High blood pressure. Diseases that affect the circulatory system, such as high blood pressure or high cholesterol, may increase the risk of macular degeneraon. Steven M. Newman, O.D., C.N.S. • Inflammaon. Your immune system can cause swelling of your body 9ssues, which may Board Cer9fied Optometric Physician increase the risk of macular degeneraon. Florida Board of Optometry • Cardiovascular disease. If you have had diseases that affected your heart and blood vessels (cardiovascular disease), you may be at higher risk of macular degeneraon Board Cer9fied Nutri9on Specialist American College of Nutri8on ARMD gene9cs Hippocrates – Alternate complement pathway – ARMS2/HTRA1 – HDL cholesterol pathway “He who does not know – Extracellular matrix – Angiogenesis pathway food, how can he – Vitamin D pathway understand the diseases of man?” 1 1/19/17 Our body was designed to absorb nutrients the old fashioned way…by eang natural foods rich in an9oxidants. -

Antioxidant Capacity of Berry Crops, Culinary Herbs and Medicinal Herbs
Antioxidant Capacity of Berry Crops, Culinary Herbs and Medicinal Herbs Shiow Y. Wang Fruit Laboratory, BARC, ARS U. S. Department of Agriculture Beltsville, Maryland 20705, USA Keywords: antioxidants, anthocyanins, carotenoids, flavonoids, phenolics Abstract Herbs and berry crops have been shown to contain high levels of antioxidant compounds. These antioxidants are capable of performing a number of functions including acting as free radical scavengers, peroxide decomposers, singlet and triplet oxygen quenchers, enzyme inhibitors, and synergists. The different antioxidant components found in herbs and berry crops provide protection against harmful free radicals and have been associated with lower incidence and mortality rates of cancer and heart disease, in addition to a number of other health benefits. Herbs have been used for many purposes including medicine, nutrition, flavorings, beverages, and industry. Since prehistoric times, herbs have been the basis for nearly all medicinal therapy until synthetic drugs were developed in the Nineteenth Century. Today herbs are still found in 40 percent of prescription drugs. Culinary herbs also have been grown and used for their ability to enhance and complement the flavors of a wide variety of foods. Even though a variety of herbs are known to be remarkable sources of phenolic compounds, data on the composition and antioxidant activities of herbs and berry crops are insufficient. We found herbs and berry crops to contain a number of healthful phytochemicals such as vitamin E, vitamin C, bata carotene, flavonoids, phenolic acids and are an effective and potential source of natural antioxidants. The results from this presentation will be useful to plant breeders, other researchers, and the general public who are interested in the antioxidant potentials of various herbs and berry crops as dietary supplements.