Mcgill OPHTHALMOLOGY CLINICAL DAY 2017 Medical And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Read PDF Edition
THE MEDICARE APPEALS PROCESS P. 16 • RESEARCH BRIEFS P. 60 OCTA AND GLAUCOMA P. 62 • THE LATEST TECHNOLOGY AND DRUGS P. 70 WILLS EYE RESIDENT CASE SERIES P. 77 Review of Ophthalmology Vol. XXV, No. 5 • May 2019 • Charting Your Own Course • The Questionable Cataract • EHR Glaucoma Own Course • The Issues • Uveitic 2019 • Charting Your No. 5 • May Review of Ophthalmology Vol. XXV, MAMAYY 22019019 reviewofophthalmology.comreviewofophthalmology.com CHARTING YOUR OWN COURSE Experts share tips on how to go solo, but note that there are many challenges to overcome as well. P. 20 ALSO INSIDE: • EHR: Room for Improvement? P. 32 • The Questionable Cataract: Who Decides? P. 40 • How to Manage Uveitic Glaucoma P. 48 • Strong Moves for Weak Zonules P. 54 001_rp0519_fc.indd 1 4/16/19 10:03 AM +3.25 D RP0519_J & J Surgical.indd 1 4/5/19 9:57 AM REVIEW NEWS Volume XXV • No. 5 • May 2019 Calcium Intake and Age- Related Macular Degeneration In a recently published study, a secondary the association between calcium in- analysis of patients enrolled in the take and AMD have produced mixed Age-Related Eye Disease Study was results. Findings from the Blue conducted to determine whether an Mountains Eye Study show that Emily Chew, MD Emily Chew, association exists between dietary and calcium may be an important factor supplementary calcium intake and in limiting AMD development/pro- age-related macular degeneration. gression.1 Conversely, fi ndings from Emily Chew, MD, director of the di- the Nutrition Examination Survey vision of epidemiology and clinical ap- suggest that increased calcium in- plications at the National Eye Institute take is harmful in terms of macular at the National Institutes of Health, degeneration.2 However, Dr. -
Emily Y. Chew, M.D
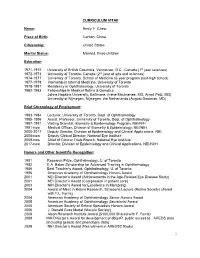
CURRICULUM VITAE Name: Emily Y. Chew Place of Birth: Canton, China Citizenship: United States Marital Status: Married, three children Education 1971-1972 University of British Columbia, Vancouver, B.C., Canada (1st year sciences) 1972-1973 University of Toronto, Canada (2nd year of arts and sciences) 1974-1977 University of Toronto, School of Medicine (6-year program post-high school) 1977-1978 Internship in Internal Medicine, University of Toronto 1978-1981 Residency in Ophthalmology, University of Toronto 1982-1983 Fellowships in Medical Retina & Genetics Johns Hopkins University, Baltimore, (Irene Maumenee, MD, Arnall Patz, MD) University of Nijmegen, Nijmegen, the Netherlands (August Deutman, MD) Brief Chronology of Employment: 1983-1984 Lecturer, University of Toronto, Dept. of Ophthalmology 1985-1986 Assist. Professor, University of Toronto, Dept. of Ophthalmology 1987-1991 Visiting Scientist, Biometry & Epidemiology Program, NEI/NIH 1991-now Medical Officer, Division of Biometry & Epidemiology, NEI/NIH 2000-2017 Deputy Director, Division of Epidemiology and Clinical Applications, NEI. 2008-now Deputy Clinical Director, National Eye Institute 2009-now Chief of Clinical Trials Branch, National Eye Institute 2017-now Director, Division of Epidemiology and Clinical Applications, NEI/NIIH Honors and Other Scientific Recognition: 1981 Research Prize, Ophthalmology, U. of Toronto 1982 E.A. Baker Scholarship for Advanced Training in Ophthalmology 1986 Best Teacher’s Award, Ophthalmology, U. of Toronto 1996 American Academy of Ophthalmology Honors Award 2001 NEI Director’s Award (Achievements in the Age-Related Eye Disease Study) 2001 NEI Director’s Award (Compassion in patient care) 2003 NIH Director’s Award for Excellence in Mentoring 2004 Award of Merit in Retina Research, Schepens Lecture (Retina Society) shared with F.L. -
Contributing Lecturers
2019 CONTINUING EDUCATION PROGRAM June 14, 15 & 16 CONTRIBUTING LECTURERS Emily Chew, MD Emily Chew is the Director of the Division of Epidemiology and Clinical Applications (DECA), at the National Eye Institute, the National Institutes of Health in Bethesda, Maryland. She is also the Chief of the Clinical Trials Branch. Emily received her medical degree and her ophthalmology training at the U. of Toronto, School of Medicine, in Toronto, Canada. She completed her fellowship in Medical Retina at the Wilmer Eye Institute, the Johns Hopkins Medical Institutes and the U. of Nijmegen, the Netherlands Her research interest includes designing and conducting phase I/II clinical trials and epidemiologic studies in chronic retinovascular diseases such as age-related macular degeneration, diabetic retinopathy, the leading causes of blindness in the US. She also studies rare diseases such as ocular manifestation of von Hippel-Lindau Disease and others. She works extensively in large multi-centered trials headed by the staff of DECA including the diabetic studies, the Age-Related Eye Disease Study and the Age-Related Eye Disease Study 2, which she chairs. She also chairs the Actions to Control Cardiovascular Risk in Diabetes (ACCORD) Eye Study in participants with type 2 diabetes, working in collaboration with NHLBI and NIDDK colleagues. Emily Chew is the director of the clinical program in the Macular Telangiectasia Project (Mac Tel Project) which is an international study conducted in 22 clinics in 7 countries along with four basic science laboratories. She chairs the current international study, known as the AMD Ryan Initiative Study (ARIS), which evaluates the natural course of early AMD. -

The Evolving Management of Diabetic Retinopathy: Lessons from Wisconsin and Beyond
The Evolving Management of Diabetic Retinopathy: Lessons from Wisconsin and Beyond AuthorBlock: Lloyd P. Aiello1,2 1Joslin Diabetes Center, Boston, Massachusetts, United States; 2Ophthalmology, Harvard Medical School, Boston, Massachusetts, United States; DisclosureBlock: Lloyd P. Aiello, KalVista Code C (Consultant), KalVista Code I (Personal Financial Interest), Novo Nordisk Code C (Consultant), Optos Code R (Recipient) Presentation Description Less than 50 years ago, diabetic retinopathy was a severe blindng disease with few therapeutic options and often poor outcomes. The advent of laser photocoagulation ushered in a new era where severe visual loss from proliferative diabetic retinopathy (PDR) and diabetic macular edema (DME) could be averted in the majority of patients. However, some degree of visual loss was still frequent and laser photocoagulation destroyed areas of retina leading to side effects and complications. The discovery that VEGF played a central role in both PDR and DME led to development of VEGF inhibitors and a revolution in the care of diabetic eye disease. As a result, visual loss was further reduced, previously unseen magnitudes of visual improvement were realized, and amelioration nonproliferative diabetic retinopathy severity was also observed. The clinical benefit in various patient cohorts and therapeutic differences between VEGF inhibitors have also been evaluated. These and numerous other developing therapies contiunue to make the clinical care of diabetic eye disease one of the longest and most rapidly evolving areas in ophthalmology. Throughout these many remarkable advancements, the fundamental robust understanding of the natural history and epidemiology of diabetic retinopathy provided by the Klein's and others have supported and guided the many clinical trial evaluations of these therapies. -

Print This Issue
January 2011 National Institutes of Health • Department of Health and Human Services • newsinhealth.nih.gov Inside News: 3 Protein Shapes... 4 Dialysis and Kidney Patients... College Drinking... Dietary Supplements Your Aging Eyes “You might find you’re holding your book farther away to read it. You How You See as Time Goes By might even start thinking your arms You may barely notice the changes just aren’t long enough,” says Dr. at first. Maybe you’ve found Emily Chew, a clinical researcher at yourself reaching more NIH’s National Eye Institute. “A good often for your glasses to and simple treatment for presbyopia see up close. You might is reading glasses.” have trouble adjusting to Cloudy areas in the lens, called glaring lights or reading cataracts, are another common eye when the light is dim. You problem that comes with age. may even have put on blue More than 22 million Ameri- socks thinking they were cans have cataracts. By age black. These are some of 80, more than half of us the normal changes to will have had them. Some your eyes and vision as cataracts stay small and have you age. little effect on eyesight, but As more Americans others become large and head toward retirement interfere with vision. Symp- and beyond, scientists toms include blurriness, expect the number of people with of disability in older adults,” says Dr. difficulty seeing well at night, lights age-related eye problems to rise Cynthia Owsley, an eye researcher at that seem too bright and faded color dramatically. You can’t prevent all the University of Alabama at Birming- vision. -

Inside Features
Election 2020 Q&A With Candidates for U.S. House, Missouri Governor, County Executive – Page 10 Inside Features 2 p Mask Up: The Right Thing to Do 4 p Nominees for 2021 SLMMS Leadership 16 p Racial Disparities in Medical Education 24 p The FDA Drug Approval Process B:8.75" T:8" S:7" See what PNC can do for your practice. _ Get banking solutions that help you make each moment matter. S:9.625" B:11.25" T:10.5" As a healthcare provider and practice owner, you know how important it is to make each moment matter. At PNC, our dedicated team of Healthcare Business Bankers understands your business challenges. That’s why we offer a range of solutions to help your practice run more effi ciently. Whether you’re looking to expand, optimize cash fl ow, or simplify your patient payment process, we are here to help make banking easier. Visit pnc.com/hcprofessionals or call 877-566-1355 to learn more. ©2020 The PNC Financial Services Group, Inc. All rights reserved. PNC Bank, National Association. Member FDIC FILE PRINTED AT: None of Actual Size JOB#: PNC_BBK_M05097 CLIENT: The PNC Financial Services Group PROD: Melissa Betancur DATE SCALE: 1" = 1" SAP#: 11395097-1040-A0 AD TITLE: 2020 Q3 BBK Hc/Ag Print AE: N/A BLEED: 8.75" x 11.25" 8.75" x 11.25" WORK ORDER #: 82952-4.4 PUB: 2020 BBK MEMM - General Physician AD: N/A STUDIO TRIM: 8" x 10.5" 8" x 10.5" FILE NAME: PNC_BBK_M05097_GPH_A.R4.indd PUBDATE: None CW: N/A SAFETY: 7" x 9.625" 7" x 9.625" TOOLKIT #: None ARTIST: stephanie.matusewicz PR 1 2 OUTPUT FINAL AT: 100% WIP: Yes PM FILE PATH: Macintosh HD:Users:stephanie.matusewicz:Desktop:WFH:08.06:PNC_BBK_M05097_GPH_A.R4:PNC_BBK_M05097_GPH_A.R4.indd -

ARMD from Spinach to Injection
1/19/17 Risk Factors determined by the Mayo Clinic • Age. Your risk of macular degeneraon increases as you age, especially aer age 50. Macular ARMD degeneraon is most common in people older than 65. • Family history of macular degenera6on. If someone in your family had macular degeneraon, you're more likely to develop macular degeneraon. From Spinach to Injec9on • Race. Macular degeneraon is more common in whites (Caucasians) than it is in other races. • Smoking. Smoking cigareTes increases your risk of macular degeneraon. • Obesity. Being severely overweight increases the chance that early or intermediate macular degeneraon will progress to the more severe form of the disease. • Diet. A diet that includes few fruits and vegetables may increase the risk of macular degeneraon. • High blood pressure. Diseases that affect the circulatory system, such as high blood pressure or high cholesterol, may increase the risk of macular degeneraon. Steven M. Newman, O.D., C.N.S. • Inflammaon. Your immune system can cause swelling of your body 9ssues, which may Board Cer9fied Optometric Physician increase the risk of macular degeneraon. Florida Board of Optometry • Cardiovascular disease. If you have had diseases that affected your heart and blood vessels (cardiovascular disease), you may be at higher risk of macular degeneraon Board Cer9fied Nutri9on Specialist American College of Nutri8on ARMD gene9cs Hippocrates – Alternate complement pathway – ARMS2/HTRA1 – HDL cholesterol pathway “He who does not know – Extracellular matrix – Angiogenesis pathway food, how can he – Vitamin D pathway understand the diseases of man?” 1 1/19/17 Our body was designed to absorb nutrients the old fashioned way…by eang natural foods rich in an9oxidants. -

Instilling the Mission and Vision of OUWB
Service in the pre-clinical years: Instilling the mission and vision of OUWB Jean M. Szura, PhD, Rose A. Wedemeyer, PhD, Tracy L. Wunderlich, MA, Linda H. Gillum, PhD, Evan D. Fobar, & Nelia M. Afonso, MD Oakland University William Beaumont School of Medicine MATERIALS AND METHODS STRENGTHS COMPASS Center for Community Engagement – A collaboration of faculty and staff from different • Institutional support departments • Ingrained desire to engage the community. • Medical Education OBJECTIVE • Wide array of experiences • Diversity and Inclusion • Impact on community constituents The Oakland University William Beaumont • Biomedical Sciences School of Medicine (OUWB) is a community • Beaumont Health System LCME Accreditation serving its community with a mission of • OUWB Administration • COMPASS cited as an institutional strength enabling students to become skillful, Each member of COMPASS brings a unique perspective and background ethical, and compassionate physicians. AREAS FOR IMPROVEMENT Curricular Service-Learning community service tied to course curriculum as a required course It is important to gain an understanding of the component inclusive of reflection impact on the community through evaluation of The goal of this poster is to outline a new • Promotion and Maintenance of Health (PMH) Art and Practice of Medicine (APM) courses student experiences as well as the experiences of medical school’s approach to fulfilling its Faculty development and administrative support facilitated the integration of service-learning faculty and staff by conducting a 360 evaluation. vision of promoting, maintaining, and This comprehensive evaluation will include restoring health to individuals and directly into courses allowing students to connect curricular content with real-world, hands on interviews with faculty, revamping our evaluation communities served by the school and its experiences while meeting community needs. -

Anatomy, Grave-Robbing, and Spiritualism in Antebellum St. Louis
Anatomy, Grave-Robbing, and Spiritualism in Antebellum St. Louis BY LUKE RITTER 34 | The Confluence | Spring/Summer 2012 When Mrs. Malter went missing on the eleventh of September in 1849, her family suspected Dr. Joseph Nash McDowell, head of the Missouri Medical College. She was last seen at seven o’clock in the evening, walking her dog along Chouteau Avenue in south St. Louis. The mysterious disappearance of Mrs. Malter, a German immigrant married to a respected German American businessman, headlined the local newspapers. In the excitement surrounding her disappearance, one witness told reporters he thought he saw Mrs. Malter’s handkerchief, “or some other article” of hers, near McDowell’s medical college. The Missouri Medical College was then located at Eighth and Gratiot streets, just one block away from Mrs. Malter’s last known location. According to one local newspaper, the rumors about the handkerchief and McDowell’s implication in her disappearance “excited in the minds of many Germans a suspicion that she [had] been burked, seized, and taken for dissection.” St. Louisans suspected Dr. McDowell and his students of robbing the city’s graveyards for cadavers, and for good reason, but this accusation was murder. By Friday morning, September With the professionalization of medicine and medical training 14, hundreds of Germans in the city’s south side were in the late eighteenth and early nineteenth centuries came new convinced someone had seen a whole “bundle (of forms of research and teaching, including human dissection. clothing)” in front of the college. Mr. Malter demanded One occupation that emerged in response to a growing demand for cadavers was that of graverobbing. -

Resources-Doctor-AMD-AREDS2
Resources-Doctor-AMD-AREDS2 Study Title: Lutein + Zeaxanthin and Omega-3 Fatty Acids for Age-Related Macular Degeneration Study Authors(s): National Eye Institute/National Institute of Health, Lead Investigator: Dr. Emily Chew Journal: Journal of American Medical Association May 15, 2013 – Vol 309, No. 19 Sponsor: NEI/NIH, Study Meds were provided by Alcon, Bausch & Lomb, DSM and Pfizer Study Objective: 1. To determine whether adding lutein + Zeaxanthin decreases the risk of developing advanced AMD 2. To determine whether DHA + EPA decreases the risk of developing advanced AMD 3. To determine whether Lutein + Zeaxanthin + EPA + DHA decreases the risk of developing advanced AMD 4. Evaluate the effect of eliminating beta carotene from the AREDS formulation 5. Evaluate the effect of lowering zinc doses in the AREDS formulation • Design and Participants: Multi-center, randomized, double-masked, placebo-controlled phase 3 study 4203 participants aged 50 to 85 years at risk for progression to advanced AMD with bilateral large drusen or large drusen in 1 eye and advanced AMD in the fellow eye • Study Design: Participants were randomized to receive: 1. Lutein (10mg) + Zeaxanthin (2mg) 2. DHA (350mg) + EPA (650mg) 3. Lutein + Zeaxanthin + EPA + DHA 4. Placebo All Participants took one of the following: 1. Original AREDS formulation 2. Original AREDS formulation eliminating Beta-Carotene 3. Original AREDS formula with lowered zinc 25mg 4. Original AREDS formula without Beta-Carotene and lowered zinc Primary Outcome: Development of advanced AMD. The unit of analyses used was by eye. Results: Median follow-up was 5 years with 1940 study eyes. • 31% Progression to advanced AMD for placebo • 29% progression to advanced AMD for Lutein + Zeaxanthin • 31% progression to advanced AMD for DHA+EPA • 30% progression to advanced AMD for Lutein + Zeaxanthin + DHA+EPA • Null effect of beta carotene elimination or lower-dose zinc on progression to advanced AMD. -

WILLIAM BEAUMONT and HIS BOOK ELISHA NORTH and HIS COPY of BEAUMONT’S BOOK* by WILLIAM SNOW MILLER, M.D., SC.D
WILLIAM BEAUMONT AND HIS BOOK ELISHA NORTH AND HIS COPY OF BEAUMONT’S BOOK* By WILLIAM SNOW MILLER, M.D., SC.D. MADISON, WISCONSIN N 1833, Dr. William Beaumont duced me to his patients, told them that published at Plattsburgh, New it was his last visit and that he was York, a book bearing the title turning over to me all of his patients. “Experiments and Observations Some days after this he called me Ion the Gastric Juice, and the Physiolinto- his office and ottered to give me ogy of Digestion.” This was not a his library. Alas! I did not at that “pot boiler” as are many of the time possess any knowledge of medical modern books. It was a scientific history nor did I recognize the value treatise, based on observations which of his books. The old Doctor took no other person had recorded. It is down several volumes and insisted one of the outstanding contributions that 1 take them, “for,” he said, made by The United States of “they are unusual books;” one of America to scientific medicine.1 these was the volume under consideration. Histor y of AIy Copy of Beaum ont In 1886, unable to endure the The history of my copy of Beau- strenuousness of a country practice, mont is interesting. It belonged and recognizing an increasing diffi- originally to Elisha North, a dis- culty in hearing, I gave up the prac- tinguished physician, who spent the tice of medicine and resolved to devote greater part of his professional life at my time to research. -
No Slide Title
Use of Antioxidant Vitamins and Minerals in Age-Related Eye Diseases Emily Chew, M.D. National Eye Institute/National Institutes of Health Age-Related Eye Diseases Cataract AMD Sclera Retina Cornea Macula Iris Lens Cortical Cataract Normal Retina Macula Advanced AMD Neovascular AMD or Central Geographic Atrophy Importance of potential prevention age-related cataract & macular degeneration with vitamins/mineral Cataract Surgery • highly successful, huge expense Age-related macular degeneration • lack of successful treatment for the majority of cases (atrophic) Rationale for use of vitamins in age-related cataract & macular degeneration Oxidative stress • generated through photo oxidation and metabolic processes • results in reactive oxygen intermediates: free radicals, hydrogen peroxide, or singlet oxygen Rationale for use of vitamins in age-related cataract & macular degeneration • Data from animal models, in vitro experiments • Observational human data • Controlled clinical trials Studies of Cataract and Nutrition Observational studies • Cross-sectional studies • Case-control studies Controlled clinical trials Cataract: Observational Studies Cross-Sectional Studies Baltimore Longitudinal Study on Aging Nutritional Factors in Eye Disease Study Beaver Dam Eye Study Inconsistent associations with vitamins Cataract: Observational Studies Case-Control Studies of Vitamin Use India-US Case Control Study of Cataract Plasma antioxidant index (protective) Lens Opacities Case-Control Study Dietary C,E, and carotene (protective) Italian American