PDF of This Issue
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Report 2011–5010
Shahejie−Shahejie/Guantao/Wumishan and Carboniferous/Permian Coal−Paleozoic Total Petroleum Systems in the Bohaiwan Basin, China (based on geologic studies for the 2000 World Energy Assessment Project of the U.S. Geological Survey) 114° 122° Heilongjiang 46° Mongolia Jilin Nei Mongol Liaoning Liao He Hebei North Korea Beijing Korea Bohai Bay Bohaiwan Bay 38° Basin Shanxi Huang He Shandong Yellow Sea Henan Jiangsu 0 200 MI Anhui 0 200 KM Hubei Shanghai Scientific Investigations Report 2011–5010 U.S. Department of the Interior U.S. Geological Survey Shahejie−Shahejie/Guantao/Wumishan and Carboniferous/Permian Coal−Paleozoic Total Petroleum Systems in the Bohaiwan Basin, China (based on geologic studies for the 2000 World Energy Assessment Project of the U.S. Geological Survey) By Robert T. Ryder, Jin Qiang, Peter J. McCabe, Vito F. Nuccio, and Felix Persits Scientific Investigations Report 2011–5010 U.S. Department of the Interior U.S. Geological Survey U.S. Department of the Interior KEN SALAZAR, Secretary U.S. Geological Survey Marcia K. McNutt, Director U.S. Geological Survey, Reston, Virginia: 2012 For more information on the USGS—the Federal source for science about the Earth, its natural and living resources, natural hazards, and the environment, visit http://www.usgs.gov or call 1–888–ASK–USGS. For an overview of USGS information products, including maps, imagery, and publications, visit http://www.usgs.gov/pubprod To order this and other USGS information products, visit http://store.usgs.gov Any use of trade, product, or firm names is for descriptive purposes only and does not imply endorsement by the U.S. -

Table of Codes for Each Court of Each Level
Table of Codes for Each Court of Each Level Corresponding Type Chinese Court Region Court Name Administrative Name Code Code Area Supreme People’s Court 最高人民法院 最高法 Higher People's Court of 北京市高级人民 Beijing 京 110000 1 Beijing Municipality 法院 Municipality No. 1 Intermediate People's 北京市第一中级 京 01 2 Court of Beijing Municipality 人民法院 Shijingshan Shijingshan District People’s 北京市石景山区 京 0107 110107 District of Beijing 1 Court of Beijing Municipality 人民法院 Municipality Haidian District of Haidian District People’s 北京市海淀区人 京 0108 110108 Beijing 1 Court of Beijing Municipality 民法院 Municipality Mentougou Mentougou District People’s 北京市门头沟区 京 0109 110109 District of Beijing 1 Court of Beijing Municipality 人民法院 Municipality Changping Changping District People’s 北京市昌平区人 京 0114 110114 District of Beijing 1 Court of Beijing Municipality 民法院 Municipality Yanqing County People’s 延庆县人民法院 京 0229 110229 Yanqing County 1 Court No. 2 Intermediate People's 北京市第二中级 京 02 2 Court of Beijing Municipality 人民法院 Dongcheng Dongcheng District People’s 北京市东城区人 京 0101 110101 District of Beijing 1 Court of Beijing Municipality 民法院 Municipality Xicheng District Xicheng District People’s 北京市西城区人 京 0102 110102 of Beijing 1 Court of Beijing Municipality 民法院 Municipality Fengtai District of Fengtai District People’s 北京市丰台区人 京 0106 110106 Beijing 1 Court of Beijing Municipality 民法院 Municipality 1 Fangshan District Fangshan District People’s 北京市房山区人 京 0111 110111 of Beijing 1 Court of Beijing Municipality 民法院 Municipality Daxing District of Daxing District People’s 北京市大兴区人 京 0115 -

China's E-Tail Revolution: Online Shopping As a Catalyst for Growth
McKinsey Global Institute McKinsey Global Institute China’s e-tail revolution: Online e-tail revolution: shoppingChina’s as a catalyst for growth March 2013 China’s e-tail revolution: Online shopping as a catalyst for growth The McKinsey Global Institute The McKinsey Global Institute (MGI), the business and economics research arm of McKinsey & Company, was established in 1990 to develop a deeper understanding of the evolving global economy. Our goal is to provide leaders in the commercial, public, and social sectors with the facts and insights on which to base management and policy decisions. MGI research combines the disciplines of economics and management, employing the analytical tools of economics with the insights of business leaders. Our “micro-to-macro” methodology examines microeconomic industry trends to better understand the broad macroeconomic forces affecting business strategy and public policy. MGI’s in-depth reports have covered more than 20 countries and 30 industries. Current research focuses on six themes: productivity and growth; natural resources; labor markets; the evolution of global financial markets; the economic impact of technology and innovation; and urbanization. Recent reports have assessed job creation, resource productivity, cities of the future, the economic impact of the Internet, and the future of manufacturing. MGI is led by two McKinsey & Company directors: Richard Dobbs and James Manyika. Michael Chui, Susan Lund, and Jaana Remes serve as MGI principals. Project teams are led by the MGI principals and a group of senior fellows, and include consultants from McKinsey & Company’s offices around the world. These teams draw on McKinsey & Company’s global network of partners and industry and management experts. -

Exploring the Dynamic Spatio-Temporal Correlations Between PM2.5 Emissions from Different Sources and Urban Expansion in Beijing-Tianjin-Hebei Region
Article Exploring the Dynamic Spatio-Temporal Correlations between PM2.5 Emissions from Different Sources and Urban Expansion in Beijing-Tianjin-Hebei Region Shen Zhao 1,2 and Yong Xu 1,2,* 1 Institute of Geographic Sciences and Natural Resources Research, Chinese Academy of Sciences, Beijing 100101, China; [email protected] 2 College of Resources and Environment, University of Chinese Academy of Sciences, Beijing 100049, China * Correspondence: [email protected] Abstract: Due to rapid urbanization globally more people live in urban areas and, simultaneously, more people are exposed to the threat of environmental pollution. Taking PM2.5 emission data as the intermediate link to explore the correlation between corresponding sectors behind various PM2.5 emission sources and urban expansion in the process of urbanization, and formulating effective policies, have become major issues. In this paper, based on long temporal coverage and high- quality nighttime light data seen from the top of the atmosphere and recently compiled PM2.5 emissions data from different sources (transportation, residential and commercial, industry, energy production, deforestation and wildfire, and agriculture), we built an advanced Bayesian spatio- temporal autoregressive model and a local regression model to quantitatively analyze the correlation between PM2.5 emissions from different sources and urban expansion in the Beijing-Tianjin-Hebei region. Our results suggest that the overall urban expansion in the study area maintained gradual growth from 1995 to 2014, with the fastest growth rate during 2005 to 2010; the urban expansion maintained a significant positive correlation with PM2.5 emissions from transportation, energy Citation: Zhao, S.; Xu, Y. -
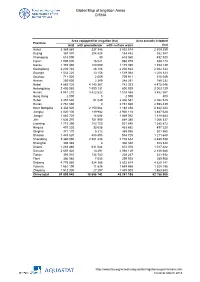
Global Map of Irrigation Areas CHINA
Global Map of Irrigation Areas CHINA Area equipped for irrigation (ha) Area actually irrigated Province total with groundwater with surface water (ha) Anhui 3 369 860 337 346 3 032 514 2 309 259 Beijing 367 870 204 428 163 442 352 387 Chongqing 618 090 30 618 060 432 520 Fujian 1 005 000 16 021 988 979 938 174 Gansu 1 355 480 180 090 1 175 390 1 153 139 Guangdong 2 230 740 28 106 2 202 634 2 042 344 Guangxi 1 532 220 13 156 1 519 064 1 208 323 Guizhou 711 920 2 009 709 911 515 049 Hainan 250 600 2 349 248 251 189 232 Hebei 4 885 720 4 143 367 742 353 4 475 046 Heilongjiang 2 400 060 1 599 131 800 929 2 003 129 Henan 4 941 210 3 422 622 1 518 588 3 862 567 Hong Kong 2 000 0 2 000 800 Hubei 2 457 630 51 049 2 406 581 2 082 525 Hunan 2 761 660 0 2 761 660 2 598 439 Inner Mongolia 3 332 520 2 150 064 1 182 456 2 842 223 Jiangsu 4 020 100 119 982 3 900 118 3 487 628 Jiangxi 1 883 720 14 688 1 869 032 1 818 684 Jilin 1 636 370 751 990 884 380 1 066 337 Liaoning 1 715 390 783 750 931 640 1 385 872 Ningxia 497 220 33 538 463 682 497 220 Qinghai 371 170 5 212 365 958 301 560 Shaanxi 1 443 620 488 895 954 725 1 211 648 Shandong 5 360 090 2 581 448 2 778 642 4 485 538 Shanghai 308 340 0 308 340 308 340 Shanxi 1 283 460 611 084 672 376 1 017 422 Sichuan 2 607 420 13 291 2 594 129 2 140 680 Tianjin 393 010 134 743 258 267 321 932 Tibet 306 980 7 055 299 925 289 908 Xinjiang 4 776 980 924 366 3 852 614 4 629 141 Yunnan 1 561 190 11 635 1 549 555 1 328 186 Zhejiang 1 512 300 27 297 1 485 003 1 463 653 China total 61 899 940 18 658 742 43 241 198 52 -

Sentencing Cases of Falun Gong Practitioners Reported in January 2021
186 Sentencing Cases of Falun Gong Practitioners Reported in January 2021 Minghui.org Case Prison Probation Year Month Fine / Police Name Province City Court Number Term (yrs) Sentenc Sentenced Extortion #1 黄日新 Huang Rixin Guangdong Dongguan Dongguan City No.2 Court 3 2020 Feb ¥ 30,000 #2 安春云 An Chunyun Tianjin Dagang Court 0.83 2020 Feb ¥ 1,000 #3 王占君 Wang Zhanjun Jilin Changchun Dehui City Court 6 2020 Mar #4 毕业海 Bi Yehai Jilin Changchun Dehui City Court 3 2020 Mar #5 刘兴华 Liu Xinghua Jilin Changchun Dehui City Court 2 2020 Mar #6 张文华 Zhang Wenhua Jilin Changchun Dehui City Court 1.5 2020 Mar #7 何维玲(何维林) He Weiling (He Weilin) Anhui Hefei Shushan District Court 2.83 2020 May #8 马庆霞 Ma Qingxia Tianjin Wuqing District Court 5 2020 Jun #9 陈德春 Chen Dechun Sichuan Chengdu 3 2020 Jun ¥ 2,000 #10 余志红 Yu Zhihong Liaoning Yingkou 1.5 2020 Jul #11 陈星伯 Chen Xingbo Hebei Xingtai Xiangdu District Court 3 2020 Aug #12 肖大富 Xiao Dafu Sichuan Dazhou Tongchuan District Court 8.5 2020 Sep #13 汤艳兰 Tang Yanlan Guangdong Jiangmen Pengjiang District Court 8 2020 Sep ¥ 10,000 #14 李行军 Li Xingjun Hubei Jingzhou 7 2020 Sep #15 孙江怡 Sun Jiangyi Hubei Jingzhou 7 2020 Sep #16 雷云波 Lei Yunbo Hubei Jingzhou 6 2020 Sep #17 陈顺英 Chen Chunying Hubei Jingzhou 3.5 2020 Sep #18 刘瑞莲 Liu Ruilian Hebei Chengde 3 2020 Sep #19 卢丽华 Lu Lihua Jiangsu Nantong Chongchuan Court 1 2020 Sep #20 张海燕 Zhang Haiyan Heilongjiang Harbin 3 3 2020 Sep #21 王亚琴 Wang Yaqin Jilin Jilin 5.5 2020 Oct #22 许凤梅 Xu Fengmei Henan Zhoukou Chuanhui District Court 5 2020 Oct #23 郭远和 Guo Yuanhe Hunan Chenzhou -

A COVID-19 Outbreak — Nangong City, Hebei Province, China, January 2021
China CDC Weekly Outbreak Reports A COVID-19 Outbreak — Nangong City, Hebei Province, China, January 2021 Shiwei Liu1,&; Shuhua Yuan2,&; Yinqi Sun2; Baoguo Zhang3; Huazhi Wang4; Jinxing Lu1; Wenjie Tan1; Xiaoqiu Liu1; Qi Zhang1; Yunting Xia1; Xifang Lyu1; Jianguo Li2,#; Yan Guo1,# On January 3, 2021, Nangong City (part of Xingtai Summary City, Hebei Province with 484,000 residents in 2017) What is known about this topic? reported its first symptomatic case of COVID-19. Coronavirus disease 2019 (COVID-19) is widespread China CDC, Hebei CDC, and Xingtai CDC jointly globally. In China, COVID-19 has been well carried out a field epidemiological investigation and controlled and has appeared only in importation- traced the outbreak. On January 6, Nangong City related cases. Local epidemics occur sporadically in started its first round of population-wide nucleic acid China and have been contained relatively quickly. screening. On January 9, Nangong City was locked What is added by this report? down by conducting control and prevention measures Epidemiological investigation with genome sequence that included staying at home and closing work units traceability analysis showed that the first case of for seven days. As of January 27, 2021, 76 cases had COVID-19 in Nangong City acquired infection from a been reported in Nangong City; among these, 8 were confirmed case from Shijiazhuang City; infection asymptomatic. No additional cases have been reported subsequently led to 76 local cases. All cases were to date, and there were no COVID-19-related deaths associated with the index case, and most were located in the outbreak. in Fenggong Street and did not spread outside of Nangong City. -

Officials Punished As China Logs Highest Daily Virus Cases Since July 7 January 2021
Officials punished as China logs highest daily virus cases since July 7 January 2021 Major highways leading into Shijiazhuang, around 300 kilometres (200 miles) south of Beijing, have been closed and inter-city bus travel halted. The state media tabloid Global Times reported that the city was in "de facto lockdown" due to the large- scale suspension of transport services. "I did the nucleic acid test last night, but don't have the results yet. Without it I can't leave the city," one young woman at Shijiazhuang train station told state broadcaster CCTV. Three officials from Shijiazhuang's Gaocheng Credit: Unsplash/CC0 Public Domain district—the epicentre of the latest outbreak—were reprimanded for their handling of the outbreak, the local disciplinary commission said Thursday. Transport services were cut off to a city of 11 The officials had allowed a woman who had tested million people near Beijing on Thursday as local positive to leave the area, the commission claimed. officials were reprimanded for a COVID-19 outbreak that pushed China's new infections to the Gaocheng district has been declared high risk and highest single-day tally since July. sealed off, and authorities said tens of thousands have already been tested for the virus. The virus first emerged in central China in late 2019, but since then authorities have largely There were 63 new COVID-19 infections in brought the situation under control through travel mainland China on Thursday, including 11 imported restrictions, strict lockdowns and mass testing. cases and one other domestic case in the northeast. But a recent outbreak in northern Hebei province, which surrounds Beijing, has seen cases spike and © 2021 AFP prompted mass testing, school closures and suspension of travel links to the province. -

Distribution, Genetic Diversity and Population Structure of Aegilops Tauschii Coss. in Major Whea
Supplementary materials Title: Distribution, Genetic Diversity and Population Structure of Aegilops tauschii Coss. in Major Wheat Growing Regions in China Table S1. The geographic locations of 192 Aegilops tauschii Coss. populations used in the genetic diversity analysis. Population Location code Qianyuan Village Kongzhongguo Town Yancheng County Luohe City 1 Henan Privince Guandao Village Houzhen Town Liantian County Weinan City Shaanxi 2 Province Bawang Village Gushi Town Linwei County Weinan City Shaanxi Prov- 3 ince Su Village Jinchengban Town Hancheng County Weinan City Shaanxi 4 Province Dongwu Village Wenkou Town Daiyue County Taian City Shandong 5 Privince Shiwu Village Liuwang Town Ningyang County Taian City Shandong 6 Privince Hongmiao Village Chengguan Town Renping County Liaocheng City 7 Shandong Province Xiwang Village Liangjia Town Henjin County Yuncheng City Shanxi 8 Province Xiqu Village Gujiao Town Xinjiang County Yuncheng City Shanxi 9 Province Shishi Village Ganting Town Hongtong County Linfen City Shanxi 10 Province 11 Xin Village Sansi Town Nanhe County Xingtai City Hebei Province Beichangbao Village Caohe Town Xushui County Baoding City Hebei 12 Province Nanguan Village Longyao Town Longyap County Xingtai City Hebei 13 Province Didi Village Longyao Town Longyao County Xingtai City Hebei Prov- 14 ince 15 Beixingzhuang Town Xingtai County Xingtai City Hebei Province Donghan Village Heyang Town Nanhe County Xingtai City Hebei Prov- 16 ince 17 Yan Village Luyi Town Guantao County Handan City Hebei Province Shanqiao Village Liucun Town Yaodu District Linfen City Shanxi Prov- 18 ince Sabxiaoying Village Huqiao Town Hui County Xingxiang City Henan 19 Province 20 Fanzhong Village Gaosi Town Xiangcheng City Henan Province Agriculture 2021, 11, 311. -

Hebei Yichen Industrial Group Corporation Limited* 河北翼辰實業
THIS CIRCULAR IS IMPORTANT AND REQUIRES YOUR IMMEDIATE ATTENTION If you are in any doubt as to any aspect of this circular or as to the action to be taken, you should consult your stockbroker or other registered dealer in securities, bank manager, solicitor, professional accountant or other professional adviser. If you have sold or transferred all your shares in Hebei Yichen Industrial Group Corporation Limited* (河北翼辰實業集團股份有限公司), you should at once hand this circular, together with the enclosed form of proxy, to the purchaser or transferee or to the bank, stockbroker or other agent through whom the sale or transfer was effected for transmission to the purchaser or transferee. Hong Kong Exchanges and Clearing Limited and The Stock Exchange of Hong Kong Limited take no responsibility for the contents of this circular, make no representation as to its accuracy or completeness and expressly disclaim any liability whatsoever for any loss howsoever arising from or in reliance upon the whole or any part of the contents of this circular. Hebei Yichen Industrial Group Corporation Limited* 河北翼辰實業集團股份有限公司 (A joint stock limited liability company incorporated in the People’s Republic of China) (Stock Code: 1596) RE-ELECTION OF DIRECTORS, RE-ELECTION OF SHAREHOLDER REPRESENTATIVE SUPERVISORS AND NOTICE OF EXTRAORDINARY GENERAL MEETING A notice convening the EGM to be held at the meeting room of the Company, No. 1 Yichen North Street, Gaocheng District, Shijiazhuang City, Hebei Province, the People’s Republic of China (the PRC) on Thursday, 6 December 2018 at 10:30 a.m. is set out on pages 22 to 24 of this circular. -

COVID-19 and Immigration Tracker
Mobility: Immigration Tracker Impact of COVID-19 on global immigration 25 January 2021 Important notes • This document provides a snapshot of the policy changes that have been announced in jurisdictions around the world in response to the COVID-19 crisis. It is designed to support conversations about policies that have been proposed or implemented in key jurisdictions • Policy changes across the globe are being proposed and implemented on a daily basis. This document is updated on an ongoing basis but not all entries will be up-to-date as the process moves forward. In addition, not all jurisdictions are reflected in this document • Find the most current version of this tracker on ey.com • Please consult with your EY engagement team to check for new updates and new developments EY teams have developed additional trackers to help you follow changes: ► Force Majeure ► Global Mobility ► Global Tax Policy ► Global Trade Considerations ► Labor and Employment Law ► Tax Controversy ► US State and Local Taxes EY professionals are updating the trackers regularly as the situation continues to develop. Page 2 Impact of COVID-19 on Global Immigration Overview/key issues • With the crisis evolving at different stages globally, government authorities continue to implement immigration-related measures to limit the spread of the COVID-19 pandemic and protect the health and safety of individuals in and outside of their jurisdictions. • Measures to stem the spread of COVID-19 include the following: • Entry restrictions and heightened admission criteria for -

Chinese Audiences' Preference For, Dependence On, and Gratifications Derived from CCTV 1, Dragon TV and Hunan TV News Programs Dongfang Nangong Iowa State University
Iowa State University Capstones, Theses and Graduate Theses and Dissertations Dissertations 2011 Chinese Audiences' Preference for, Dependence on, and Gratifications Derived from CCTV 1, Dragon TV and Hunan TV News Programs Dongfang Nangong Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/etd Part of the Communication Commons Recommended Citation Nangong, Dongfang, "Chinese Audiences' Preference for, Dependence on, and Gratifications Derived from CCTV 1, Dragon TV and Hunan TV News Programs" (2011). Graduate Theses and Dissertations. 10072. https://lib.dr.iastate.edu/etd/10072 This Thesis is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Graduate Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. Chinese audiences’ preference for, dependence on, and gratifications derived from CCTV 1, Dragon TV and Hunan TV news programs by Dongfang Nangong A thesis submitted to the graduate faculty in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE Major: Journalism and Mass Communication Program of Study Committee: Lulu Rodriguez, Major Professor Thomas Beell Mark Kaiser Iowa State University Ames, Iowa 2011 Copyright © Dongfang Nangong, 2011. All rights reserved. ii TABLE OF CONTENTS LIST OF TABLES iv ABSTRACT vi CHAPTER 1. INTRODUCTION AND STATEMENT OF THE PROBLEM 1 CHAPTER 2. LITERATURE REVIEW AND THEORETICAL FRAMEWORK 8 News credibility 9 The uses and gratifications theory 11 Media dependency theory 13 Historical/structural origins 14 Individual origins 15 Social/environmental origins 15 The Influence of Demographic Variables 16 Gender 17 Age 17 Income 18 Education 18 CHAPTER 3.