Colectomy (ACS)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hepatic Surgery
Hepatic Surgery Honorary Editors: Tan To Cheung, Long R. Jiao Editors: Zhiming Wang, Giovanni Battista Levi Sandri, Alexander Parikh Associate Editors: Yiming Tao, Michael D. Kluger, Romaric Loffroy Editors: Zhiming Wang, Giovanni Battista Levi Sandri, Levi Battista Giovanni Alexander Parikh Hepatic Surgery Honorary Editors: Tan To Cheung, Long R. Jiao Editors: Zhiming Wang, Giovanni Battista Levi Sandri, Alexander Parikh Associate Editors: Yiming Tao, Michael D. Kluger, Romaric Loffroy AME Publishing Company Room C 16F, Kings Wing Plaza 1, NO. 3 on Kwan Street, Shatin, NT, Hong Kong Information on this title: www.amegroups.com For more information, contact [email protected] Copyright © AME Publishing Company. All rights reserved. This publication is in copyright. Subject to statutory exception and to the provisions of relevant collective licensing agreements, no reproduction of any part may take place without the written permission of AME Publishing Company. First published in 2018 Printed in China by AME Publishing Company Editors: Zhiming Wang, Giovanni Battista Levi Sandri, Alexander Parikh Hepatic Surgery (Hard Cover) ISBN: 978-988-78919-1-8 AME Publishing Company, Hong Kong AME Publishing Company has no responsibility for the persistence or accuracy of URLs for external or third-party internet websites referred to in this publication, and does not guarantee that any content on such websites is, or will remain, accurate or appropriate. The advice and opinions expressed in this book are solely those of the authors and do not necessarily represent the views or practices of the publisher. No representation is made by the publisher about the suitability of the information contained in this book, and there is no consent, endorsement or recommendation provided by the publisher, express or implied, with regard to its contents. -

The American Society of Colon and Rectal Surgeons' Clinical Practice
CLINICAL PRACTICE GUIDELINES The American Society of Colon and Rectal Surgeons’ Clinical Practice Guideline for the Evaluation and Management of Constipation Ian M. Paquette, M.D. • Madhulika Varma, M.D. • Charles Ternent, M.D. Genevieve Melton-Meaux, M.D. • Janice F. Rafferty, M.D. • Daniel Feingold, M.D. Scott R. Steele, M.D. he American Society of Colon and Rectal Surgeons for functional constipation include at least 2 of the fol- is dedicated to assuring high-quality patient care lowing symptoms during ≥25% of defecations: straining, Tby advancing the science, prevention, and manage- lumpy or hard stools, sensation of incomplete evacuation, ment of disorders and diseases of the colon, rectum, and sensation of anorectal obstruction or blockage, relying on anus. The Clinical Practice Guidelines Committee is com- manual maneuvers to promote defecation, and having less posed of Society members who are chosen because they than 3 unassisted bowel movements per week.7,8 These cri- XXX have demonstrated expertise in the specialty of colon and teria include constipation related to the 3 common sub- rectal surgery. This committee was created to lead inter- types: colonic inertia or slow transit constipation, normal national efforts in defining quality care for conditions re- transit constipation, and pelvic floor or defecation dys- lated to the colon, rectum, and anus. This is accompanied function. However, in reality, many patients demonstrate by developing Clinical Practice Guidelines based on the symptoms attributable to more than 1 constipation sub- best available evidence. These guidelines are inclusive and type and to constipation-predominant IBS, as well. The not prescriptive. -
OT Resource for K9 Overview of Surgical Procedures
OT Resource for K9 Overview of surgical procedures Prepared by: Hannah Woolley Stage Level 1 2 Gynecology/Oncology Surgeries Lymphadenectomy (lymph node dissection) Surgical removal of lymph nodes Radical: most/all of the lymph nodes in tumour area are removed Regional: some of the lymph nodes in the tumour area are removed Omentectomy Surgical procedure to remove the omentum (thin abdominal tissue that encases the stomach, large intestine and other abdominal organs) Indications for omenectomy: Ovarian cancer Sometimes performed in combination with TAH/BSO Posterior Pelvic Exenteration Surgical removal of rectum, anus, portion of the large intestine, ovaries, fallopian tubes and uterus (partial or total removal of the vagina may also be indicated) Indications for pelvic exenteration Gastrointestinal cancer (bowel, colon, rectal) Gynecological cancer (cervical, vaginal, ovarian, vulvar) Radical Cystectomy Surgical removal of the whole bladder and proximal lymph nodes In men, prostate gland is also removed In women, ovaries and uterus may also be removed Following surgery: Urostomy (directs urine through a stoma on the abdomen) Recto sigmoid pouch/Mainz II pouch (segment of the rectum and sigmoid colon used to provide anal urinary diversion) 3 Radical Vulvectomy Surgical removal of entire vulva (labia, clitoris, vestibule, introitus, urethral meatus, glands/ducts) and surrounding lymph nodes Indication for radical vulvectomy Treatment of vulvar cancer (most common) Sentinel Lymph Node Dissection (SLND) Exploratory procedure where the sentinel lymph node is removed and examined to determine if there is lymph node involvement in patients diagnosed with cancer (commonly breast cancer) Total abdominal hysterectomy/bilateral saplingo-oophorectomy (TAH/BSO) Surgical removal of the uterus (including cervix), both fallopian tubes and ovaries Indications for TAH/BSO: Uterine fibroids: benign growths in the muscle of the uterus Endometriosis: condition where uterine tissue grows on structures outside the uterus (i.e. -

Information for Patients Having a Sigmoid Colectomy
Patient information – Pre-operative Assessment Clinic Information for patients having a sigmoid colectomy This leaflet will explain what will happen when you come to the hospital for your operation. It is important that you understand what to expect and feel able to take an active role in your treatment. Your surgeon will have already discussed your treatment with you and will give advice about what to do when you get home. What is a sigmoid colectomy? This operation involves removing the sigmoid colon, which lies on the left side of your abdominal cavity (tummy). We would then normally join the remaining left colon to the top of the rectum (the ‘storage’ organ of the bowel). The lines on the attached diagram show the piece of bowel being removed. This operation is done with you asleep (general anaesthetic). The operation not only removes the bowel containing the tumour but also removes the draining lymph glands from this part of the bowel. This is sent to the pathologists who will then analyse each bit of the bowel and the lymph glands in detail under the microscope. This operation can often be completed in a ‘keyhole’ manner, which means less trauma to the abdominal muscles, as the biggest wound is the one to remove the bowel from the abdomen. Sometimes, this is not possible, in which case the same operation is done through a bigger incision in the abdominal wall – this is called an ‘open’ operation. It does take longer to recover with an open operation but, if it is necessary, it is the safest thing to do. -
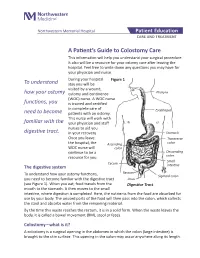
A Patient's Guide to Colostomy Care
Northwestern Memorial Hospital Patient Education CARE AND TREATMENT A Patient’s Guide to Colostomy Care This information will help you understand your surgical procedure. It also will be a resource for your ostomy care after leaving the hospital. Feel free to write down any questions you may have for your physician and nurse. During your hospital Figure 1 To understand stay you will be visited by a wound, how your ostomy ostomy and continence Pharynx (WOC) nurse. A WOC nurse functions, you is trained and certified in complete care of Esophagus need to become patients with an ostomy. This nurse will work with familiar with the your physician and staff nurses to aid you digestive tract. in your recovery. Stomach Once you leave Transverse the hospital, the Ascending colon WOC nurse will colon continue to be a Descending resource for you. colon Small Cecum The digestive system intestine Rectum To understand how your ostomy functions, Sigmoid colon you need to become familiar with the digestive tract Anus (see Figure 1). When you eat, food travels from the Digestive Tract mouth to the stomach. It then moves to the small intestine, where digestion is completed. Here, the nutrients from the food are absorbed for use by your body. The unused parts of the food will then pass into the colon, which collects the stool and absorbs water from the remaining material. By the time this waste reaches the rectum, it is in a solid form. When the waste leaves the body, it is called a bowel movement (BM), stool or feces. -
Chapter 1 History of Laparoscopic Surgery
Chapter 1 History of Laparoscopic Surgery Kiyokazu Nakajima, Jeffrey W. Milsom, and Bartholomäus Böhm Although laparoscopic surgery has transformed surgery only in the past two decades, its evolution is only the natural byproduct of the medical doctor’s curiosity to directly visualize and treat surgical dis- eases. The earliest known attempts to look inside the living human body date from 460 to 375 BC, from the Kos school of medicine led by Hippocrates in Greece.1,2 They described a rectal examination using a speculum remarkably similar to the instruments we use today. Similar specula were discovered in the ruins of Pompeii (70 AD) that were used to examine the vagina, the cervix, and the rectum, and obtain an inside view of the nose and ear.1 The Babylonian Talmud written in 500 AD described a lead siphon, named “Siphophert,” with a mouthpiece, which was bent inward and held a mechul (wooden drain).1,3 The apparatus was introduced into the vagina and was used to differentiate between vaginal and uterine bleeding. During these early years ambient light was used. The term “endoscopein” is attributed to Avicenna (Ibn Sina, 980–1037 AD) of Persia, although an Arabian physician, Albulassim (912–1013 AD), who placed a mirror in front of the exposed vagina, was the fi rst to use refl ected light as a source of illumination for an endoscopic examination. Giulio Caesare Aranzi in Venice (1530–1589) developed the fi rst endoscopic light in 1587. He used the Benedictine monk Don Panuce’s principle of the “camera obscura” for medical purposes – the -

Mucocele of the Appendix - Appendectomy Or Colectomy?
Original Article Mucocele of the appendix - appendectomy or colectomy? JANDUÍ GOMES DE ABREU FILHO1, ERIVALDO FERNANDES DE LIRA1 1Service of Coloproctology of Hospital de Base do Distrito Federal (HBDF), Secretariat of Health in Distrito Federal - Brasília (DF), Brazil. FILHO JGDA; LIRA EFD. Mucocele of the appendix - appendectomy or colectomy? Rev bras Coloproct, 2011;31(3): 276-284. ABSTRACT: Mucocele of the appendix is a rare disease. It can be triggered by benign or malignant diseases, which cause the obstruc- tion of the appendix and the consequent accumulation of mucus secretion. The preoperative diagnosis is difficult due to non-specific clinical manifestations of the disease. Imaging tests can suggest the diagnosis. The treatment is always surgical and depends on the integrity and size of the appendix base and on the histological type of the original lesion. The prognosis is good in cases of integrity of the appendix. The perforation of the appendix and subsequent extravasation of its contents into the abdominal cavity may lead to pseudomyxoma peritonei, which has very poor prognosis if not treated properly. Keywords: mucocele; appendix; pseudomyxoma peritonei; treatment. INTRODUCTION first one defends the right colectomy as a treatment9, and the second one recommends only appendecto- The mucocele of the appendix was first de- my10. Despite the different adopted conducts, in both scribed in 1842 by Rokitansky1. This disease is reported cases a cystadenoma was diagnosed in the considered as a rare lesion of the appendix, which appendix; the choice was for elective surgery. is found in 0.2 to 0.3% of the appendectomies2. It The objective of this review is to analyze liter- is characterized by the dilation of the organ lumen ature as to mucocele, especially regarding diagnosis with mucus accumulation, being more frequent and treatment, besides discussing follow-up and prog- among individuals aged 50 years or more3,4. -

Direct Oral Anticoagulants Use in the Setting of Bariatric Surgery and Feeding Tubes Excellence.Acforum.Org
Rapid Resource Direct Oral Anticoagulants Use in the Setting of Bariatric Surgery and Feeding Tubes excellence.acforum.org ACE Rapid Resources are not informed practice guidelines; they are Anticoagulation Forum, Inc.’s best recommendations based on (DOACs) NOTES current knowledge, and no warranty or guaranty is expressed or implied. The content provided is for informational purposes for medical • DOACs are absorbed at various professionals only and is not intended to be used or relied upon by them as specific medical advice, diagnosis, or treatment, the locations throughout the determination of which remains the responsibility of the medical professionals for their patients. gastrointestinal tract. Bariatric Surgery (See Table 1) • Bariatric surgery results in weight FIGURE 1 – Types of Bariatric Surgery loss by reducing stomach volume (which results in a more alkaline pH) A B C D and/or reducing effective intestinal surface area which results in malabsorption. • There is very little evidence regarding safety and efficacy of DOACs in patients with a history of bariatric surgery or requiring DOAC administration via a feeding tube. A. Adjustable gastric banding (AGB): Adjustable silicone band placed around stomach to create a smaller pouch. • This document was compiled utilizing current literature incorporating case B. Roux-en-Y gastric bypass (RYGB): reports, package inserts, and Stomach stapled to form gastric pouch that connects to distal jejunum, excluding the duodenum and proximal jejunum. pharmacokinetic studies as no current C. Gastrectomy (partial or total): randomized controlled trials are Sleeve gastrectomy results in longitudinal resection of 80% of stomach. available. As always, clinical judgment D. Biliopancreatic diversion with duodenal switch (BPD-DS): and a shared decision making Gastric pouch reattached more distally to terminal ileum resulting in considerable reduction in absorptive surface approach should be utilized. -

Hybrid Procedure Offers a Less Invasive Alternative to Colectomy
The better way to get better Hybrid procedure offers a less invasive alternative to colectomy Insufflation gas provides important advantage The colonoscopy-laparoscopy procedure is made possible through the combined skills of the gastroenterologist and laparoscopic surgeon, and the use of CO2 rather than ambient air for insufflation — the introduction of gas into the colon to improve visibility. CO2 is more quickly absorbed by the gastrointestinal tract and results in less bowel distension, giving the laparoscopic surgeon a better field of vision within the abdominal cavity. © Copyright Olympus. Used with permission. “Some patients who would have required a bowel resection can instead benefit from this A new, minimally invasive procedure that is a hybrid of colonoscopy and less invasive procedure. We’re laparoscopy is proving to be a safe and effective alternative to open colectomy using this combined technique (removal of part of the colon) for patients with benign colon polyps that are as a way for patients to avoid colectomy,” explains James not removable endoscopically. Yoo, M.D., a colorectal surgeon Patients who undergo this hybrid procedure experience less pain and often go at UCLA. “This procedure home after only one or two days. Scarring and wound complications are minimal involves tiny incisions for the as the laparoscopic surgeon makes only small, keyhole incisions in the abdomen laparoscopic instruments and patients stay in the hospital only rather than the long incision characteristic of a traditional colectomy. a day or two.” WWW.UCLAHEALTH.ORG 1-800-UCLA-MD1 (1-800-825-2631) Who can benefit from the procedure? Participating When a routine colonoscopy reveals polyps, they are usually removed at the Physicians time of the procedure as a precaution against their progression to cancer. -

DDSI Week 2019 Brochure
DDSI WEEK 2019 Digestive Disease & Surgery Institute Week 30th Anniversary Jagelman 40th Anniversary Turnbull International Colorectal Disease Symposium February 14-16, 2019 Marriott Harbor Beach Resort & Spa Fort Lauderdale, Florida 3rd Annual Pelvic Dissection taTME Cadaver Lab February 13, 2019 | M.A.R.C., Coral Gables, Florida Get your CME and MOC Points (ABS & ABIM) Call for Abstracts Deadline: November 15, 2018 8th Annual Gastroenterology and Hepatology Symposium February 14-16, 2019 Marriott Harbor Beach Resort & Spa Fort Lauderdale, Florida REGISTER ONLINE AT www.ccfcme.org/DDSI-Week 30th Anniversary Jagelman / 40th Anniversary Turnbull International Colorectal Disease Symposium February 14-16, 2019 #ccfcrs19 3rd Annual Pelvic Dissection taTME Cadaver Lab #ddsiweek19 February 13, 2019 Please join us as we celebrate our 30th Anniversary Who Should Attend? David G. Jagelman MD / 40th Anniversary Rupert Physicians, residents, fellows, nurses, wound care B. Turnbull MD International Colorectal Disease professionals, physician assistants, and allied health Symposium as part of our annual Digestive Disease professionals specializing in colorectal surgery, general and Surgery Institute Week (DDSI). This internationally surgery, laparoscopic surgery, endoscopic surgery and acclaimed gathering of surgeons from around the world gastroenterology. will be held from February 14-16, 2019 at the newly remodeled Marriott Harbor Beach Resort & Spa in Fort Lauderdale. This special anniversary course is paying Sessions tribute to the more than 1,000 surgeons from the USA Wednesday, Feb 13 and virtually every other country who have trained 3rd Annual Pelvic Dissection taTME Cadaver Lab as clinicians and/or researchers at Cleveland Clinic, Location: M.A.R.C. (Miami Anatomical Research in Florida and/or in Ohio. -

Laparoscopic Sentinel Node Mapping for Colorectal Cancer Using Infrared Ray Laparoscopy
ANTICANCER RESEARCH 26: 2307-2312 (2006) Laparoscopic Sentinel Node Mapping for Colorectal Cancer Using Infrared Ray Laparoscopy KOICHI NAGATA1, SHUNGO ENDO1, EIJI HIDAKA1, JUN-ICHI TANAKA1, SHIN-EI KUDO1 and AKIRA SHIOKAWA2 1Digestive Disease Center and 2Pathology Section, Showa University Northern Yokohama Hospital, Yokohama 224-8503, Japan Abstract. Background: Sentinel lymph node (SN) mapping colectomy (LAC). SNs were mapped by the submucosal by dye injection on conventional laparoscopy (CL) is often injection of dye on intra-operative colonoscopy, or by the precluded by the presence of mesenteric adipose tissue in use of a spinal needle and percutaneous subserosal injection patients with colorectal cancer. SN mapping on CL was of dye at a premarked site (pre-operative tattooing of compared with that on infrared ray laparoscopy (IRL) during polypectomy site with carbon). However, our experience laparoscopy-assisted colectomy (LAC). Patients and indicates that laparoscopic SN mapping by dye injection is Methods: Forty-eight patients with colorectal cancer who technically difficult because injection of the dye into the underwent LAC were enrolled. The tumor was identified by colon wall during LAC is cumbersome. Submucosal intra-operative fluoroscopy with marking clips. The tumor injection of dye on intra-operative colonoscopy makes LAC was stained intra-operatively by peritumoral injection of difficult and problematic. Distension of the small intestine indocyanine green dye. SNs were observed by CL and by IRL. with air on colonoscopy interferes with the operative field Results: In all 48 patients, dye injection and tumor and precludes laparoscopic procedures. Moreover, intra- localization during LAC were successful. The identification operative colonoscopic examinations require considerable of SNs on IRL was approximately five times better than that time, especially in patients with right-sided colon cancer. -
Operative Laparoscopy
Operative Laparoscopy Technique Procedure involves the placement of a laparoscope (special telescope with a video camera attached) into the abdomen at the belly button. The pelvis including the uterus, fallopian tubes, ovaries, bladder and appendix are all visualized to determine the source of the patient's problem. The treatment necessary is determined based upon what the surgeon sees during this exam. Potential treatments include ovarian cyst removal, ovarian removal, excision or destruction of endometriosis, and removal of scar tissue. Incisions 3-4 small incisions (less than one inch) are made on the abdomen for this procedure. Operative Time Operative times vary greatly depending on the findings at the time of surgery. Your surgeon will proceed with safety as his/her first priority. Average times range from 45-90 minutes. Anesthesia General anesthesia Preoperative Care Nothing by mouth after midnight The procedure is usually scheduled immediately after your menstrual period. Hospital Stay Day surgery or 23 hour observation Postoperative Care These guidelines are intended to give you a general idea of your postoperative course. Since every patient is unique and has a unique procedure, your recovery may differ. You will be prescribed both an anti-inflammatory and a narcotic pain medicine for postoperative use. We recommend that anti-inflammatory medications, such as ibuprofen, naproxen, etc., be used on a scheduled (regular) basis and that narcotic pain medicine be utilized on an "as needed" basis. Driving is allowed after your procedure only when you do not require the narcotic pain medicine to manage your pain. Patients may return to work in 2-3 days following the procedure.