Lung Transplantation with the OCS (Organ Care System)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Surgical Advances in Heart and Lung Transplantation
Anesthesiology Clin N Am 22 (2004) 789–807 Surgical advances in heart and lung transplantation Eric E. Roselli, MD*, Nicholas G. Smedira, MD Department of Thoracic and Cardiovascular Surgery, Cleveland Clinic Foundation, Desk F25, 9500 Euclid Avenue, Cleveland, OH 44195, USA The first heart transplants were performed in dogs by Alexis Carrel and Charles Guthrie in 1905, but it was not until the 1950s that attempts at human orthotopic heart transplant were reported. Several obstacles, including a clear definition of brain death, adequate organ preservation, control of rejection, and an easily reproducible method of implantation, slowed progress. Eventually, the first successful human to human orthotopic heart transplant was performed by Christian Barnard in South Africa in 1967 [1]. Poor healing of bronchial anastomoses hindered early progress in lung transplantation, first reported in 1963 [2]. The first successful transplant of heart and both lungs was accomplished at Stanford University School of Medicine (Stanford, CA) in 1981 [3]. The introduction of cyclosporine to immunosuppres- sion protocols, with lower doses of steroids, led to the first successful isolated lung transplant, performed at Toronto General Hospital in 1983 [4]. Since these early successes at thoracic transplantation, great progress has been made in the care of patients with end-stage heart and lung disease. Although only minor changes have occurred in surgical technique for heart and lung transplantation, the greatest changes have been in liberalizing donor criteria to expand the donor pool. This article focuses on more recent surgical advances in donor selection and management, procurement and implantation, and the impact these advances have had on patient outcome. -

Clinical Policy: Lung Transplantation Reference Number: CP.MP.57 Coding Implications Last Review Date: 05/20 Revision Log
Clinical Policy: Lung Transplantation Reference Number: CP.MP.57 Coding Implications Last Review Date: 05/20 Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Medical necessity criteria for the review of lung transplantation requests. Policy/Criteria I. It is the policy of health plans affiliated with Centene Corporation® that lung transplant for members with chronic, end-stage lung disease who have failed maximal medical therapy is medically necessary when all of the following criteria are met: A. High (> 50%) risk of death from lung disease within 2 years if lung transplantation is not performed. B. High (> 80%) likelihood of surviving at least 90 days after lung transplantation. C. High (> 80%) likelihood of 5-year post-transplant survival from a general medical perspective provided that there is adequate graft function. D. Does not have ANY of the following absolute contraindications: 1. Malignancy, except for non-melanoma localized skin cancer that has been treated appropriately, low grade prostate cancer, a malignancy that has been completely resected, or a treated malignancy determined to have a small likelihood of recurrence and acceptable future risks; 2. Untreatable significant dysfunction of another major organ system unless combined organ transplantation can be performed; 3. Uncorrected atherosclerotic disease with suspected or confirmed end-organ ischemia or dysfunction and/or coronary artery disease not amenable to revascularization; 4. Acute medical instability, including, but not limited to, acute sepsis, acute viral respiratory infection, myocardial infarction, and liver failure; 5. Uncorrectable bleeding diathesis; 6. Chronic infection with highly virulent and/or resistant microbes that are poorly controlled pre-transplant; 7. -

Case Report AJNT
Arab Journal of Nephrology and Transplantation. 2011 Sep;4(3):155-8 Case Report AJNT High Ureteric Injury Following Multiorgan Recovery: Successful Kidney Transplant with Boari Flap Ureterocystostomy Reconstruction Michael Charlesworth*, Gabriele Marangoni, Niaz Ahmad Department of Transplantation, Division of Surgery, St James’s University Hospital, Leeds, United Kingdom Abstract Keywords: Kidney; Transplant; Ureter; Donor efficiency Introduction: Despite increased utilization of marginal organs, there is still a marked disparity between organ The authors declared no conflict of interest supply and demand for transplantation. To maximize resources, it is imperative that procured organs are in Introduction good condition. Surgical damage at organ recovery can happen and organs are sometimes discarded as a result. Despite the extension of the donor pool with the inclusion We describe a damaged recovered kidney with high of marginal organs and the use of organs donated after ureteric transection that was successfully transplanted cardiac death, there is still a great disparity between the using a primary Boari flap ureterocystostomy. number of patients on the transplant waiting list and the number of kidney transplants performed each year. Case report: The donor kidney was procured form a It is therefore of paramount importance to maximize deceased donor and sustained damage by transection our scarce resources and avoid the discard of otherwise of the ureter just distal to the pelvi-ureteric junction at functional kidneys due to iatrogenic injuries at the time organ recovery. The recipient had been on the transplant of multi-organ recovery. Essentially, three types of organ waiting list for eight years and not accepting this kidney damage can potentially occur: vascular, parenchymal would have seriously jeopardized her chance of future and ureteric. -

Pelvic Anatomyanatomy
PelvicPelvic AnatomyAnatomy RobertRobert E.E. Gutman,Gutman, MDMD ObjectivesObjectives UnderstandUnderstand pelvicpelvic anatomyanatomy Organs and structures of the female pelvis Vascular Supply Neurologic supply Pelvic and retroperitoneal contents and spaces Bony structures Connective tissue (fascia, ligaments) Pelvic floor and abdominal musculature DescribeDescribe functionalfunctional anatomyanatomy andand relevantrelevant pathophysiologypathophysiology Pelvic support Urinary continence Fecal continence AbdominalAbdominal WallWall RectusRectus FasciaFascia LayersLayers WhatWhat areare thethe layerslayers ofof thethe rectusrectus fasciafascia AboveAbove thethe arcuatearcuate line?line? BelowBelow thethe arcuatearcuate line?line? MedianMedial umbilicalumbilical fold Lateralligaments umbilical & folds folds BonyBony AnatomyAnatomy andand LigamentsLigaments BonyBony PelvisPelvis TheThe bonybony pelvispelvis isis comprisedcomprised ofof 22 innominateinnominate bones,bones, thethe sacrum,sacrum, andand thethe coccyx.coccyx. WhatWhat 33 piecespieces fusefuse toto makemake thethe InnominateInnominate bone?bone? PubisPubis IschiumIschium IliumIlium ClinicalClinical PelvimetryPelvimetry WhichWhich measurementsmeasurements thatthat cancan bebe mademade onon exam?exam? InletInlet DiagonalDiagonal ConjugateConjugate MidplaneMidplane InterspinousInterspinous diameterdiameter OutletOutlet TransverseTransverse diameterdiameter ((intertuberousintertuberous)) andand APAP diameterdiameter ((symphysissymphysis toto coccyx)coccyx) -

Skin Is Not the Largest Organ
View metadata, citation and similar papers at core.ac.uk brought to you by CORE providedRD by Elsevier Sontheimer - Publisher Connector Skin is Not the Largest Organ 3 content. CHS, JNB, and MAS were involved in Paris, France; Division of Genetics and susceptibility to psoriasis vulgaris. J Invest study supervision. Molecular Medicine, St John’s Institute of Dermatol 134:271–3 Dermatology, Guy’s Hospital, London, UK; Martin MA, Klein TE, Dong BJ et al. (2012) Clinical 1,8 4 Alexander A. Navarini , Guy’s and St Thomas’ NHS Foundation pharmacogenetics implementation consortium Trust, Skin Therapy Research Unit, St John’s Laurence Valeyrie-Allanore2,8, guidelines for HLA-B genotype and abacavir 1 Institute of Dermatology, St Thomas’ Hospital, dosing. Clin Pharmacol Ther 91:734–8 Niovi Setta-Kaffetzi , London, UK; 5King’s College Hospital, London, Jonathan N. Barker1,3,4, UK; 6University Medical Center Freiburg, Navarini AA, Valeyrie-Allanore L, Setta-Kaffetzi N et al. (2013) Rare variations in IL36RN in 1 5 Institute of Medical Biometry and Medical Francesca Capon , Daniel Creamer , severe adverse drug reactions manifesting as 2 6 Informatics, Freiburg, Germany and Jean-Claude Roujeau , Peggy Sekula , 7 acute generalized exanthematous pustulosis. 1 Department of Dermatology, J Invest Dermatol 133:1904–7 Michael A. Simpson , Dokumentationszentrum Schwerer 1 Richard C. Trembath , Hautreaktionen (dZh), Universita¨ts-Hautklinik, Setta-Kaffetzi N, Navarini AA, Patel VM et al. (2013) Maja Mockenhaupt7,8 and Freiburg, Germany Rare pathogenic variants in IL36RN underlie a spectrum of psoriasis-associated 1,3,4,8 8 Catherine H. Smith These authors contributed equally to this work. -

Chronic Lung Allograft Dysfunction Post Lung Transplantation: a Review of Computed Tomography Quantitative Methods for Detection and Follow-Up
Journal of Clinical Medicine Review Chronic Lung Allograft Dysfunction Post Lung Transplantation: A Review of Computed Tomography Quantitative Methods for Detection and Follow-Up Trieu-Nghi Hoang-Thi 1,2,3 , Guillaume Chassagnon 1, Thong Hua-Huy 3, Veronique Boussaud 4, Anh-Tuan Dinh-Xuan 3 and Marie-Pierre Revel 1,* 1 AP-HP.Centre, Hôpital Cochin, Department of Radiology, Université de Paris, 75014 Paris, France; [email protected] (T.-N.H.-T.); [email protected] (G.C.) 2 Department of Diagnostic Imaging, Vinmec Central Park Hospital, Ho Chi Minh City 70000, Vietnam 3 AP-HP.Centre, Hôpital Cochin, Department of Respiratory Physiology, Université de Paris, 75014 Paris, France; [email protected] (T.H.-H.); [email protected] (A.-T.D.-X.) 4 AP-HP.Centre, Hôpital Cochin, Department of Pneumology, Université de Paris, 75014 Paris, France; [email protected] * Correspondence: [email protected]; Tel.: +33-1-5841-2471 Abstract: Chronic lung allograft dysfunction (CLAD) remains the leading cause of morbidity and mortality after lung transplantation. The term encompasses both obstructive and restrictive pheno- types, as well as mixed and undefined phenotypes. Imaging, in addition to pulmonary function tests, plays a major role in identifying the CLAD phenotype and is essential for follow-up after Citation: Hoang-Thi, T.-N.; lung transplantation. Quantitative imaging allows for the performing of reader-independent precise Chassagnon, G.; Hua-Huy, T.; Boussaud, V.; Dinh-Xuan, A.-T.; evaluation of CT examinations. In this review article, we will discuss the role of quantitative imaging Revel, M.-P. -

GLOSSARY of MEDICAL and ANATOMICAL TERMS
GLOSSARY of MEDICAL and ANATOMICAL TERMS Abbreviations: • A. Arabic • abb. = abbreviation • c. circa = about • F. French • adj. adjective • G. Greek • Ge. German • cf. compare • L. Latin • dim. = diminutive • OF. Old French • ( ) plural form in brackets A-band abb. of anisotropic band G. anisos = unequal + tropos = turning; meaning having not equal properties in every direction; transverse bands in living skeletal muscle which rotate the plane of polarised light, cf. I-band. Abbé, Ernst. 1840-1905. German physicist; mathematical analysis of optics as a basis for constructing better microscopes; devised oil immersion lens; Abbé condenser. absorption L. absorbere = to suck up. acervulus L. = sand, gritty; brain sand (cf. psammoma body). acetylcholine an ester of choline found in many tissue, synapses & neuromuscular junctions, where it is a neural transmitter. acetylcholinesterase enzyme at motor end-plate responsible for rapid destruction of acetylcholine, a neurotransmitter. acidophilic adj. L. acidus = sour + G. philein = to love; affinity for an acidic dye, such as eosin staining cytoplasmic proteins. acinus (-i) L. = a juicy berry, a grape; applied to small, rounded terminal secretory units of compound exocrine glands that have a small lumen (adj. acinar). acrosome G. akron = extremity + soma = body; head of spermatozoon. actin polymer protein filament found in the intracellular cytoskeleton, particularly in the thin (I-) bands of striated muscle. adenohypophysis G. ade = an acorn + hypophyses = an undergrowth; anterior lobe of hypophysis (cf. pituitary). adenoid G. " + -oeides = in form of; in the form of a gland, glandular; the pharyngeal tonsil. adipocyte L. adeps = fat (of an animal) + G. kytos = a container; cells responsible for storage and metabolism of lipids, found in white fat and brown fat. -

Human Anatomy and Physiology
LECTURE NOTES For Nursing Students Human Anatomy and Physiology Nega Assefa Alemaya University Yosief Tsige Jimma University In collaboration with the Ethiopia Public Health Training Initiative, The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education 2003 Funded under USAID Cooperative Agreement No. 663-A-00-00-0358-00. Produced in collaboration with the Ethiopia Public Health Training Initiative, The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education. Important Guidelines for Printing and Photocopying Limited permission is granted free of charge to print or photocopy all pages of this publication for educational, not-for-profit use by health care workers, students or faculty. All copies must retain all author credits and copyright notices included in the original document. Under no circumstances is it permissible to sell or distribute on a commercial basis, or to claim authorship of, copies of material reproduced from this publication. ©2003 by Nega Assefa and Yosief Tsige All rights reserved. Except as expressly provided above, no part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without written permission of the author or authors. This material is intended for educational use only by practicing health care workers or students and faculty in a health care field. Human Anatomy and Physiology Preface There is a shortage in Ethiopia of teaching / learning material in the area of anatomy and physicalogy for nurses. The Carter Center EPHTI appreciating the problem and promoted the development of this lecture note that could help both the teachers and students. -

Islet Interleukin-1Β Immunoreactivity Is an Early Feature of Cystic Fibrosis That May Contribute to Β-Cell Failure
Diabetes Care 1 Islet Interleukin-1b Rebecca L. Hull,1 Ronald L. Gibson,2 Sharon McNamara,2 Gail H. Deutsch,3 Immunoreactivity Is an Early Corinne L. Fligner,3 Charles W. Frevert,1,4 Bonnie W. Ramsey,2 and Srinath Sanda5,6 Feature of Cystic Fibrosis That May Contribute to b-Cell Failure https://doi.org/10.2337/dc17-1387 OBJECTIVE Cystic fibrosis–related diabetes (CFRD) is a common complication of cystic fibrosis (CF), increasing patient morbidity and mortality. Poor understanding of CFRD path- ogenesis limits the development of targeted therapies to treat and/or prevent the disease. The aim of this study was to evaluate islet pathology, specifically, inflam- mation, amyloid deposition, and endocrine cell composition in subjects with CF with diabetes and with CF without diabetes. RESEARCH DESIGN AND METHODS A retrospective analysis of archived pancreas tissue collected at autopsy was con- ducted using pancreas tissue from subjects with CF and diabetes (CFRD) (n = 18) and PATHOPHYSIOLOGY/COMPLICATIONS CF without diabetes (CF-no DM) (n = 17). Two cohorts of control non-CF subjects were identified, each matched to CFRD and CF-no DM subjects for age, sex, and BMI (non-CF older, n = 20, and non-CF younger, n = 20), respectively. Immunohistochem- istry was performed to assess IL-1b and islet hormone (insulin, glucagon, somato- statin, and pancreatic polypeptide) immunoreactivity; histochemistry was performed 1Department of Medicine, University of Wash- to quantify amyloid deposition. ington, Seattle, WA 2Department of Pediatrics, University of Wash- RESULTS ington, Seattle, WA 3Department of Pathology, University of Wash- Islet IL-1b immunoreactivity was substantially increased in both CFRD and CF-no DM ington, Seattle, WA subjects compared with non-CF subjects and was common in young subjects with CF 4Department of Comparative Medicine, Univer- (£10 years of age). -
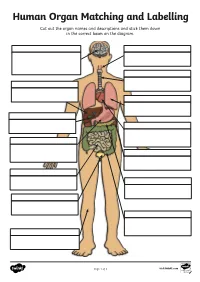
Human Organ Matching and Labelling Cut out the Organ Names and Descriptions and Stick Them Down in the Correct Boxes on the Diagram
Human Organ Matching and Labelling Cut out the organ names and descriptions and stick them down in the correct boxes on the diagram. Page 1 of 3 visit twinkl.com Maintains body temperature using Receives food from the oesophagus sweat and goosebumps. and begins to break it down with digestive juices (enzymes). Controls all of our necessary bodily functions, sends the Transports air from the nose and impulses which allow us to move mouth to the lungs. and enables you to think and learn. Pumps oxygenated blood around your body and receives de- oxygenated blood back. Filters water and salt out of your oesophagus blood and creates urine. bladder Makes bile for digestion, filters out toxins and regulates blood sugar. liver Produces enzymes necessary for large intestine digestion. gall bladder Digests food using enzymes and absorbs nutrients for the blood. kidneys Continues the digestion process, stomach absorbs as much water as possible and expels excess fibre and waste. heart Stores and concentrates bile pancreas produced by the liver. lungs Takes in oxygen, which reaches the blood via the heart. small intestine Stores urine so that we can decide trachea when we want to go to the toilet. skin Transports food and drink from the mouth to the stomach. brain Page 2 of 3 visit twinkl.com Answers brain oesophagus Controls all of our necessary bodily Transports food and drink from the functions, sends the impulses which mouth to the stomach. allow us to move and enables you to think and learn. trachea Transports air from the nose and liver mouth to the lungs. -

A Case Study in Organ Allocation Policy and Administrative Law
139 Journal of Health & Biomedical Law, XIV (2018) 139-148 © 2018 Journal of Health & Biomedical Law Suffolk University Law School THE LUNG LAWSUIT: A CASE STUDY IN ORGAN ALLOCATION POLICY AND ADMINISTRATIVE LAW Alexandra K. Glazier, J.D., M.P.H.* In November 2017, twenty-one-year-old Miriam Holman, was waiting for a lung transplant.1 Miriam was suffering from a rare form of pulmonary hypertension for which there is no medical therapy, and which is rapidly fatal without lung transplantation. Miriam was on an artificial lung machine in the ICU at Columbia Medical Center in New York where she was listed for organ transplantation.2 Organ allocation policies are, under federal law, designed to balance equity and utility principles based on medical criteria to rank order patients waiting for suitable organs to be available that are a biological match.3 Allocation policy therefore, incorporates factors such as (1) how critically ill the patient waiting is; (2) how long the patient has been waiting; and (3) for some organs allocation policies, the relative magnitude of the * Ms. Glazier is President and CEO of New England Donor Services, the two OPOs serving Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island and Vermont, a member of the OPTN Board of Directors, previously chaired the OPTN Ethics Committee and has twice been appointed to the U.S. Secretary of HHS, Advisory Committee on Organ Transplantation. 1 Complaint at 18, Holman v. Secretary of HHS, No. 17-cv-09041 (S.D.N.Y. filed Nov. 11, 2017) (describing the plaintiff’s medical history). 2 Id. -

Airway Versus Transbronchial Biopsy and BAL in Lung Transplant Recipients: Different but Complementary
Eur Respir J 1997; 10: 2876–2880 Copyright ERS Journals Ltd 1997 DOI: 10.1183/09031936.97.10122876 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 Airway versus transbronchial biopsy and BAL in lung transplant recipients: different but complementary C. Ward, G.I. Snell, B. Orsida, L. Zheng, T.J. Williams, E.H. Walters Airway versus transbronchial biopsy and BAL in lung transplant recipients: different Dept of Respiratory Medicine, Alfred but complementary. C. Ward, G.I. Snell, B. Orsida, L. Zheng, T.J. Williams, E.H. Walters. Hospital and Monash University Medical ©ERS Journals Ltd 1997. School, Melbourne, Australia. ABSTRACT: Lung transplantation is now an established therapeutic intervention Correspondence: E.H Walters for end-stage cardiopulmonary disease in humans. Chronic rejection, in the form Dept of Respiratory Medicine of bronchiolitis obliterans syndrome (BOS), remains the commonest cause of mor- Alfred Hospital bidity and mortality in those surviving more than 3 months. The pathology of BOS Prahran involves airway changes. We have evaluated the potential for endobronchial biop- Melbourne sies (EBB) to complement existing sampling methods used in allograft monitoring Victoria 3181 and have compared the results of EBB findings with those of bronchoalveolar Australia lavage (BAL) and transbronchial biopsy (TBB) in 18 clinically stable patients. Keywords: Bronchoalveolar lavage We found that all the EBB had inflammatory cells present but that only five endobronchial biopsy TBB specimens had evidence of inflammation, with airway material being present lung transplant in 78% of the TBB. Paired BAL and EBB yielded different results, with no cor- transbronchial biopsy relations between total macrophages, lymphocytes, CD4+ cells or CD8+ cells.