Molecular Effects of Polyphenols in Experimental Type 2 Diabetes Mellitus and Metabolic Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

367.Full.Pdf
Human Complement Factor I Does Not Require Cofactors for Cleavage of Synthetic Substrates This information is current as Stefanos A. Tsiftsoglou and Robert B. Sim of October 2, 2021. J Immunol 2004; 173:367-375; ; doi: 10.4049/jimmunol.173.1.367 http://www.jimmunol.org/content/173/1/367 Downloaded from References This article cites 41 articles, 17 of which you can access for free at: http://www.jimmunol.org/content/173/1/367.full#ref-list-1 Why The JI? Submit online. http://www.jimmunol.org/ • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average by guest on October 2, 2021 Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2004 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Human Complement Factor I Does Not Require Cofactors for Cleavage of Synthetic Substrates1 Stefanos A. Tsiftsoglou2 and Robert B. Sim Complement factor I (fI) plays a major role in the regulation of the complement system. It circulates in an active form and has very restricted specificity, cleaving only C3b or C4b in the presence of a cofactor such as factor H (fH), complement receptor type 1, membrane cofactor protein, or C4-binding protein. -

THE EFFECTS of ENVIRONMENTAL and PHYSICAL STRESS on ENERGY EXPENDITURE, ENERGY INTAKE, and APPETITE by Iva Mandic a Thesis Subm
THE EFFECTS OF ENVIRONMENTAL AND PHYSICAL STRESS ON ENERGY EXPENDITURE, ENERGY INTAKE, AND APPETITE by Iva Mandic A thesis submitted in conformity with the requirements for the degree of Doctor of Philosophy Graduate Department of Exercise Science University of Toronto © Copyright by Iva Mandic (2018) The effects of environmental and physical stress on energy expenditure, energy intake, and appetite Iva Mandic Doctor of Philosophy The Graduate Department of Exercise Sciences University of Toronto 2018 Abstract Body weight loss occurs frequently in military personnel engaged in field operations. When this weight loss is rapid, or extensive it is associated with health and performance decrements. While the nature of military work does not allow for energy expenditure (EE) to be freely altered, energy intake (EI) can be increased to match EE and prevent weight loss. Therefore a primary objective of the current dissertation was to develop a physiological and empirical basis to facilitate informed estimates of the EI that would be required to offset the EE demand of military tasks during field operations. Three different approaches were undertaken: 1) The energy costs of 46 infantry tasks were measured; the results should reduce the dependency on less accurate predictions. 2) The impact of ambient temperature on EE of the tasks was minimal (~3%) when the ambient temperature was between -10°C and 30°C. This indicates that caloric supplementation of field rations on account of temperature is likely unnecessary during short-term operations occurring within this temperature range; and, lastly 3) A simple algorithm based on accelerometry and heart rate was developed to assess EE in the field. -

Relationship Between Digestive Enzymes, Proteins and Anti-Nutritive Factors in Monogastric Digestion
RELATIONSHIP BETWEEN DIGESTIVE ENZYMES, PROTEINS AND ANTI-NUTRITIVE FACTORS IN MONOGASTRIC DIGESTION By: Theofilos Kempapidis A Thesis Submitted in Partial Fulfilment of the Requirements for the Degree of Doctor of Philosophy Department of Chemical and Biological Engineering Faculty of Engineering The University of Sheffield December 2019 ‘To my beloved mother, whom I couldn’t have done this without and to the memory of my beloved father that passed away during my PhD.’ i ABSTRACT Monogastrics’ lack of some digestive enzymes is compensated by using exogenous enzymes in the animal feed. Those interact with feed ingredients causing enzyme inhibition. Two known inhibiting substances are phytic acid and polyphenolics. Phytase is an important exogenous enzyme that is breaking down phytic acid. The effect of sorghum polyphenolic-rich extracts on the 6-phytase activity was investigated using an ITC by calculating its relative activity. Results show inhibition of the phytase, from all three extracts. For a better understanding of this assay, a real-time mass spectroscopic analysis was performed, that showed the pattern in which the phytase is hydrolysing phytic acid. Consecutively, the effect of phytic acid on the activity of three proteases exogenous and endogenous chymotrypsin and endogenous trypsin was studied. A colorimetric assay using casein as a substrate was used. The results showed different levels of inhibition of all three enzymes by phytic acid. Finally, the interaction between the exogenous chymotrypsin and the phytase was studied by using the ITC enzyme assay and an SDS-Page gel analysis. ITC results showed partial inhibition of the phytase activity, while SDS-Page results showed complete inhibition. -

Essential Trace Elements in Human Health: a Physician's View
Margarita G. Skalnaya, Anatoly V. Skalny ESSENTIAL TRACE ELEMENTS IN HUMAN HEALTH: A PHYSICIAN'S VIEW Reviewers: Philippe Collery, M.D., Ph.D. Ivan V. Radysh, M.D., Ph.D., D.Sc. Tomsk Publishing House of Tomsk State University 2018 2 Essential trace elements in human health UDK 612:577.1 LBC 52.57 S66 Skalnaya Margarita G., Skalny Anatoly V. S66 Essential trace elements in human health: a physician's view. – Tomsk : Publishing House of Tomsk State University, 2018. – 224 p. ISBN 978-5-94621-683-8 Disturbances in trace element homeostasis may result in the development of pathologic states and diseases. The most characteristic patterns of a modern human being are deficiency of essential and excess of toxic trace elements. Such a deficiency frequently occurs due to insufficient trace element content in diets or increased requirements of an organism. All these changes of trace element homeostasis form an individual trace element portrait of a person. Consequently, impaired balance of every trace element should be analyzed in the view of other patterns of trace element portrait. Only personalized approach to diagnosis can meet these requirements and result in successful treatment. Effective management and timely diagnosis of trace element deficiency and toxicity may occur only in the case of adequate assessment of trace element status of every individual based on recent data on trace element metabolism. Therefore, the most recent basic data on participation of essential trace elements in physiological processes, metabolism, routes and volumes of entering to the body, relation to various diseases, medical applications with a special focus on iron (Fe), copper (Cu), manganese (Mn), zinc (Zn), selenium (Se), iodine (I), cobalt (Co), chromium, and molybdenum (Mo) are reviewed. -

TRPV1: a Potential
Opinion TRPV1: A Potential Therapeutic Target in Type 2 Diabetes and Comorbidities? 1, 2 3 Dorte X. Gram, * Jens J. Holst, and Arpad Szallasi With an estimated 422 million affected patients worldwide in 2016, type 2 Trends diabetes (T2D) has reached pandemic proportions and represents a major T2D is being increasingly recognized as unmet medical need. T2D is a polygenic disease with a chronic, low-grade a disease with a chronic, low-grade inflammatory component; in preclinical inflammatory component. Second-generation transient receptor potential models, elimination of this inflammatory vanilloid-1 (TRPV1) antagonists are potent anti-inflammatory agents with proven response improves glucose homeosta- clinical safety. In rodent models of T2D, TRPV1 blockade was shown to halt sis and halts disease progression. disease progression and improve glucose metabolism. Thus, we propose that T2D is a heterogeneous disease, so a TRPV1 antagonists merit further study as novel therapeutic approaches to ‘one-size-fits-all’ approach in drug potentially treat T2D and its comorbidities. development may not be feasible (elicits the need for personalized medicine). Novel antidiabetic agents that not only The Human and Monetary Cost of Type 2 Diabetes: A Need for Novel return blood glucose to near normal Therapeutic Interventions levels but also treat comorbidities such Globally, the estimated number of diabetic patients has increased from 108 million in 1980 to as obesity and hyperlipidemia at the i same time are needed. 422 million in 2016 and the disease has thus reached pandemic proportions . We posit that TRPV1 antagonists may In the United States, the prevalence of Type 2 diabetes (T2D, see Glossary and Box 1) is also serve as putative antidiabetic agents to on the rise, following the global trend. -

Peripheral Regulation of Pain and Itch
Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1596 Peripheral Regulation of Pain and Itch ELÍN INGIBJÖRG MAGNÚSDÓTTIR ACTA UNIVERSITATIS UPSALIENSIS ISSN 1651-6206 ISBN 978-91-513-0746-6 UPPSALA urn:nbn:se:uu:diva-392709 2019 Dissertation presented at Uppsala University to be publicly examined in A1:107a, BMC, Husargatan 3, Uppsala, Friday, 25 October 2019 at 13:00 for the degree of Doctor of Philosophy (Faculty of Medicine). The examination will be conducted in English. Faculty examiner: Professor emeritus George H. Caughey (University of California, San Francisco). Abstract Magnúsdóttir, E. I. 2019. Peripheral Regulation of Pain and Itch. Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1596. 71 pp. Uppsala: Acta Universitatis Upsaliensis. ISBN 978-91-513-0746-6. Pain and itch are diverse sensory modalities, transmitted by the somatosensory nervous system. Stimuli such as heat, cold, mechanical pain and itch can be transmitted by different neuronal populations, which show considerable overlap with regards to sensory activation. Moreover, the immune and nervous systems can be involved in extensive crosstalk in the periphery when reacting to these stimuli. With recent advances in genetic engineering, we now have the possibility to study the contribution of distinct neuron types, neurotransmitters and other mediators in vivo by using gene knock-out mice. The neuropeptide calcitonin gene-related peptide (CGRP) and the ion channel transient receptor potential cation channel subfamily V member 1 (TRPV1) have both been implicated in pain and itch transmission. In Paper I, the Cre- LoxP system was used to specifically remove CGRPα from the primary afferent population that expresses TRPV1. -

Serum Proteases Alter the Antigenicity of Peptides Presented by Class I
Proc. Nati. Acad. Sci. USA Vol. 89, pp. 8347-8350, September 1992 Immunology Serum proteases alter the antigenicity of peptides presented by class I major histocompatibility complex molecules (antigen presentation/cytotoxic T lymphocytes/imnmunotherapy/vaccine) Louis D. FALO, JR.*t, LEONARD J. COLARUSSO*, BARUJ BENACERRAF*t, AND KENNETH L. ROCK*t *Division of Lymphocyte Biology, Dana-Farber Cancer Institute, Boston, MA 02115; and Departments of tDermatology and SPathology, Harvard Medical School, Boston, MA 02115 Contributed by Baruj Benacerraf, June 4, 1992 ABSTRACT Any effect of serum on the antigenicity of tions for peptide-based vaccine design and immunotherapy peptides is potentially relevant to their use as immunogens in are discussed. vivo. Here we demonstrate that serum contains distinct prote- ases that can increase or decrease the antigenicity of peptides. AND METHODS By using a functional assay, we show that a serum component MATERIALS other than P2-microglobulin enhances the presentation of Reagents. Chicken ovalbumin (OVA) was purchased from ovalbumin peptides produced by cyanogen bromide cleavage. Sigma. CNBr cleavage of OVA was preformed as described Three features of this serum activity implicate proteolysis: it is (8). The peptide corresponding to amino acids 257-264 [OVA- temperature dependent, it results in increased antigenicity in a (257-264)] was synthesized at the molecular biology core low molecular weight peptide fraction, and it is inhibited by the facility of the Dana-Farber Cancer Institute. Purified human protease inhibitor leupeptin. Conversely, presentation of the 132-microglobulin, leupeptin, and bestatin were purchased synthetic peptide OVA-(257-264) is inhibited by serum. This from Sigma. inhibition is unaffected by leupeptin but is blocked by bestatin, Cell Lines. -

Vol.50 Issue No.02 February 2013
Vol.50 Issue No.02 FEBRUARY 2013 INDIAN DRUGS 50(02) FEBRUARY 2013 1 2 INDIAN DRUGS 50(02) FEBRUARY 2013 Vol. 50 No. 02 February 2013 REVIEW ARTICLE - Protease Inhibitors: A Review Sapkale P. V., Jadhav S. B. and Sable P. N. ................................................................. 5 ORIGINAL RESEARCH ARTICLES - Method Development and Validation of Olanzapine in Pure and Pharmaceutical Dosage form by RP-HPLC Method Mastiholimath V.S., Dandagi P.M., Gadad A.P., Murali Krishna N.V. and Mannur V. .............................................................................................................. 20 - Quantitative Determination of Deferasirox in Bulk and Pharmaceutical Formulation by UV Spectrophotometric Method Marathe G. M., Pande V. V., Patil P. H., Mutha R. E. and Bari S. B. ........................... 27 - Preclinical Evaluation of Nootropic Activity of Glabridin Rich Extract of Glycyrrhiza Glabra using Passive Avoidance Paradigm in Rats Desai S. K., Pandey C. H. and Mulgaonkar S.M. ......................................................... 33 - Antihyperglycemic and In Vitro Antioxidant Activities of Punica Granatum Linn. in Alloxan Induced Diabetic Rats Patil U. S., Bandawane D. D., Bibave K. H. and Chaudhari P. D. ................................ 39 SHORT NOTES - A Novel Method For Isolation of Mangiferin from Mangifera Indica L. Bark Gholkar M. S and Laddha K. S. ................................................................................... 47 - Anti-Inflammatory Effect of Seeds ofTamarindus Indica in Wistar Rats Hivrale M. G., Mali A. A. and Bandawane D. D. ........................................................... 49 INDIAN DRUG MANUFACTURERS' ASSOCIATION 102-B, 'A-Wing', Poonam Chambers, Dr. A.B. Road, Worli, Mumbai - 400 018 Tel : 022-2494 4624 / 2497 4308 Fax: 022-2495 0723 E-mail: [email protected] / [email protected], Website: www.idma-assn.org INDIAN DRUGS 50(02) FEBRUARY 2013 3 Founder Editor *Dr. -

Treatment of Streptozotocin-Induced Diabetic Rats with Alogliptin: Effect on Vascular and Neural Complications
Hindawi Publishing Corporation Experimental Diabetes Research Volume 2011, Article ID 810469, 7 pages doi:10.1155/2011/810469 Research Article Treatment of Streptozotocin-Induced Diabetic Rats with Alogliptin: Effect on Vascular and Neural Complications Eric P. Davidson,1 Lawrence J. Coppey,1 Brian Dake,1 and Mark A. Yorek1, 2 1 Department of Internal Medicine, University of Iowa, Iowa City, IA 52246, USA 2 Department of Veterans Affairs Iowa City Health Care System, Iowa City, IA 52246, USA Correspondence should be addressed to Mark A. Yorek, [email protected] Received 14 May 2011; Accepted 21 June 2011 Academic Editor: A. Veves Copyright © 2011 Eric P. Davidson et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. We sought to determine the effect of dipeptidyl peptidase IV (DPP-IV) inhibition on streptozotocin diabetes-induced vascular and neural dysfunction. After 4 weeks of untreated diabetes, rats were treated for 12 weeks with Alogliptin (DPP-IV inhibitor). Diabetes caused a slowing of motor and sensory nerve conduction velocity, thermal hypoalgesia, reduction in intraepidermal nerve fiber density in the hindpaw, and impairment in vascular relaxation to acetylcholine and calcitonin gene-related peptide in epineurial arterioles. Treatment significantly improved motor nerve conduction velocity and thermal response latency. Sensory nerve conduction velocity was marginally improved with treatment of diabetic rats, and treatment did not improve the decrease in intraepidermal nerve fiber density. Vascular relaxation by epineurial arterioles to calcitonin gene-related peptide but not acetylcholine was significantly improved with treatment. -
Biochemical, Kinetic, and Computational Structural Characterization of Shikimate Kinase from Methicillin-Resistant Staphylococcus Aureus
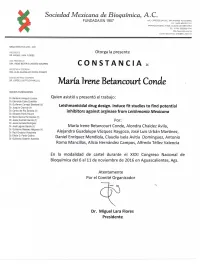
Otorgaa la presente C O N S T A N C I A a: Luis Enrique Pérez Del Castillo Quien asistió y presentó el trabajo: Exploring chemical space to find potential inhibitors of protein tyrosine phosphatase 1B Por: Luis Enrique Pérez del Castillo, Claudia Isela Avitia Domínguez, Marcelo Gómez‐Palacio Gastelum, Jorge Cisneros Martínez, Alfredo Téllez Valeencia En la modalidad de cartel durante el XXXII Congreso Nacional de Bioquímica 4 ‐ 9 de noviembre de 2018 en Ixtapa, Zihuatanejo, Gro. Atentamente Por el Comité Organizador Dra. Irene B. Castaño Navarro Presidente Send Orders for Reprints to [email protected] 260 Current Protein and Peptide Science, 2016, 17, 260-274 Targeting Plasmodium Metabolism to Improve Antimalarial Drug Design Claudia Avitia-Domínguez1, Erick Sierra-Campos2, Irene Betancourt-Conde1, Miriam Aguirre-Raudry1, Alejandra Vázquez-Raygoza1, Artemisa Luevano-De la Cruz1, Alejandro Favela-Candia1, Marie Sarabia-Sanchez1, Lluvia Ríos-Soto1, Edna Méndez-Hernández1, Jorge Cisneros-Martínez1, Marcelo Gómez Palacio-Gastélum3, Mónica Valdez-Solana2, Jessica Hernández-Rivera2, Jaime De Lira-Sánchez2, Mara Campos-Almazán2 and Alfredo Téllez-Valencia1,* 1Facultad de Medicina y Nutrición, Universidad Juárez del Estado de Durango, Av. Universidad y Fanny Anitua S/N, Durango. Dgo. México, C.P. 34000; 2Facultad de Ciencias Químicas, Universidad Juárez del Estado de Durango, Av. Artículo 123 S/N Fracc. Filadelfia, Gómez Palacio, Durango, CP. 35010, México; 3Facultad de Odontología, Universi- dad Juárez del Estado de Durango, Predio Canoas S/N, Colonia Los Ángeles, Durango. Dgo. México, C.P. 34070 Abstract: Malaria is one of the main infectious diseases in tropical developing countries and represents high morbidity and mortality rates nowadays. -

Florencio Zaragoza Dörwald Lead Optimization for Medicinal Chemists
Florencio Zaragoza Dorwald¨ Lead Optimization for Medicinal Chemists Related Titles Smith, D. A., Allerton, C., Kalgutkar, A. S., Curry, S. H., Whelpton, R. van de Waterbeemd, H., Walker, D. K. Drug Disposition and Pharmacokinetics and Metabolism Pharmacokinetics in Drug Design From Principles to Applications 2012 2011 ISBN: 978-3-527-32954-0 ISBN: 978-0-470-68446-7 Gad, S. C. (ed.) Rankovic, Z., Morphy, R. Development of Therapeutic Lead Generation Approaches Agents Handbook in Drug Discovery 2012 2010 ISBN: 978-0-471-21385-7 ISBN: 978-0-470-25761-6 Tsaioun, K., Kates, S. A. (eds.) Han, C., Davis, C. B., Wang, B. (eds.) ADMET for Medicinal Chemists Evaluation of Drug Candidates A Practical Guide for Preclinical Development 2011 Pharmacokinetics, Metabolism, ISBN: 978-0-470-48407-4 Pharmaceutics, and Toxicology 2010 ISBN: 978-0-470-04491-9 Sotriffer, C. (ed.) Virtual Screening Principles, Challenges, and Practical Faller, B., Urban, L. (eds.) Guidelines Hit and Lead Profiling 2011 Identification and Optimization ISBN: 978-3-527-32636-5 of Drug-like Molecules 2009 ISBN: 978-3-527-32331-9 Florencio Zaragoza Dorwald¨ Lead Optimization for Medicinal Chemists Pharmacokinetic Properties of Functional Groups and Organic Compounds The Author All books published by Wiley-VCH are carefully produced. Nevertheless, authors, Dr. Florencio Zaragoza D¨orwald editors, and publisher do not warrant the Lonza AG information contained in these books, Rottenstrasse 6 including this book, to be free of errors. 3930 Visp Readers are advised to keep in mind that Switzerland statements, data, illustrations, procedural details or other items may inadvertently be Cover illustration: inaccurate. -

Uva-DARE (Digital Academic Repository)
UvA-DARE (Digital Academic Repository) Peptidases in antigen processing and neurodegenerative diseases Raspe, M.A. Publication date 2011 Link to publication Citation for published version (APA): Raspe, M. A. (2011). Peptidases in antigen processing and neurodegenerative diseases. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:01 Oct 2021 CHAPTER 5 Exploring the role of endopeptidases in peptide degradation and antigen processing Metallo-endopeptidases degrade basic peptides and influence proteasome-independent HLA-A11 and HLA-A3 MhC class I presentation M.A. Raspe1 T. Le1 W. benckhuizen2 J.H. Kessler2 M.H.M. Heemskerk3 W.J. Drijfhout2 J. Neefjes4 E.A. Reits1# 1 Research Group