Mild Traumatic Brain Injury, Mtbi) and Considers Relevant Effects
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Agitation After Traumatic Brain Injury (TBI) Is the Most Frequently Observed Behavioral Problem and Is a Challenge to Care Providers
CHAPTER I INTRODUCTION Problem Statement Agitation after traumatic brain injury (TBI) is the most frequently observed behavioral problem and is a challenge to care providers. About one third of TBI patients exhibit agitation in the subacute stage of rehabilitation and during the posttraumatic amnesia (PTA) stage of recovery (Sandel & Mysiw, 1996; Weir, Doig, Fleming, Wiemers, & Zemljic, 2006). Agitation not only reduces the opportunity for patients to engage in rehabilitation but also becomes a major stressor for patients and their caregivers. Furthermore, a prolonged agitation period may reduce functional independence, induce a longer hospital stay, delay or prevent a return to work, and disturb family dynamics and community integration (Bogner, Corrigan, Fugate, Mysiw, & Clinchot, 2001; Brooke, Questad, Patterson, & Bashak, 1992; Citrome, 2002; Eslinger, 1995; Nott, Chapparo, & Baguley, 2006). Because there are many problems produced by agitation, dealing with agitation presents multiple challenges during rehabilitation after TBI. Although the prevalence and severity of agitated behavior following TBI has long been known, there is surprisingly little known about its management. One possible reason for this dearth of knowledge is that because patients are excluded from rehabilitation due 1 to their behavior, there is little chance to focus on agitation (Alderman, Knight, & Morgan, 1997). Among the current methods of intervention in many rehabilitation units, pharmacological intervention is the most likely to be used to manage agitation. Anticonvulsants, antidepressants, antipsychotics, beta-blockers, and neurostimulants are commonly used in agitated patients after TBI. Although pharmacological intervention can be beneficial, detrimental side effects can be more harmful than the untreated agitation symptoms. In addition, medication-induced drowsiness can interrupt patient participation in their therapies (Corrigan & Mysiw, 1988; Zafonte, 1997). -

Rock Album Discography Last Up-Date: September 27Th, 2021
Rock Album Discography Last up-date: September 27th, 2021 Rock Album Discography “Music was my first love, and it will be my last” was the first line of the virteous song “Music” on the album “Rebel”, which was produced by Alan Parson, sung by John Miles, and released I n 1976. From my point of view, there is no other citation, which more properly expresses the emotional impact of music to human beings. People come and go, but music remains forever, since acoustic waves are not bound to matter like monuments, paintings, or sculptures. In contrast, music as sound in general is transmitted by matter vibrations and can be reproduced independent of space and time. In this way, music is able to connect humans from the earliest high cultures to people of our present societies all over the world. Music is indeed a universal language and likely not restricted to our planetary society. The importance of music to the human society is also underlined by the Voyager mission: Both Voyager spacecrafts, which were launched at August 20th and September 05th, 1977, are bound for the stars, now, after their visits to the outer planets of our solar system (mission status: https://voyager.jpl.nasa.gov/mission/status/). They carry a gold- plated copper phonograph record, which comprises 90 minutes of music selected from all cultures next to sounds, spoken messages, and images from our planet Earth. There is rather little hope that any extraterrestrial form of life will ever come along the Voyager spacecrafts. But if this is yet going to happen they are likely able to understand the sound of music from these records at least. -
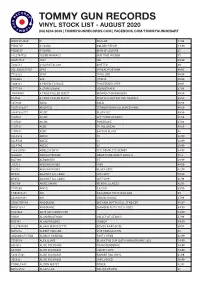
Vinyl Stock List - August 2020 (03) 6234 2039 | Tommygunrecords.Com | Facebook.Com/Tommygunhobart
TOMMY GUN RECORDS VINYL STOCK LIST - AUGUST 2020 (03) 6234 2039 | TOMMYGUNRECORDS.COM | FACEBOOK.COM/TOMMYGUNHOBART WARPLP302X !!! WALLOP 47.99 PIE027LP #1 DADS GOLDEN REPAIR 44.99 PIE005LP #1 DADS MAN OF LEISURE 35 8122794723 10,000 MANIACS OUR TIME IN EDEN 45 SSM144LP 1927 ISH 39.99 7202581 24 CARAT BLACK GHETTO 69 USI_B001655701 2PAC 2PACALYPSE NOW 49.95 7783828 2PAC THUG LIFE 49.99 FWR004 360 UTOPIA 49.99 5809181 A PERFECT CIRCLE THIRTEENTH STEP 49.95 6777554 A STAR IS BORN SOUNDTRACK 67.99 JIV41490.1 A TRIBE CALLED QUEST MIDNIGHT MARAUDERS 49.99 R14734 A TRIBE CALLED QUEST PEOPLE'S INSTINCTIVE TRAVELS 69.99 5351106 ABBA GOLD 49.99 19075850371 ABORTED TERRORVISION COLOURED VINYL 49.99 88697383771 AC/DC BLACK ICE 49.99 5107611 AC/DC LET THERE BE ROCK 41.99 5107621 AC/DC POWERAGE 47.99 5107581 ACDC 74 JAIL BREAK 49.99 5107651 ACDC BACK IN BLACK 45 XLLP313 ADELE 19 32.99 XLLP520 ADELE 21 32.99 XLLP740 ADELE 25 29.99 1866310761 ADOLESCENTS THE COMPLETE DEMOS 34.95 LL030LP ADRIAN YOUNGE SOMETHING ABOUT APRIL II 52.8 M27196 AEROSMITH ST 39.99 J12713 AFGHAN WHIGS 1965 49.99 P18761 AFGHAN WHIGS BLACK LOVE 42.99 OP048 AGAINST ALL LOGIC 2012-2017 59.99 OP053 AGAINST ALL LOGIC 2017-2019 61.99 S80109 AIMEE MANN MENTAL ILLNESS 42.95 7747280 AINTS 5,6,7,8,9 39.99 1.90296E+11 AIR CASANOVA 70 PIC DISC RSD 40 2438488481 AIR VIRGIN SUICIDE 37.99 SPINE799189 AIRBOURNE BREAKIN OUTTA HELL STND EDT 45.95 NW31135-1 AIRBOURNE DIAMOND CUTS THE B SIDES 44.99 FN279LP AK79 40TH ANNIV EDT 63.99 VS001 ALAN BRAUFMAN VALLEY OF SEARCH 47.99 M76741 ALAN PARSONS I -

Australian Literature and Music, 1945 to Present
The Space and Time of Imagined Sound: Australian Literature and Music, 1945 to Present Joseph Cummins A thesis in fulfillment of the requirements for the degree of Doctor of Philosophy School of Arts and Media Faculty of Arts and Social Sciences 2015 Acknowledgements Since I started as an undergraduate, Elizabeth McMahon and John Napier have inspired and guided my intellectual pathway. I’ll always remember John playing Bartok and Ravel, and Liz lecturing on Whitman and Tsiolkas. Without their encouragement, knowledge, discussion, editing skills and advice this project would not have taken place. Thank you both. Ashley Barnwell. Thank you for all your encouragement, inspiration, support, and love. You are my partner in crime, always willing to discuss, deconstruct, and argue. Thanks for your help in the last six months of this project, for pushing my writing, and for reading through the final copy. Alister Spence, Phil Slater and Helen Groth have been great and generous mentors to me during my time at UNSW. Thank you for your encouragement and advice. A particular thank you to Al and Phil, from whom I learnt so much. Thanks to my family, my music family, ASAL, AAL, IASPM, CMSA, Maroubra, Sydney Roosters, and International Grammar School. For sparking my love of the literary and historical, and for her encouragement, example of open mindedness and discussion, and genuine interest in my work, this thesis is dedicated to Nan Colleen. Abstract This thesis examines the space and time of imagined sound in Australian post-World War Two literature and music. Using what I term a critical close listening methodology, I will discuss a range of novels, poems, songs, song suites, film clips and art music compositions that, through a return to various times in the past, offer a remapping of Australian space. -

2SM Charts, 1979-09-14 to 1980-08-01
117 THE 25M HOT 100 „ 4,044,44440 41340 04 Vt1141, kratitrt tvikko ,,,- SEPTEMBER 14, 1979 LEGEND: * BULB • GOLD A PLATINUM II* NEW ENTRY 32 26 10 U.K. SQUEEZE 1 2 12 ELECTRIC LIGHT ORCHESTRA 1 1 6 A, MY SHARONA 32' 41 4__A_ THE MAIN EVENT/FIGHT Al` Discovery Cool For Cats A, The Knack W Barbra Streisand 33 23 9 ROBERT PALMER A LED ZEPPELIN 2 3 11 Ab I WAS MADE FOR LOVIN' YOU 33 - 1_,_LAHIGHVVAY TO HELL Secrets 2 1 3 In Through The Out Door w Kiss AC/DC 34 33 17 A ABBA 3 3 6 AA THE KNACK 3 2 12 A SOME GIRLS 34 - 1 I DON'T LIKE MONDAYS A Voulez-Vous IP Get The Knack Racey "Ir Boomtown Rats 35 37 14 JOE JACKSON 35 37 5 A, HOORAY HOORAY. IT'S A HOLI 4 — .L.ApP B DYLAN Look Sharp! 4 6 5UP THERE CAZALY S/ow Train Coming A V. Boney M -HOLIDAY 36 — 1 .4JOAN ARMATRADING A The Two Man Band SUPE RTRAMP 36 34 8 LONESOME LOSER P‘Steppin` Out 5 7 13, YOU CAN'T CHANGE THAT 5 5 25 Breakfast in America Raydio Little River Band 37 — 1 4.-XTC 37 21 19 A, HOT STUFF 6 7 16 LEO SAYER 4 Drums and Wires 6 9 7 GOLD The Very Best Of Leo Sayer John Stewart w Donna Summer 38 40 2 NILS LOFGREN 38 25 15 IS SHE REALLY GOING OUT WITH LE RIVER BAND Nils 7 5 9 REUNITED 7 6 8 • FL rsT-r t Under The Wire Peaches & Herb Joe Jackson HIM? 39 25 17 A DEMIS ROUSSOS 39 - 1 __AXE DON'T TALK ANYMORE JON ENGLISH Forever And Ever 8 4 10 A, RING MY BELL ♦"iP 8 4 9 A English History W Anita Ward Cliff Richard 40 49 2 CHRIS DE BURGH 40 22 16 BOOGIE WONDERLAND 9 8 11 A KISS 1 Crusader 9 12 14COOLAA FOR CATS • Dyansty U.K. -
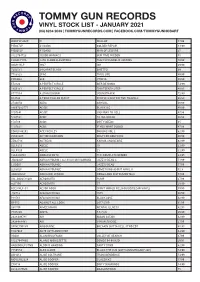
Vinyl Stock List - January 2021 (03) 6234 2039 | Tommygunrecords.Com | Facebook.Com/Tommygunhobart
TOMMY GUN RECORDS VINYL STOCK LIST - JANUARY 2021 (03) 6234 2039 | TOMMYGUNRECORDS.COM | FACEBOOK.COM/TOMMYGUNHOBART WARPLP302X !!! WALLOP 47.99 PIE027LP #1 DADS GOLDEN REPAIR 44.99 PIE005LP #1 DADS MAN OF LEISURE 35 8122794723 10,000 MANIACS OUR TIME IN EDEN 45 CHARLY111L 13TH FLOOR ELEVATORS THE PSYCHEDELIC SOUNDS 49.99 SSM144LP 1927 ISH 39.99 7202581 24 CARAT BLACK GHETTO 69 7783828 2PAC THUG LIFE 49.99 FWR004 360 UTOPIA 49.99 E52120 A PERFECT CIRCLE MER DE NOMS 54.99 5809181 A PERFECT CIRCLE THIRTEENTH STEP 49.95 6777554 A STAR IS BORN SOUNDTRACK 72.99 R14734 A TRIBE CALLED QUEST PEOPLE'S INSTINCTIVE TRAVELS 69.99 2734650 ABBA ARRIVAL 49.99 88697383771 AC/DC BLACK ICE 49.99 5107641 AC/DC HIGHWAY TO HELL 47.99 5107581 ACDC 74 JAIL BREAK 49.99 150586 ACDC DIRTY DEEDS 45 5107631 ACDC IF YOU WANT BLOOD 47.99 EOMLP46292 ACE FREHLEY ORIGINS VOL 2 62.99 LVR01365 ACTION BRONSON ONLY FOR DOLPHINS 49.99 ZEN271X ACTRESS KARMA AND DESIRE 62.99 XLLP313 ADELE 19 32.99 XLLP520 ADELE 21 32.99 1866310761 ADOLESCENTS THE COMPLETE DEMOS 34.95 JID003LP ADRIAN YOUNG / ALI SHAH MUHAMMAD JAZZ IS DEAD 3 51.99 LJID001 ADRIAN YOUNGE JAZZ IS DEAD 57.99 LL030LP ADRIAN YOUNGE SOMETHING ABOUT APRIL II 52.8 4AD0302LP ADRIANNE LENKER SONGS AND INSTRUMENTALS 57.99 USI_B002518301 AEROSMITH PUMP 37.99 m27196 AEROSMITH ST 39.99 RSE314LP-C1 AESOP ROCK SPIRIT WORLD FIELD GUIDE(CLEAR VINYL) 59.99 J12713 AFGHAN WHIGS 1965 49.99 P18761 AFGHAN WHIGS BLACK LOVE 42.99 OP053 AGAINST ALL LOGIC 2017-2019 61.99 S80109 AIMEE MANN MENTAL ILLNESS 42.95 7747280 AINTS 5,6,7,8,9 39.99 -

Midnight Oil Head Injuries Mp3, Flac, Wma
Midnight Oil Head Injuries mp3, flac, wma DOWNLOAD LINKS (Clickable) Genre: Other Album: Head Injuries Country: Australia Released: 1979 MP3 version RAR size: 1733 mb FLAC version RAR size: 1802 mb WMA version RAR size: 1136 mb Rating: 4.8 Votes: 301 Other Formats: ASF MOD DTS MP1 FLAC AIFF DXD Tracklist A1 Cold Cold Change 3:29 A2 Section 5 (Bus To Bondi) 2:58 A3 Naked Flame 3:28 A4 Back On The Borderline 3:09 A5 Koala Sprint 5:10 B1 No Reaction 2:56 B2 Stand In Line 4:46 B3 Profiteers 3:44 B4 Is It Now? 4:24 Companies, etc. Manufactured By – RCA Limited Distributed By – RCA Limited Made By – 7 Records Pty Limited Recorded At – Trafalgar Studios Mastered At – EMI Studios 301 Published By – Sprint Music Published By – Rondor Credits Artwork [Album Concept Management] – Midnight Oil Bass, Backing Vocals – Andrew James Drums, Backing Vocals – Rob Hirst Engineer – Peter J. Walker* Guitar – Martin Rotsey Guitar, Keyboards – Jim Moginie Management – Gary Morris Mastered By – Richard Mott Photography By – Philip Morris Producer – Leszek J. Karski* Vocals – Peter Garrett Written-By – James* (tracks: A4), Moginie* (tracks: A1 to A3, A5 to B4), Rotsey* (tracks: A2, A3, A5 to B3), Garrett* (tracks: A2, A4, A5, B2, B4), Hirst* (tracks: A1 to A4, B1 to B3) Notes Released in an outer sleeve, and an inner sleeve with a photo montage of gig posters on one side, and tracklisting, lyrics and credits on the other. This release has slight differences in artwork from another similar release: - there are LP and cassette catalog no.s on the upper right corner of the rear of the outer sleeve of this release (it appears these have been erased from the sleeve on the other version by some manipulation of the image) - "10/79/BC" is in the bottom left hand corner of the rear of the outer sleeve of this release - on this release the side B label layout is different (and is generally the same as the side A label layout of the other version), as follows: there is no matrix no.; the catalog no.