Histamine Intolerance: the Current State of the Art
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Neurotransmitter Resource Guide
NEUROTRANSMITTER RESOURCE GUIDE Science + Insight doctorsdata.com Doctor’s Data, Inc. Neurotransmitter RESOURCE GUIDE Table of Contents Sample Report Sample Report ........................................................................................................................................................................... 1 Analyte Considerations Phenylethylamine (B-phenylethylamine or PEA) ................................................................................................. 1 Tyrosine .......................................................................................................................................................................................... 3 Tyramine ........................................................................................................................................................................................4 Dopamine .....................................................................................................................................................................................6 3, 4-Dihydroxyphenylacetic Acid (DOPAC) ............................................................................................................... 7 3-Methoxytyramine (3-MT) ............................................................................................................................................... 9 Norepinephrine ........................................................................................................................................................................ -

Headache Is One of the Most Common Complaints Voiced in a Doctor's
Headache is one of the most common complaints voiced in a doctor’s examination room. Many of these headaches are "benign" in the sense that they are brought on by stress or anxiety, the amount of discomfort is mild to moderate, and relief is achieved withi n a few hours. A second type of headache occurs secondary to a medical illnesses, usually a minor condition such as the flu. Only in rare cases are these headaches a sign of serious conditions such as cerebral aneurysms or strokes. A third type of headache , affecting 10 - 20% of the population, is a migraine (1). Migraines consist of periodic attacks of hemicranial pain, vomiting, photophobia, phonophobia, tiredness, irritability, and impaired concentration. In the case of a classical migraine, the headache itself is preceded by an "aura" consisting of visual problems, generally blind spots or hallucinations. A common migraine contains no premonitory aura (2). Several hypothesis have been proposed to account for the various features of a migraine, yet no cle ar mechanism exists to explain why or how a migraine headache occurs. Certain foods, such as chocolate, wine, and cheese, have been suspected of initiating migraines. It is the purpose of this paper to evaluate the evidence for dietary triggers of migraine s, suggest a mechanism by which specific molecules in food could induce a migraine, and make recommendations regarding dietary treatment for migraine sufferers. Research on the Role of Food in Migraine Headaches Studies implicating food in the pathogene sis of migraines date back to the 1920’s when researchers began to examine and manipulate the diets of individuals suffering from migraines. -

Diphenhydramine Hydrochloride (CASRN 147-24-0) in F344/N Rats
NATIONAL TOXICOLOGY PROGRAM Technical Report Series No. 355 TOXICOLOGY AND CARCINOGENESIS STUDIES OF DIPHENHYDRAMINE HYDROCHLORIDE (CAS NO. 147-24-0) IN F344/N RATS AND B6C3F1 MICE (FEED STUDIES) LJ.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutes of Health NTP ‘TECHNICAL REPORT ON THE TOXICOLOGY AND CARCINOGENESIS STUDIES OF DIPHENHYDRAMINE HYDROCHLORIDE (CAS NO. 147-24-0) IN F344/N RATS AND B6C3F1 MICE (FEED STUDIES) R. Melnick, Ph.D., Study Scientist NATIONAL TOXICOLOGY PROGRAM P.O. Box 12233 Research Triangle Park, NC 27709 September 1989 NTP TR 355 NIH Publication No. 89-2810 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutes of Health CONTENTS PAGE ABSTRACT ................................................................ 3 EXPLANATION OF LEVELS OF EVIDENCE OF CARCINOGENIC ACTIVITY .................. 6 CONTRIBUTORS ............................................................ 7 PEERREVIEWPANEL ........................................................ 8 SUMMARY OF PEER REVIEW COMMENTS ......................................... 9 I. INTRODUCTION ........................................................ 11 I1. MATERIALS AND METHODS .............................................. 21 III. RESULTS ............................................................. 35 RATS ............................................................. 36 MICE ............................................................. 45 GENETIC TOXICOLOGY ............................................... 53 IV. -
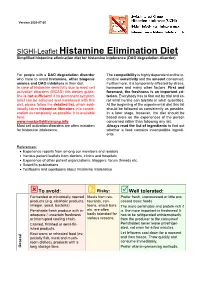
SIGHI-Leaflet Histamine Elimination Diet Simplified Histamine Elimination Diet for Histamine Intolerance (DAO Degradation Disorder)
Version 2020-07-20 SIGHI-Leaflet Histamine Elimination Diet Simplified histamine elimination diet for histamine intolerance (DAO degradation disorder) For people with a DAO degradation disorder The compatibility is highly dependent on the in- who have to avoid histamine, other biogenic dividual sensitivity and the amount consumed. amines and DAO inhibitors in their diet. Furthermore, it is temporarily affected by stress, In case of histamine sensitivity due to mast cell hormones and many other factors. First and activation disorders (MCAD) this dietary guide- foremost, the freshness is an important cri- line is not sufficient! If no permanent symptom terion. Everybody has to find out by trial and er- relief can be achieved and maintained with this ror what he/she can tolerate in what quantities. diet, please follow the detailed list, which addi- At the beginning of the experimental diet this list tionally takes histamine liberators into consid- should be followed as consistently as possible. eration as completely as possible. It is available In a later stage, however, the diet should be here: based more on the experiences of the person www.mastzellaktivierung.info concerned rather than following any list. Mast cell activation disorders are often mistaken Always read the list of ingredients to find out for histamine intolerance. whether a food contains incompatible ingredi- ents. References: • Experience reports from among our members and readers • Various patient leaflets from doctors, clinics and hospitals • Experience of other patient organizations, bloggers, forum threads etc. • Scientific publications • Textbooks and cookbooks about histamine intolerance To avoid: ? Risky: Well tolerated: Fermented or microbially ripened Meals from res- Prefer fresh, unprocessed or little pro- products (e.g. -

Role of Dietary Histidine in the Prevention of Obesity and Metabolic Syndrome
Open access Editorial Open Heart: first published as 10.1136/openhrt-2017-000676 on 1 July 2018. Downloaded from Role of dietary histidine in the prevention of obesity and metabolic syndrome James J DiNicolantonio,1 Mark F McCarty,2 James H OKeefe 1 To cite: DiNicolantonio JJ, HISTIDINE SUPPLEMENTATION AMELIORATES histidine dose dependently increases hypo- McCarty MF, OKeefe JH. Role of METABOLIC SYNDROME thalamic levels of histamine as well as hypo- dietary histidine in the prevention of obesity and A recent Chinese supplementation study, in thalamic activity of histidine decarboxylase, metabolic syndrome. Open Heart which obese middle-aged women diagnosed the enzyme which converts histidine to hista- 10 2018;5:e000676. doi:10.1136/ with metabolic syndrome received 12 weeks mine. Such administration also inhibits food openhrt-2017-000676 of supplemental histidine (2 g, twice daily) or consumption—an effect that is blocked in matching placebo, achieved remarkable find- animals pretreated with an irreversible inhib- 1 Accepted 24 April 2018 ings. Insulin sensitivity improved significantly itor of histidine decarboxylase. in the histidine-supplemented subjects, and Neuronal histamine release in the hypo- this may have been partially attributable to thalamus is subject to feedback regulation loss of body fat. Body mass index (BMI), waist by presynaptic H3 receptors. In rodent circumference and body fat declined in the studies, antagonists and inverse agonists for histidine-supplemented group relative to the these receptors have been shown to mark- placebo group; the average fat loss in the histi- edly amplify hypothalamic histamine levels, dine group was a robust 2.71 kg. Markers of suppress feeding, decrease body weight and systemic inflammation such as serum tumour enhance metabolic rate.11–15 Such agents may necrosis factor-alpha (TNF-α) and inter- have clinical potential for managing obesity. -

THE USE of MIRTAZAPINE AS a HYPNOTIC O Uso Da Mirtazapina Como Hipnótico Francisca Magalhães Scoralicka, Einstein Francisco Camargosa, Otávio Toledo Nóbregaa
ARTIGO ESPECIAL THE USE OF MIRTAZAPINE AS A HYPNOTIC O uso da mirtazapina como hipnótico Francisca Magalhães Scoralicka, Einstein Francisco Camargosa, Otávio Toledo Nóbregaa Prescription of approved hypnotics for insomnia decreased by more than 50%, whereas of antidepressive agents outstripped that of hypnotics. However, there is little data on their efficacy to treat insomnia, and many of these medications may be associated with known side effects. Antidepressants are associated with various effects on sleep patterns, depending on the intrinsic pharmacological properties of the active agent, such as degree of inhibition of serotonin or noradrenaline reuptake, effects on 5-HT1A and 5-HT2 receptors, action(s) at alpha-adrenoceptors, and/or histamine H1 sites. Mirtazapine is a noradrenergic and specific serotonergic antidepressive agent that acts by antagonizing alpha-2 adrenergic receptors and blocking 5-HT2 and 5-HT3 receptors. It has high affinity for histamine H1 receptors, low affinity for dopaminergic receptors, and lacks anticholinergic activity. In spite of these potential beneficial effects of mirtazapine on sleep, no placebo-controlled randomized clinical trials of ABSTRACT mirtazapine in primary insomniacs have been conducted. Mirtazapine was associated with improvements in sleep on normal sleepers and depressed patients. The most common side effects of mirtazapine, i.e. dry mouth, drowsiness, increased appetite and increased body weight, were mostly mild and transient. Considering its use in elderly people, this paper provides a revision about studies regarding mirtazapine for sleep disorders. KEYWORDS: sleep; antidepressive agents; sleep disorders; treatment� A prescrição de hipnóticos aprovados para insônia diminuiu em mais de 50%, enquanto de antidepressivos ultrapassou a dos primeiros. -

Brucellosis in Humans – Etiology, Diagnostics, Clinical Forms
Annals of Agricultural and Environmental Medicine 2013, Vol 20, No 2, 233–238 REVIEW ARTICLE www.aaem.pl Brucellosis in humans – etiology, diagnostics, clinical forms Elżbieta Monika Galińska1, Jerzy Zagórski2 1 Department of Allergology and Environmental Hazards, Institute of Rural Health, Lublin, Poland 2 Department of Public Health, Institute of Rural Health, Lublin, Poland Galińska EM, Zagórski J. Brucellosis in humans – etiology, diagnostics, clinical forms. Ann Agric Environ Med. 2013; 20(2): 233–238. Abstract Brucellosis in humans is a zoonosis of greatly varied clinical image. It occurs on all inhabited continents. The course of the disease may be acute, sub-acute or chronic. The etiologic factors of brucellosis are small, aerobic Gram-negative rods of the genus Brucella, which currently contains ten species: B. abortus, B. suis, B. ovis, B. melitensis, B. canis, B. neotomae, B. pinnipedialis, B. ceti, B. microti and B. inopinata. In humans, the disease is caused mainly by: B. melitensis as the most pathogenic species, followed by B. suis, whereas B. abortus is considered as the mildest type of brucellosis. The natural reservoir of the germ and the source of infection in humans are infected domestic animals, primarily cattle, sheep, goats, as well as wild animals. Infection in humans occurs by penetration through damaged skin, conjunctiva, and more rarely via the alimentary route by the consumption of infected products. Especially exposed are: veterinarians, veterinary technicians, insemination service employees, zoo technicians, -

Histamine and Gut Mucosal Immune Regulation S
Allergy REVIEW ARTICLE Histamine and gut mucosal immune regulation S. Smolinska1,2, M. Jutel1,2, R. Crameri3 & L. O’Mahony3 1Department of Clinical Immunology, Wroclaw Medical University, Wroclaw; 2‘ALL-MED’ Medical Research Institute, Wroclaw, Poland; 3Swiss Institute of Allergy and Asthma Research, University of Zurich, Davos, Switzerland To cite this article: Smolinska S, Jutel M, Crameri R, O’Mahony L. Histamine and gut mucosal immune regulation. Allergy 2013; DOI: 10.1111/all.12330. Keywords Abstract allergy; histamine; inflammation; microbial Histamine is a biogenic amine with extensive effects on many cell types, mediated metabolites; mucosal immunology. by the activation of its four receptors (H1R–H4R). Distinct effects are dependent Correspondence on receptor subtypes and their differential expression. Within the gastrointestinal Dr. Liam O’Mahony, SIAF, Obere Strasse tract, histamine is present at relatively high concentrations, particularly during 22, 7270 Davos Platz, Switzerland. inflammatory responses. In this review, we discuss the immunoregulatory influ- Tel.: +41-81-4100853 ence of histamine on a number of gastrointestinal disorders, including food Fax: +41-81-4100840 allergy, scombroid food poisoning, histamine intolerance, irritable bowel syn- E-mail: [email protected] drome, and inflammatory bowel disease. It is clear that the effects of histamine on mucosal immune homeostasis are dependent on expression and activity of the Accepted for publication 21 October 2013 four currently known histamine receptors; however, the relative protective or pathogenic effects of histamine on inflammatory processes within the gut are still DOI:10.1111/all.12330 poorly defined and require further investigation. Edited by: Hans-Uwe Simon Histamine [2-(4-imidazolyl)-ethylamine] is a short-acting studies demonstrate the influence of histamine on wound endogenous amine, which is widely distributed throughout healing, circulatory disease, immunology, oncology, and the body (1, 2). -

(DNCB) and Respiratory Allergy in the Th2-Prone Brown Norway Rat C
Available online at www.sciencedirect.com Toxicology 246 (2008) 213–221 The contact allergen dinitrochlorobenzene (DNCB) and respiratory allergy in the Th2-prone Brown Norway rat C. Frieke Kuper a,∗, Rob H. Stierum a, Andre Boorsma a,b, Marcel A. Schijf a, Menk Prinsen a, Joost P. Bruijntjes a, Nanne Bloksma c, Josje H.E. Arts a a TNO, Quality of Life, Zeist, The Netherlands b Department of Health Risk Analysis and Toxicology, Maastricht University, Maastricht, The Netherlands c Subfaculty of Biology, Faculty of Science, Utrecht University, The Netherlands Received 30 October 2007; received in revised form 21 December 2007; accepted 21 January 2008 Available online 2 February 2008 Abstract All LMW respiratory allergens known to date can also induce skin allergy in test animals. The question here was if in turn skin allergens can induce allergy in the respiratory tract. Respiratory allergy was tested in Th2-prone Brown Norway (BN) rats by dermal sensitization with the contact allergen dinitrochlorobenzene (DNCB; 1%, day 0; 0.5%, day 7) and a head/nose-only inhalation challenge of 27 mg/m3 of DNCB (15 min, day 21), using a protocol that successfully identified chemical respiratory allergens. Skin allergy to DNCB was examined in BN rats and Th1-prone Wistar rats in a local lymph node assay followed by a topical patch challenge of 0.1% DNCB. Sensitization of BN rats via the skin induced DNCB-specific IgG in serum, but not in all animals, and an increased number of CD4+ cells in the lung parenchyma. Subsequent inhalation challenge with DNCB did not provoke apneas or allergic inflammation (signs of respiratory allergy) in the BN rats. -

Effects of the Inhibitor of Glutamate Decarboxylase on the Development
RSC Advances View Article Online PAPER View Journal | View Issue Effects of the inhibitor of glutamate decarboxylase on the development and GABA accumulation in Cite this: RSC Adv.,2018,8,20456 germinating fava beans under hypoxia-NaCl stress Yongqi Yin, Chao Cheng and Weiming Fang* Glutamate decarboxylase (GAD) is the key enzyme in GABA shunt, which catalyzes the a-decarboxylation of glutamate to produce GABA. A specific inhibitor for GAD is convenient to study the dynamic balances of GABA metabolism in plants. The inhibitor of GAD in germinated fava beans was screened, and its inhibitory effect on the growth and GABA accumulation in fava beans during germination under hypoxia- NaCl stress was investigated. The inhibitory effect of aminoxyacetate for fava bean GAD was better than those of other chemicals, and it increased with the increase in concentration in vivo. After aminoxyacetate (5 mM) application for 4 days during germination, the GAD activity in germinating fava beans was significantly inhibited by more than 90% in both organs. Meanwhile, the growth of fava bean Creative Commons Attribution-NonCommercial 3.0 Unported Licence. sprouts was also slightly suppressed. Moreover, the GABA contents decreased by 43.9% and 81.5% in a 4 Received 8th May 2018 day-old cotyledon and embryo, respectively, under aminoxyacetate treatment compared with that in the Accepted 23rd May 2018 control. In summary, these results showed that aminoxyacetate can serve as a specific inhibitor of GAD DOI: 10.1039/c8ra03940b in plants. At least 43.9% and 81.5% of GABA in germinating fava beans under hypoxia-NaCl stress were rsc.li/rsc-advances synthesized via GABA shunt. -

Convenient Preparation of Poly(L-Histidine) by the Direct Polymerization of L-Histidine Or Nim Benzyl-L-Histidine with Diphenylphosphoryl Azide
Polymer Journal, Vol. 13, No. 12, pp 1151-1154 (1981) SHORT COMMUNICATION Convenient Preparation of Poly(L-histidine) by the Direct Polymerization of L-Histidine or Nim_Benzyl-L-histidine with Diphenylphosphoryl Azide Takumi NARUSE, Bun-ichiro NAKAJIMA, Akihiro TSUTSUMI, and Norio NISHI Department of Polymer Science, Faculty of Science, Hokkaido University, Nishi 8-chome, Kita 10-jo, Kita-ku, Sapporo 060, Japan. (Received August 14, 1981) KEY WORDS Polymerization I Diphenylphosphoryl Azide (DPPA) I L- Histidine I N'm-Benzyl-L-histidine I Poly(L-histidine) I Poly(N'm-benzyl-L histidine) I IR Spectrum I 13C NMR Spectrum I Intrinsic Viscosity I Poly(L-histidine) is a very interesting poly(a histidine) by the polymerization of L-histidine with amino acid) as a synthetic functional polymer or as iodine-phosphonic acid esters was unsuccessful. The a model for the functional biopolymer such as simplification of the synthetic route for poly(L enzymes. It is known, however, that poly(L histidine) is still necessary. histidine) can not be prepared by the Fuchs Diphenylphosphoryl azide (DPPA) has been used Farthing method 1 which is very popular for prepar as a convenient reagent for racemization-free pep ing poly(a-amino acid)s. A synthetic route with tide synthesis, since it was synthesized by Shioiri et several steps involving the synthesis of NCA (a a!. in 1972.6 Recently, we reported that this reagent amino acid N-carboxyanhydride) by the rather can also be used successfully for the polymerization classical Leuchs method/ have been used for the of amino acids or peptides. -

(Trouessart) and D. Farinae Hughes (Acari: Pyroglyphidae) Sensitivity in Patients with Allergic Rhinitis: a Comparative Study
Systematic & Applied Acarology 23(2): 404–404 (2018) ISSN 1362-1971 (print); http://dx.doi.org/10.11158/saa.23.2.17 ISSN 2056-6069 (online) Erratum Correction: Evaluation of Dermatophagoides pteronyssinus (Trouessart) and D. farinae Hughes (Acari: Pyroglyphidae) sensitivity in patients with allergic rhinitis: a comparative study ERHAN ZEYTUN1*, SALİH DOĞAN1, EDHEM ÜNVER2 & FATİH ÖZÇİÇEK3 1 Department of Biology, Arts & Sciences Faculty, Erzincan University, Erzincan, Turkey 2 Department of Chest Disease, Erzincan University School of Medicine, Erzincan, Turkey 3 Department of Internal Medicine, Erzincan University School of Medicine, Erzincan, Turkey * Corresponding author: [email protected] The authors are sorry that they made a mistake in spelling the family name of the first author on line 4 of page 206 in Zeytun et al. (2018): EYTUN should be ZEYTUN. This type error is evident in the paper itself because the running title in the footer of page 207 has the correct name: “ZEYTUN ET AL.: SENSITIVITY TO HDMS IN PATIENTS WITH ALLERGIC RHINITIS”. Reference Zeytun1, E., Doğan, S., Ünver, E. & Özçiçek, F. (2018) Evaluation of Dermatophagoides pteronys- sinus (Trouessart) and D. farinae Hughes (Acari: Pyroglyphidae) sensitivity in patients with allergic rhinitis: a comparative study. Systematic & Applied Acarology, 23(2), 206–215. https://doi.org/10.11158/saa.23.2.2 Published: 22 Feb. 2018 1. Not “Eytun” 404 © Systematic & Applied Acarology Society Systematic & Applied Acarology 23(2): 206–215 (2018) ISSN 1362-1971 (print) http://doi.org/10.11158/saa.23.2.2