Alterations in Ventilation-Perfusion Relationships in the Lung After
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Correlation Between Tidal Volume Measured by Spirometry and Impedance Pneumography
New Jersey Institute of Technology Digital Commons @ NJIT Theses Electronic Theses and Dissertations Fall 10-31-1994 Correlation between tidal volume measured by spirometry and impedance pneumography Krithika Seshadri New Jersey Institute of Technology Follow this and additional works at: https://digitalcommons.njit.edu/theses Part of the Biomedical Engineering and Bioengineering Commons Recommended Citation Seshadri, Krithika, "Correlation between tidal volume measured by spirometry and impedance pneumography" (1994). Theses. 1696. https://digitalcommons.njit.edu/theses/1696 This Thesis is brought to you for free and open access by the Electronic Theses and Dissertations at Digital Commons @ NJIT. It has been accepted for inclusion in Theses by an authorized administrator of Digital Commons @ NJIT. For more information, please contact [email protected]. Copyright Warning & Restrictions The copyright law of the United States (Title 17, United States Code) governs the making of photocopies or other reproductions of copyrighted material. Under certain conditions specified in the law, libraries and archives are authorized to furnish a photocopy or other reproduction. One of these specified conditions is that the photocopy or reproduction is not to be “used for any purpose other than private study, scholarship, or research.” If a, user makes a request for, or later uses, a photocopy or reproduction for purposes in excess of “fair use” that user may be liable for copyright infringement, This institution reserves the right to refuse to -

Hypothermia Brochure
Visit these websites for more water safety and hypothermia prevention in- formation. What is East Pierce Fire & Rescue Hypothermia? www.eastpiercefire.org Hypothermia means “low temperature”. Washington State Drowning When your body is exposed to cold tem- Prevention Coalition Hypothermia www.drowning-prevention.org perature, it tries to protect itself by keeping a normal body temperature of 98.6°F. It Children’s Hospital & tries to reduce heat loss by shivering and Regional Medical Center In Our Lakes moving blood from your arms and legs to www.seattlechildrens.org the core of your body—head, chest and and Rivers abdomen. Hypothermia Prevention, Recognition and Treatment www.hypothermia.org Stages of Hypothermia Boat Washington Mild Hypothermia www.boatwashington.org (Core body temperature of 98.6°— 93.2°F) Symptoms: Shivering; altered judg- ment; numbness; clumsiness; loss of Boat U.S. Foundation dexterity; pain from cold; and fast www.boatus.com breathing. Boat Safe Moderate Hypothermia www.boatsafe.com (Core body temperature of 93.2°—86°F) Symptoms: Semiconscious to uncon- scious; shivering reduced or absent; lips are blue; slurred speech; rigid n in muscles; appears drunk; slow Eve breathing; and feeling of warmth can occur. mer! Headquarters Station Sum Severe Hypothermia 18421 Old Buckley Hwy (Core body temperature below 86°F) Bonney Lake, WA 98391 Symptoms: Coma; heart stops; and clinical death. Phone: 253-863-1800 Fax: 253-863-1848 Email: [email protected] Know the water. Know your limits. Wear a life vest. By choosing to swim in colder water you Waters in Western Common Misconceptions Washington reduce your survival time. -

Maximum Expiratory Flow Rates in Induced Bronchoconstriction in Man
Maximum expiratory flow rates in induced bronchoconstriction in man A. Bouhuys, … , B. M. Kim, A. Zapletal J Clin Invest. 1969;48(6):1159-1168. https://doi.org/10.1172/JCI106073. Research Article We evaluated changes of maximum expiratory flow-volume (MEFV) curves and of partial expiratory flow-volume (PEFV) curves caused by bronchoconstrictor drugs and dust, and compared these to the reverse changes induced by a bronchodilator drug in previously bronchoconstricted subjects. Measurements of maximum flow at constant lung inflation (i.e. liters thoracic gas volume) showed larger changes, both after constriction and after dilation, than measurements of peak expiratory flow rate, 1 sec forced expiratory volume and the slope of the effort-independent portion of MEFV curves. Changes of flow rates on PEFV curves (made after inspiration to mid-vital capacity) were usually larger than those of flow rates on MEFV curves (made after inspiration to total lung capacity). The decreased maximum flow rates after constrictor agents are not caused by changes in lung static recoil force and are attributed to narrowing of small airways, i.e., airways which are uncompressed during forced expirations. Changes of maximum expiratory flow rates at constant lung inflation (e.g. 60% of the control total lung capacity) provide an objective and sensitive measurement of changes in airway caliber which remains valid if total lung capacity is altered during treatment. Find the latest version: https://jci.me/106073/pdf Maximum Expiratory Flow Rates in Induced Bronchoconstriction in Man A. Bouiuys, V. R. HuNTr, B. M. Kim, and A. ZAPLETAL From the John B. Pierce Foundation Laboratory and the Yale University School of Medicine, New Haven, Connecticut 06510 A B S T R A C T We evaluated changes of maximum ex- rates are best studied as a function of lung volume. -

The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board
The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board Introduction • Nitrogen makes up 78% of the air we breath; because of this it is often assumed that nitrogen is not hazardous. • However, nitrogen is safe to breath only if it is mixed with an appropriate amount of oxygen. • Additional nitrogen (lower oxygen) cannot be detected by the sense of smell. Introduction • Nitrogen is used commercially as an inerting agent to keep material free of contaminants (including oxygen) that may corrode equipment, present a fire hazard, or be toxic. • A lower oxygen concentration (e.g., caused by an increased amount of nitrogen) can have a range of effects on the human body and can be fatal if if falls below 10% Effects of Oxygen Deficiency on the Human Body Atmospheric Oxygen Concentration (%) Possible Results 20.9 Normal 19.0 Some unnoticeable adverse physiological effects 16.0 Increased pulse and breathing rate, impaired thinking and attention, reduced coordination 14.0 Abnormal fatigue upon exertion, emotional upset, faulty coordination, poor judgment 12.5 Very poor judgment and coordination, impaired respiration that may cause permanent heart damage, nausea, and vomiting <10 Inability to move, loss of consciousness, convulsions, death Source: Compressed Gas Association, 2001 Statistics on Incidents CSB reviewed cases of nitrogen asphyxiation that occurred in the US between 1992 and 2002 and determined the following: • 85 incidents of nitrogen asphyxiation resulted in 80 deaths and 50 injuries. • The majority of -

Introduction to Airway Resistance Measurements
Introduction to airway resistance measurements Dr. David Kaminsky Department of Medicine The University of Vermont VT 05405 Burlington UNITED STATES OF AMERICA [email protected] AIMS Review physiology of airway resistance Survey measures of airway resistance Provide examples of clinical applications Highlight research applications SUMMARY Airway resistance (Raw) is one of the fundamental features of the mechanics of the respiratory system. While the flow-volume loop offers insight into the volume and flow of air, it is limited in terms of specific information regarding lung mechanics. Airway resistance is the ratio of driving pressure divided by flow through the airways. It specifies the pressure required to achieve a flow of air with a velocity of 1L/sec. If the airway is represented by a simple, rigid tube, with laminar flow of air through it, the airway resistance Raw = (8 x L x )/ r4, where L = length of the tube, = viscosity of the gas, and r = radius of the tube. It is important to note that the r4 relationship demonstrates how sensitive resistance is to the size of the tube, varying inversely with the 4th power of the radius. The inner diameter of the airway is itself determined by many factors, including airway smooth muscle contractile state, airway wall thickness (related to inflammation, edema and remodeling), airway wall buckling and formation of mucosal folds, the interdependence, or linkage, of airway and surrounding lung parenchyma, and the intrinsic elastic recoil of the lung parenchyma, which serves as a load on the airway and variably resists bronchoconstriction. Of course, the airways are not rigid tubes, and in fact flow is a complex process involving both laminar and turbulent conditions, so this calculation of Raw is an approximation only. -

Den170044 Summary
DE NOVO CLASSIFICATION REQUEST FOR CLEARMATE REGULATORY INFORMATION FDA identifies this generic type of device as: Isocapnic ventilation device. An isocapnic ventilation device is a prescription device used to administer a blend of carbon dioxide and oxygen gases to a patient to induce hyperventilation. This device may be labeled for use with breathing circuits made of reservoir bags (21 CFR 868.5320), oxygen cannulas (21 CFR 868.5340), masks (21 CFR 868.5550), valves (21 CFR 868.5870), resuscitation bags (21 CFR 868.5915), and/or tubing (21 CFR 868.5925). NEW REGULATION NUMBER: 21 CFR 868.5480 CLASSIFICATION: Class II PRODUCT CODE: QFB BACKGROUND DEVICE NAME: ClearMateTM SUBMISSION NUMBER: DEN170044 DATE OF DE NOVO: August 23, 2017 CONTACT: Thornhill Research, Inc. 5369 W. Wallace Ave Scottsdale, AZ 85254 INDICATIONS FOR USE ClearMateTM is intended to be used by emergency department medical professionals as an adjunctive treatment for patients suffering from carbon monoxide poisoning. The use of ClearMateTM enables accelerated elimination of carbon monoxide from the body by allowing isocapnic hyperventilation through simulated partial rebreathing. LIMITATIONS Intended Patient Population is adults aged greater than 16 years old and a minimum of 40 kg (80.8 lbs) ClearMateTM is intended to be used by emergency department medical professionals. This device should always be used as adjunctive therapy; not intended to replace existing protocol for treating carbon monoxide poisoning. When providing treatment to a non-spontaneously breathing patient using the ClearMate™ non-spontaneous breathing patient circuit, CO2 monitoring equipment for the measurement of expiratory carbon dioxide concentration must be used. PLEASE REFER TO THE LABELING FOR A MORE COMPLETE LIST OF WARNINGS AND CAUTIONS. -

Relationship Between PCO 2 and Unfavorable Outcome in Infants With
nature publishing group Articles Clinical Investigation Relationship between PCO2 and unfavorable outcome in infants with moderate-to-severe hypoxic ischemic encephalopathy Krithika Lingappan1, Jeffrey R. Kaiser2, Chandra Srinivasan3, Alistair J. Gunn4; on behalf of the CoolCap Study Group BACKGROUND: Abnormal PCO2 is common in infants with term infants with HIE, both minimum and cumulative expo- hypoxic ischemic encephalopathy (HIE). The objective was to sure to hypocapnia in the first 12 h of the trial were associated determine whether hypocapnia was independently associated with death or adverse neurodevelopmental outcome (13). The with unfavorable outcome (death or severe neurodevelopmen- dose–response relationship between PCO2 and outcome for tal disability at 18 mo) in infants with moderate-to-severe HIE. infants with moderate-to-severe HIE is unknown. METHODS: This was a post hoc analysis of the CoolCap Study The risk of developing hypocapnia or hypercapnia may be in which infants were randomized to head cooling or standard affected by severity of brain injury, intensity and duration of care. Blood gases were measured at prespecified times after newborn resuscitation, timing after the primary injury, and/or randomization. PCO2 and follow-up data were available for 196 response to metabolic acidosis. Thus, in this secondary analy- of 234 infants. Analyses were performed to investigate the rela- sis of the CoolCap Study (14), we sought to confirm the obser- tionship between hypocapnia in the first 72 h after randomiza- vation that -

Clinical Management of Severe Acute Respiratory Infections When Novel Coronavirus Is Suspected: What to Do and What Not to Do
INTERIM GUIDANCE DOCUMENT Clinical management of severe acute respiratory infections when novel coronavirus is suspected: What to do and what not to do Introduction 2 Section 1. Early recognition and management 3 Section 2. Management of severe respiratory distress, hypoxemia and ARDS 6 Section 3. Management of septic shock 8 Section 4. Prevention of complications 9 References 10 Acknowledgements 12 Introduction The emergence of novel coronavirus in 2012 (see http://www.who.int/csr/disease/coronavirus_infections/en/index. html for the latest updates) has presented challenges for clinical management. Pneumonia has been the most common clinical presentation; five patients developed Acute Respira- tory Distress Syndrome (ARDS). Renal failure, pericarditis and disseminated intravascular coagulation (DIC) have also occurred. Our knowledge of the clinical features of coronavirus infection is limited and no virus-specific preven- tion or treatment (e.g. vaccine or antiviral drugs) is available. Thus, this interim guidance document aims to help clinicians with supportive management of patients who have acute respiratory failure and septic shock as a consequence of severe infection. Because other complications have been seen (renal failure, pericarditis, DIC, as above) clinicians should monitor for the development of these and other complications of severe infection and treat them according to local management guidelines. As all confirmed cases reported to date have occurred in adults, this document focuses on the care of adolescents and adults. Paediatric considerations will be added later. This document will be updated as more information becomes available and after the revised Surviving Sepsis Campaign Guidelines are published later this year (1). This document is for clinicians taking care of critically ill patients with severe acute respiratory infec- tion (SARI). -

Pressure-Controlled Ventilation in Children with Severe Status Asthmaticus*
Feature Articles Pressure-controlled ventilation in children with severe status asthmaticus* Ashok P. Sarnaik, MD, FAAP, FCCM; Kshama M. Daphtary, MD; Kathleen L. Meert, MD, FAAP; Mary W. Lieh-Lai, MD, FAAP; Sabrina M. Heidemann, MD, FAAP Objective: The optimum strategy for mechanical ventilation in trolled ventilation, median pH increased to 7.31 (6.98–7.45, p < a child with status asthmaticus is not established. Volume-con- .005), and PCO2 decreased to 41 torr (21–118 torr, p < .005). For trolled ventilation continues to be the traditional approach in such patients with respiratory acidosis (PCO2 >45 torr) within 1 hr of children. Pressure-controlled ventilation may be theoretically starting pressure-controlled ventilation, the median length of time more advantageous in allowing for more uniform ventilation. We until PCO2 decreased to <45 torr was 5 hrs (1–51 hrs). Oxygen describe our experience with pressure-controlled ventilation in saturation was maintained >95% in all patients. Two patients had children with severe respiratory failure from status asthmaticus. pneumomediastinum before pressure-controlled ventilation. One Design: Retrospective review. patient each developed pneumothorax and subcutaneous emphy- Setting: Pediatric intensive care unit in a university-affiliated sema after initiation of pressure-controlled ventilation. All pa- children’s hospital. tients survived without any neurologic morbidity. Median duration Patients: All patients who received mechanical ventilation for of mechanical ventilation was 29 hrs (4–107 hrs), intensive care status asthmaticus. stay was 56 hrs (17–183 hrs), and hospitalization was 5 days Interventions: Pressure-controlled ventilation was used as the (2–20 days). initial ventilatory strategy. The optimum pressure control, rate, Conclusions: Based on this retrospective study, we suggest and inspiratory and expiratory time were determined based on that pressure-controlled ventilation is an effective ventilatory blood gas values, flow waveform, and exhaled tidal volume. -
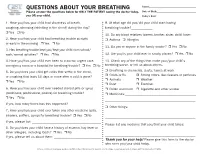
QUESTIONS ABOUT YOUR BREATHING Name:______Please Answer the Questions Below for ONLY the PATIENT Seeing the Doctor Today, Date of Birth:______You OR Your Child
QUESTIONS ABOUT YOUR BREATHING Name:_____________________________________ Please answer the questions below for ONLY THE PATIENT seeing the doctor today, Date of Birth:_______________________________ you OR your child. Today’s Date:_______________________________ 1. Have you/has your child had shortness of breath, 9. At what age did you/did your child start having coughing, wheezing (whistling in the chest) during the day? breathing trouble?_____________ r Yes r No 10. Do any blood relatives (parent, brother, sister, child) have: 2. Have you/has your child had breathing trouble at night r Asthma r Allergies or early in the morning r Yes r No 11. Do you or anyone in the family smoke? r Yes r No 3. Has breathing trouble kept you/kept your child from school/ work/normal activities? r Yes r No 12. Are you/is your child ever in smoky places? r Yes r No 4. Have you/has your child ever been to a doctor, urgent care, 13. Check any of the things that make your/your child’s emergency room or a hospital for breathing trouble? r Yes r No breathing worse, or tell us about others. 5. Do you/does your child get colds that settle in the chest, r Breathing in chemicals, dusts, fumes at work r Colds or flu r Strong odors, like cleaners or perfumes or coughing that lasts 10 days or more after a cold is gone? r Animals r Weather r Yes r No r Dust r Exercise 6. Have you/has your child ever needed steroid pills or syrup r Pollen and mold r Cigarette and other smoke (prednisone, prednisolone, prelone) for breathing trouble? r Medicines:___________________________________________ r Yes r No _______________________________________________________ If yes, how many times has this happened? ___________________ r Other things: 7. -

HANDOUT #1 CONCEPT INTRODUCTION PRESENTATION: PERFUSION Topic Description Definition of Perfusion the Passage of Oxygenated Capi
HANDOUT #1 CONCEPT INTRODUCTION PRESENTATION: PERFUSION Topic Description Definition of Perfusion The passage of oxygenated capillary blood through body tissues. Peripheral perfusion is passage (flow) of blood to the extremities of the body. Central perfusion is passage (flow) of blood to major body organs, including the heart and lungs. Scope of Perfusion Perfusion can be viewed on a continuum as adequate on one end and inadequate, decreased, or impaired on the other. Decreased Perfusion can range from minimal to severe. Ischemia refers to decreased Perfusion, while infarction is complete tissue death due to severe decreased Perfusion. Risk Factors/Populations at Risk for Examples of risk factors or populations at risk Impaired Perfusion for impaired Perfusion can be categorized as modifiable (can be changed) and nonmodifiable (cannot be changed) Modifiable factors include: • Obesity • Lack of physical activity/sedentary lifestyle • Smoking Nonmodifiable factors include age, gender, and race/ethnicity. Groups at risk for impaired Perfusion include those who are of advanced age (due to less elastic arterial vessels as a result of aging) and those who are African American and Hispanic. These racial/ethnic groups are most at risk for chronic diseases that can affect Perfusion such as diabetes mellitus, hypertension, hyperlipidemia, and peripheral vascular disease. The cause of these variations is not known, but dietary and environmental factors may contribute to the higher incidence of chronic disease in these groups. Newborns and infants who have congenital heart anomalies are also at risk for impaired central Perfusion. Many of these defects can be surgically repaired to regain adequate Perfusion. Physiologic Consequences of Impaired Consequences of impaired Perfusion vary Perfusion depending on the degree of impairment. -

What Are the Health Effects from Exposure to Carbon Monoxide?
CO Lesson 2 CARBON MONOXIDE: LESSON TWO What are the Health Effects from Exposure to Carbon Monoxide? LESSON SUMMARY Carbon monoxide (CO) is an odorless, tasteless, colorless and nonirritating Grade Level: 9 – 12 gas that is impossible to detect by an exposed person. CO is produced by the Subject(s) Addressed: incomplete combustion of carbon-based fuels, including gas, wood, oil and Science, Biology coal. Exposure to CO is the leading cause of fatal poisonings in the United Class Time: 1 Period States and many other countries. When inhaled, CO is readily absorbed from the lungs into the bloodstream, where it binds tightly to hemoglobin in the Inquiry Category: Guided place of oxygen. CORE UNDERSTANDING/OBJECTIVES By the end of this lesson, students will have a basic understanding of the physiological mechanisms underlying CO toxicity. For specific learning and standards addressed, please see pages 30 and 31. MATERIALS INCORPORATION OF TECHNOLOGY Computer and/or projector with video capabilities INDIAN EDUCATION FOR ALL Fires utilizing carbon-based fuels, such as wood, produce carbon monoxide as a dangerous byproduct when the combustion is incomplete. Fire was important for the survival of early Native American tribes. The traditional teepees were well designed with sophisticated airflow patterns, enabling fires to be contained within the shelter while minimizing carbon monoxide exposure. However, fire was used for purposes other than just heat and cooking. According to the historian Henry Lewis, Native Americans used fire to aid in hunting, crop management, insect collection, warfare and many other activities. Today, fire is used to heat rocks used in sweat lodges.