Hospital Isolated Power Systems
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
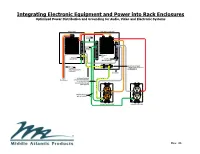
Power Distribution and Grounding of Audio, Video And
Integrating Electronic Equipment and Power into Rack Enclosures Optimized Power Distribution and Grounding for Audio, Video and Electronic Systems MAIN PANEL SUB PANEL (optional) Grounding Conductor Grounded Conductor (neutral) Ground Bar Neutral & Ground Bar Neutral (On insulators) Technical (isolated) Grounded Conductor “single-point” ground bar (Neutral & Ground on insulators combined) Enclosure From Technical (isolated) ground wire terminated Transformer in main panel only (no connection to sub panel ground) Building ground wire or conduit Isolated ground outlet conventional outlet Rev. 4b Table of Contents Preface ........................................................................................................................... 1 Neutral-Ground reversals .............................................................................................. 30 A Note about Signal Paths .............................................................................................. 2 Steps to Troubleshoot Bootleg Grounds and Neutral-Ground Reversals ....................... 32 Ground Loops and Signal Interconnections .................................................................... 2 Auxiliary Ground Rods ................................................................................................... 34 Signal Wiring: Unbalanced & Balanced Interfaces .......................................................... 3 Intersystem Bonding (Cable TV, Satellite TV, Telephone) ............................................. 35 AC Magnetic Fields -
Surge Protection, Power Distribution and Uninterruptible Power
SECTION R Surge Protection, Power Distribution and Uninterruptible Power Supply Devices INDEX Industrial Surge Protective Devices Overview . .R2 Four-Outlet Plug-Ins . .R3 5100 Series . .R3 Surge Strips . .R4 Surge Protection Modules . .R5 Surge Protection Panels . .R6, R7 74000 Series . .R6 Surge Protection Devices 57000 Series . .R7 52000 Series . .R8 47000 and 52000-7M3 Series . .R9 42000 and 32000 Series . .R10 Low Voltage Communications SPD’s 3400 and 3800 Series . .R11 Surge Counter: 51000 SMC . .R11 Equipment Cabinet SPD’s . .R12 3800 Series . .R12 Surge Protection Receptacles . .R13 Decora Series Four-In-One Series . .R14 Commercial Surge Protection Devices S1000 and S2000 Series Surge Strips . .R15 4950 Series Surge Strips . .R15 5500 and 5505 Series PDU’s with Surge Protection . .R16 Rack-mounted Power Distribution Devices 4505 Series 19" Rack Mount PDUs . .R17 P1000 Series PDUs . .R17 Metered Series PDUs . .R18 Switched Series PDUs . .R19 Residential Surge Protection Devices Meter Socket Surge Adapter . .R20 Secondary Surge Arrestors . .R20 General Purpose Plug-Ins . .R21 51000 Series Surge Protection Panels . .R21 3950 Series Module Bracket . .R22 5950 Series Surge Modules . .R22 Uninterruptible Power Supplies Sine and Online Series UPS Systems . .R23 Pro, Slim and Strip Series UPS Systems . .R23, R24 SURGE PROTECTION DEVICE FEATURES Industrial Grade Surge Protection Devices LEVITON’S SURGE PROTECTIVE DEVICES (SPD’S) ARE DESIGNED TO REDUCE THE RANDOM ENERGY SURGES OF VOLTAGE TRANSIENTS AND ELECTRICAL NOISE ON THE POWER SUPPLY LINE. Volatile transients and noise are present in utility power lines, data networks, telephone lines, closed circuit and cable tv feeds, and any other power or control lines connected to electronic equipment. -
Cord & Cordset Products
Cord & Cordset Products FOR INDUSTRIAL, COMMERCIAL AND SPECIALTY APPLICATIONS CORD & CORDSET& CORD PRODUCTS NOVEMBER 2017 Cord & Cordset This catalog contains in-depth What’s New? information on the most OUR BEST CORD JUST GOT BETTER comprehensive line of cord and The rubber cord that changed an industry just got better. General cordset products. General Cable’s Cable now offers Super Vu-Tron® Supreme with GenClean® flexible cord products are available technology as a standard feature, enabling users to benefit from this proprietary cleanable jacket technology. An outstanding today for commercial, industrial solution for the food and beverage industry, Super Vu-Tron Supreme with GenClean offers all the benefits and durability and specialty applications. Our of rubber cord with a cleanable jacket that permits unwanted contractor-grade extension cords, material to be more readily removed in a wash cycle. Learn more about GenClean on page 9. specialty cords, utility lights and accessories provide power for tools THE POWER IS ON — FROGHIDE® ULTRA FLEX® and equipment, and temporary LIGHTED EXTENSION CORD lighting on residential, commercial and industrial job sites. With the help of contractors, tradesmen and homeowners, we’ve created the ultimate extension cord. More flexible, more durable and more identifiable than any other cord on the market, featuring The product and technical sections a lighted connector to indicate the power is on — the one and only have been developed with an easy- FrogHide Ultra Flex lighted extension cord. Carol® Brand FrogHide Ultra Flex lighted extension cords are bonded to the caps and to-use “spec-on-a-page” format. connectors with heavy-duty strain reliefs built in for lasting They feature the latest information strength, even in rough applications. -

Plug Patterns… and Counting
INTER ISSUE 1 | SUMMER 2011 MAGAZINE FALL 2011 | ISSUE 1 Plug Patterns… and Counting PLUS: • Partially Insulated Swiss Plugs Increase Safety pg 6 • Saudi Arabian Standards Changed And Enforced pg 18 • A Closer look at the Brazilian Plug Standard pg 20 No minimum order requirements for Continental European cords Interpower Corporation manufactures Continental European power cords and cord sets. The Continental European plug carries all the appropriate approvals. Many lengths are in stock, and we offer a 1-week manufacturing lead time for nonstock cords. Customize your power cord or cord set! Choose from a variety of colors with no set-up charge. Interpower Corporation can also mold IEC 60320 C13 and C19 connectors. We offer straight and four angled IEC 60320 C13 connectors. All connectors fi t our existing connector locks. Connector locks secure the connector, preventing accidental removal or interruption. Custom lengths, labeling and packaging are also available upon request. Our Customer Service Department is ready to serve you from 7 a.m. to 7 p.m. Central Standard Time with no automated call attendant; receptionists answer every phone call. From 1 piece to 1,000 pieces or more we offer no minimum order requirements, so you only purchase what you need. With a 1-week manufacturing lead time, and no minimum order requirements, Interpower Corporation is your one-stop shop for power system components. • Continental European plug carries all appropriate approvals • 1-week manufacturing lead time on any nonstock Continental European power cord or cord set Toll-Free Phone: (800) 662-2290 • No minimum order requirements Order a free Catalog on CD today! E-mail [email protected] or call toll-free.