Assessing the Role of Copy Number Variations, Mitochondrial DNA and Micrornas in Neurodegenerative Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Truth and Reconciliation Commission of South Africa Report: Volume 2
VOLUME TWO Truth and Reconciliation Commission of South Africa Report The report of the Truth and Reconciliation Commission was presented to President Nelson Mandela on 29 October 1998. Archbishop Desmond Tutu Ms Hlengiwe Mkhize Chairperson Dr Alex Boraine Mr Dumisa Ntsebeza Vice-Chairperson Ms Mary Burton Dr Wendy Orr Revd Bongani Finca Adv Denzil Potgieter Ms Sisi Khampepe Dr Fazel Randera Mr Richard Lyster Ms Yasmin Sooka Mr Wynand Malan* Ms Glenda Wildschut Dr Khoza Mgojo * Subject to minority position. See volume 5. Chief Executive Officer: Dr Biki Minyuku I CONTENTS Chapter 1 Chapter 6 National Overview .......................................... 1 Special Investigation The Death of President Samora Machel ................................................ 488 Chapter 2 The State outside Special Investigation South Africa (1960-1990).......................... 42 Helderberg Crash ........................................... 497 Special Investigation Chemical and Biological Warfare........ 504 Chapter 3 The State inside South Africa (1960-1990).......................... 165 Special Investigation Appendix: State Security Forces: Directory Secret State Funding................................... 518 of Organisations and Structures........................ 313 Special Investigation Exhumations....................................................... 537 Chapter 4 The Liberation Movements from 1960 to 1990 ..................................................... 325 Special Investigation Appendix: Organisational structures and The Mandela United -
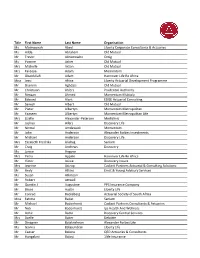
2020 Convention Attendee List 201007.Xlsx
Title First Name Last Name Organisation Ms Maimoonah Abed Liberty Corporate Consultants & Actuaries Ms Hilda Abraham Old Mutual Mr Trevor Abromowitz Omig Ms Yvonne Acker Old Mutual Mrs Michelle Acton Old Mutual Mrs Fareeya Adam Momentum Mr Obaidullah Adam Hannover Life Re Africa Miss Jessi Africa Liberty Actuarial Development Programme Mr Shamim Aghdasi Old Mutual Mr Christiaan Ahlers Prudential Authority Mr Rimaan Ahmed Momentum Multiply Mr Edward Alant EDGE Actuarial Consulting Mr Sanesh Albert Old Mutual Mr Pieter Albertyn Momentum Metropolitan Mr Yaaseen Albertyn Momentum Metropolitan Life Mrs Lizelle Alexander‐Petersen Mediclinic Mr Joshua Allers Discovery Life Mr Nirmal Amdawadi Momentum Mr John Anderson Alexander Forbes Investments Mr Michael Anderson Discovery Life Mrs Elizabeth Fredrika Andrag Sanlam Mr Craig Andrews Discovery Ms Janice Angove Mrs Petro Appelo Hannover Life Re Africa Mr Victor Asiwe Discovery Insure Mrs Jeanine Astrup Cadiant Partners Actuarial & Consulting Solutions Mr Andy Atkins Ernst & Young Advisory Services Ms Susan Atkinson Mr Robert Attwell Mr Quintin J Augustine PPS Insurance Company Mr Bruce Austin Liberty Life Mr Conrad Backeberg Actuarial Society of South Africa Miss Fatima Badat Sanlam Mr Michael Badenhorst Cadiant Partners Consultants & Actuaries Mr Nick Badenhorst Ips Health And Wellness Mr Adhir Badul Discovery Central Services Mrs Azelle Baker Deloitte Mr Dinagren Balakrishnan Alexander Forbes Life Ms Gavina Balasundran Liberty Life Mr Caesar Balona QED Actuaries & Consultants Mr Hungalani Baloyi -

YOU US WE ALL BAM Harvey Theater Nov 11—14 at 7:30Pm
#BAMNextWave #YouUsWeAll Brooklyn Academy of Music Alan H. Fishman, Chairman of the Board William I. Campbell, Vice Chairman of the Board Adam E. Max, Vice Chairman of the Board Katy Clark, President Joseph V. Melillo, Executive Producer YOU US WE ALL BAM Harvey Theater Nov 11—14 at 7:30pm Running time: one hour & 20 minutes, no intermission Music by Shara Worden Text, direction, and design by Andrew Ondrejcak B.O.X. (Baroque Orchestration X) Season Sponsor: Leadership support for opera at BAM provided by Aashish & Dinyar Devitre Endowment funding has been provided by The Andrew W. Mellon Foundation Fund for Opera and Music-Theater Major support for opera at BAM provided by The Francena T. Harrison Foundation Trust YOU US WE ALL CAST HOPE Shara Worden VIRTUE Helga Davis LOVE Martin Gerke DEATH Bernhard Landauer TIME Carlos Soto B.O.X. ENSEMBLE A Continuo/Rythm Section Theorbo, artistic direction Pieter Theuns Harpsichord, organ Anthony Romaniuk Baroque harp Jutta Troch Drums, percussion Mattijs Vanderleen An Alta Capella of Winds Cornett, flutes Lambert Colson Cornett, trumpet Jon Birdsong Sackbut (baroque trombone) Liza Malamut A Consort of Viols Treble viol, bass viol Liam Byrne Bass viol Pieter Vandeveire Violone Christine Sticher PRODUCTION CREDITS Stage, light, costume, projection design Andrew Ondrejcak Choreographer Seth Stewart Williams Production dramaturg Anne Seiwerath Executive producer/tour management ArKtype/Thomas O. Kriegsmann Production manager/lighting director Davison Scandrett Production stage manager Valerie Oliveiro Assistant stage manager Nina Segal Video design consultant Andrew Bauer Video supervisor Tei Blow Co-lighting design Lutz Deppe Co-costume design Zane Philstrom Assistant director Cecile Tonizzo Sound design David Schnirman/Hear No Evil Wig design Rick Gradone Make-up design Marco Campos Assistant, costumes and wardrobe Baille Younkman Assistant, costumes Julie Michaels Production assistant Veerle Van Rossom YOU US WE ALL is commissioned by B.O.X. -

Participant List
Participant List 10/20/2019 8:45:44 AM Category First Name Last Name Position Organization Nationality CSO Jillian Abballe UN Advocacy Officer and Anglican Communion United States Head of Office Ramil Abbasov Chariman of the Managing Spektr Socio-Economic Azerbaijan Board Researches and Development Public Union Babak Abbaszadeh President and Chief Toronto Centre for Global Canada Executive Officer Leadership in Financial Supervision Amr Abdallah Director, Gulf Programs Educaiton for Employment - United States EFE HAGAR ABDELRAHM African affairs & SDGs Unit Maat for Peace, Development Egypt AN Manager and Human Rights Abukar Abdi CEO Juba Foundation Kenya Nabil Abdo MENA Senior Policy Oxfam International Lebanon Advisor Mala Abdulaziz Executive director Swift Relief Foundation Nigeria Maryati Abdullah Director/National Publish What You Pay Indonesia Coordinator Indonesia Yussuf Abdullahi Regional Team Lead Pact Kenya Abdulahi Abdulraheem Executive Director Initiative for Sound Education Nigeria Relationship & Health Muttaqa Abdulra'uf Research Fellow International Trade Union Nigeria Confederation (ITUC) Kehinde Abdulsalam Interfaith Minister Strength in Diversity Nigeria Development Centre, Nigeria Kassim Abdulsalam Zonal Coordinator/Field Strength in Diversity Nigeria Executive Development Centre, Nigeria and Farmers Advocacy and Support Initiative in Nig Shahlo Abdunabizoda Director Jahon Tajikistan Shontaye Abegaz Executive Director International Insitute for Human United States Security Subhashini Abeysinghe Research Director Verite -

Geting Tau Pathology Or Other Patients with CBS Have Been Studied
VI Sindem MEETING Italian Association for the Study of Dementia linked to the Italian Neurological Society (SIN) Milan, Centro Congressi della Provincia di Milano – Via Corridoni, 16 March 17–19, 2011 PROCEEDINGS Scientifi c Committee Vincenzo Bonavita Carlo Caltagirone Claudio Mariani Alessandro Padovani Elio Scarpini Sandro Sorbi SINdem INVITED SPEAKERS The Progressive Aphasias S5 Stefano F. Cappa Corticobasal Degeneration and Corticobasal Syndrome: Lumping Versus Splitting Barbara Borroni S7 Amyotrophic Lateral Sclerosis and Dementia: The Borders Lucio Tremolizzo, Emanuela Susani, Matteo De Rosa, Michela Strozzi, Laura Marzorati, Ildebrando Appollonio and Carlo Ferrarese S10 Diagnostic Flow Chart for the Atypical Variants of Dementia Paolo Caffarra, Simona Gardini and Letizia Concari S13 Predictors of Successful Ageing: Epidemiological Evidence Laura Fratiglioni S16 Lifestyle and Rate of Progression of Cognitive Decline: Results of the SINDEM Cohort Study Massimo Musicco S17 Vascular Risk Factors and Leukoaraiosis: Results from the LADIS Study Domenico Inzitari S19 Dual Tasking and Memory Binding in Alzheimer’s Disease Sergio Della Sala, Jennifer A. Foley, Mario A. Parra and Robert H. Logie S22 Cognitive Neuroscience of Decision Making: Clinical and Implications Stefano F. Cappa S25 The Role of Emotions in Decisional Processes: How Neuroscience can Impact Evaluation of Patients’ Ability to will and to Act Paolo Nichelli, Mariangela Molinari and Francesca Benuzzi S27 Assessment of Capacity Andrea Stracciari S28 Using Biology to Untie -

Parkinson Disease from Mendelian Forms to Genetic Susceptibility: New Molecular Insights Into the Neurodegeneration Process
Cellular and Molecular Neurobiology https://doi.org/10.1007/s10571-018-0587-4 REVIEW PAPER Parkinson Disease from Mendelian Forms to Genetic Susceptibility: New Molecular Insights into the Neurodegeneration Process Amin Karimi‑Moghadam1 · Saeid Charsouei2 · Benjamin Bell3 · Mohammad Reza Jabalameli1,3 Received: 12 February 2018 / Accepted: 20 April 2018 © The Author(s) 2018 Abstract Parkinson disease (PD) is known as a common progressive neurodegenerative disease which is clinically diagnosed by the manifestation of numerous motor and nonmotor symptoms. PD is a genetically heterogeneous disorder with both familial and sporadic forms. To date, researches in the field of Parkinsonism have identified 23 genes or loci linked to rare monogenic familial forms of PD with Mendelian inheritance. Biochemical studies revealed that the products of these genes usually play key roles in the proper protein and mitochondrial quality control processes, as well as synaptic transmission and vesicular recycling pathways within neurons. Despite this, large number of patients affected with PD typically tends to show sporadic forms of disease with lack of a clear family history. Recent genome-wide association studies (GWAS) meta-analyses on the large sporadic PD case–control samples from European populations have identified over 12 genetic risk factors. However, the genetic etiology that underlies pathogenesis of PD is also discussed, since it remains unidentified in 40% of all PD-affected cases. Nowadays, with the emergence of new genetic techniques, international PD genomics consortiums and public online resources such as PDGene, there are many hopes that future large-scale genetics projects provide further insights into the genetic etiology of PD and improve diagnostic accuracy and therapeutic clinical trial designs. -

Google Has Had More Murdered and Strangely Dead Employees Than Almost Any Other U.S
Google Has Had More Murdered And Strangely Dead Employees Than Almost Any Other U.S. Company Google Has Had More Murdered And Strangely Dead Employees Than Almost Any Other U.S. Company CIA-Front Google seems to get it's people killed quit a bit, and it is not just a math odds issue. Google employee found dead in San Francisco Bay A woman whose body was found in the water along the San Francisco Bay Trail in Sunnyvale, California was identified as a Google employee by the company Monday. Chuchu Ma, 23, was found dead half ⦠https://www.rawstory.com/2017/12/google-employee-found-dead-in-san... 23-year-old Google employee found dead in San Francisco Bay 4 Ex-NFL Network employee alleges sexual misconduct by former players in lawsuit. 5 Cecil Parkinson's daughter is found dead at 57. 7 San Francisco mayor dies suddenly at 65. 8 GoogleStoryboard turns your videos into comic strips. gizmorati.com/2017/12/13/23-year-old-google-employee-fo NYC Google employee killed jogging in Massachusetts - NY ... A Google employee from New York City was killed while jogging in Massachusetts over the weekend â a murder eerily reminiscent of the slaying of Karina ... nydailynews.com/news/national/homicide-probe-opened-nyc-g... Vanessa Marcotte: Google Employee Killed and Sexually ... A 27-year-old Google employee who was found dead in the woods on Sunday had been stripped naked and partially burned,⦠people.com/crime/vanessa-marcotte-google-employee-ki... Google Employee, 27, Found Dead Near Mother's Home in .. -

Obituary Index-K Surnames
Name Year Month Day Age Page Newspaper Date Source Note KAAG, ANNA M 1991 3 8 70 104 SCRAPBOOK KAAN, MILDRED L 1988 12 28 87 380 SCRAPBOOK KABAKJIAN, ARMEN E DR 1969 2 6 66 19 SCRAPBOOK KABAKJIAN, EDNA W 1992 2 17 86 78 SCRAPBOOK KABAKJIAN, MARION ELIZABETH DR 1980 12 2 48 258 SCRAPBOOK KABATT, MILLICENT L (KENT) 2015 4 27 89 04/29/2015 LANC NEWSPAPERS KABOOL, KATHLEEN MARIE (SCHWEICH) 2016 11 23 57 01/15/2017 LANC NEWSPAPERS KABRHEL, JOSEPH F, JR 2012 7 9 67 07/12/2012 LANC NEWSPAPERS KACANDES, CHRYSOULA 1983 10 25 75 231 SCRAPBOOK KACH, JOHN J 2007 9 1 93 0 09/05/2007 LANC NEWSPAPERS KACHEL, ANNA MARY 2012 2 1 91 02/05/2012 LANC NEWSPAPERS KACHEL, ANNA MARY 2012 2 1 91 02/06/2012 LANC NEWSPAPERS KACHEL, CARRIE E 1973 2 13 90 29 SCRAPBOOK KACHEL, CARRIE E 1973 90 623 02/22/1973 CB OBITS KACHEL, CATHERINE 1978 8 12 62 142 SCRAPBOOK KACHEL, CHARLES E REV 1980 6 13 79 126 SCRAPBOOK KACHEL, CHARLES G 1969 1 13 75 15 IDL DIARY 1 KACHEL, CHARLES H 1988 2 13 67 47 SCRAPBOOK KACHEL, DAISY MAE 1969 4 1 81 98 IDL DIARY 2 KACHEL, DAISY MAE 1969 81 623 04/03/1969 CB OBITS KACHEL, DANIEL H SR 1985 1 19 66 19 SCRAPBOOK KACHEL, DANIEL H, JR 2012 5 12 69 05/19/2012 LANC NEWSPAPERS No Obit Published KACHEL, DANIEL S 1997 7 8 89 347 SCRAPBOOK KACHEL, DONNA I 2019 11 24 80 11/27/2019 LANC NEWSPAPERS KACHEL, DORA A 2006 5 12 83 0 05/13/2006 LANC NEWSPAPERS KACHEL, EARL MILLER 1993 6 2 80 278 SCRAPBOOK KACHEL, EDNA M 2004 8 28 89 371 SCRAPBOOK KACHEL, ELLEN M 1976 7 20 75 136 SCRAPBOOK KACHEL, EMMA L 1973 8 15 72 145 SCRAPBOOK KACHEL, ESTHER M 1986 4 8 77 -

ASSA 2012 Delegate List 091012
First Name Family Name Company Ioana Abrahams Financial Services Board Trevor Abromowitz OMIGSA Daniel Acres Prescient Investment Management Muhammad Aarif Adam Sanlam Abdurahman Adam Alexander Forbes Abubakar Addae Old Mutual Richard Addae-Manu C.S. -

Dr Anthony (Tony) Turton Light Horse Regiment & National Intelligence Service Missing Voices Project Interviewed by Mike Cadman 26 & 28/04/08
1 Dr Anthony (Tony) Turton Light Horse Regiment & National Intelligence Service Missing Voices Project Interviewed by Mike Cadman 26 & 28/04/08 TAPE ONE SIDE A Interviewer Tony, I’ve been through your book so I’ve got a good idea of your background, but can you give me just a brief, brief background of where you grew up, what your family was like, was it English speaking or Afrikaans speaking, how big and so on? Tony I don’t know if I can give you that briefly but I’ll be as brief as I possibly can. Firstly I welcome this project very much, I think it’s a hugely important project and when I first heard about it I got quite thrilled because this book that you’re talking about, I’m actually intending, if I can get all my ducks in a row, to in fact record it a sort of tape made for the blind kind of thing, sort of CD, so I’m actually looking for that. I had a very unusual upbringing in many ways, and even now at the age of 52, 53 I still ponder back on my life and think about this upbringing. Part of the unusualness of my upbringing, is the fact that I had a profound father who was a very, very interesting man. He learned Zulu as a first language, he never went to formal school as a small child and his father was, I now subsequently know, the product of the diamond rush, in fact the product of the Anglo Boer War. -

1 Mile Results
Race Name: The Midmar Mile Race Date: February 11-12 2017 Location: Durban, South Africa Distance: 1 Mile Rank Name Country Gender Div Age Group Time Points Entrants 1 Matthew Meyer South Africa M N 19&U 0:18:13 100.00 10912 2 Chad Ho South Africa M N 20-29 0:18:18 99.99 3 Chip Peterson USA M N 20-29 0:18:20 99.99 4 Ferry Weertman Netherlands M N 20-29 0:18:26 99.98 5 Tyrone Kruger South Africa M N 20-29 0:18:55 99.97 7 Neil Fair South Africa M N 20-29 0:18:59 99.97 8 Luke Erwee South Africa M N 20-29 0:19:19 99.96 9 Ashley Twichell USA F N 20-29 0:19:24 99.95 10 Holly Hibbott United Kingdom F N 20-29 0:19:37 99.95 11 Myles Brown South Africa M N 20-29 0:19:37 99.95 13 Martin Binedell South Africa M N 20-29 0:19:48 99.94 14 Chad Michau South Africa M N 20-29 0:19:51 99.93 15 Brendon Levy South Africa M N 20-29 0:19:55 99.93 16 Azyan Makhija South Africa M N 20-29 0:20:00 99.92 17 Dante Nortje South Africa M N 20-29 0:20:02 99.92 18 Calvin Stott South Africa M N 20-29 0:20:13 99.91 19 Luca Holtzhausen South Africa M N 19&U 0:20:16 99.90 20 Connor Grobler South Africa M N 20-29 0:20:21 99.89 22 Hanre Van Geffen South Africa M N 20-29 0:20:23 99.89 23 Evan Fair South Africa M N 20-29 0:20:23 99.89 24 Eric Le Roux South Africa M N 20-29 0:20:26 99.88 26 Ruben Du Pisanie South Africa M N 20-29 0:20:30 99.87 27 Gary Albertyn South Africa M N 40-49 0:20:30 99.86 28 Harrison Coulter South Africa M N 20-29 0:20:33 99.86 30 Robyn Kinghorn South Africa F N 20-29 0:20:34 99.85 38 Terry Heller South Africa M N 40-49 0:20:35 99.84 39 Cameron Pennell -

C9orf72 Intermediate Repeats Confer Genetic Risk for Severe COVID-19 Pneumonia Independently of Age
International Journal of Molecular Sciences Article C9orf72 Intermediate Repeats Confer Genetic Risk for Severe COVID-19 Pneumonia Independently of Age Isabella Zanella 1,2,*,†,‡ , Eliana Zacchi 3,4,‡, Simone Piva 5,6,‡, Massimiliano Filosto 3,7,‡ , Giada Beligni 8,9,†, Diana Alaverdian 8,9,†, Sara Amitrano 10,†, Francesca Fava 8,9,10,† , Margherita Baldassarri 8,9,† , Elisa Frullanti 8,9,†, Ilaria Meloni 8,9,†, Alessandra Renieri 8,9,10,† , GEN-COVID Multicenter Study †, GEVACOBA Study Group ‡, Francesco Castelli 3,4,†,‡ and Eugenia Quiros-Roldan 3,4,†,‡ 1 Department of Molecular and Translational Medicine, University of Brescia, 25123 Brescia, Italy 2 Clinical Chemistry Laboratory, Cytogenetics and Molecular Genetics Section, Diagnostic Department, ASST Spedali Civili di Brescia, 25123 Brescia, Italy 3 Department of Clinical and Experimental Sciences, University of Brescia, 25123 Brescia, Italy; [email protected] (E.Z.); massimiliano.fi[email protected] (M.F.); [email protected] (F.C.); [email protected] (E.Q.-R.) 4 Division of Infectious and Tropical Diseases, ASST Spedali Civili di Brescia, 25123 Brescia, Italy 5 University Division of Anesthesiology and Critical Care Medicine, ASST Spedali Civili, 25123 Brescia, Italy; [email protected] 6 Department of Medical and Surgical Specialties, Radiological Sciences and Public Health, University of Brescia, 25123 Brescia, Italy 7 NeMo-Brescia Clinical Center for Neuromuscular Diseases, 25064 Gussago, Italy 8 Medical Genetics, Department of Medical Biotechnologies,