Rotator Cuff Repair W/ SLAP
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bony Bankart Lesions and Shoulder Dislocations
Shoulder Dislocations and Bony Bankart Lesions The shoulder is the most mobile and the most commonly dislocated large joint in the body. Dislocation means that the joint is moved out of position, such that the joint surfaces at the ends of the bones are no longer in contact. In the shoulder, most dislocations are anterior (moving forward from the body); however, they can occur in several directions. When a dislocation occurs, the soft tissues that stabilize the shoulder can be torn, and the bone that forms the socket also can be broken at the same time. Traumatic dislocations of the shoulder can result in a Bankart lesion (tear). The head of the humerus (ball of upper arm bone) is stabilized against the glenoid (socket of the shoulder joint) using a combination of muscles, labrum, and ligaments. Ligaments run from the glenoid to the humeral head, and they blend with fibrous tissue called the capsule that encloses the entire joint. When the humeral head is forced forward in a dislocation, the soft tissues stretch or tear, and in some cases, bone is fractured off the glenoid rim, resulting in a bony Bankart lesion. X-ray of a patient with a bony Bankart facture of 3-D scan of the same patient more clearly the glenoid (socket), secondary to shoulder recreating the fracture. dislocation. Orthopaedic Surgery & Sports Medicine 630-324-0402 ⚫ [email protected] Teaching & Research Foundation stevenchudikmd.com otrfund.org Schedule online now © 2018 Steven Chudik MD Shoulder, Knee & Sports Medicine. All rights reserved. Frequent Signs and -

34Th Annual Meeting of the Japan Shoulder Society
34TH ANNUAL MEETING OF THE JAPAN SHOULDER SOCIETY 1 F Wave Monitoring After Arthroscopic Shoulder Surgery gers may be used to evaluate the functions of the shoulder joint. It is IWATA Yoshio, Department of Orthopaedics, Uji Takeda Hospital also believed that people can perform approximately half of the ac- MORIHARA Toru, HAYASHIDA Tatsurou, OGURA Akiko, KUBO tions even if the diseased hand is on their dominant side. Toshikazu, Department of Orthopaedics, Kyoto Prefectural Univer- sity of Medicine, Graduate School of Medical Science HORII Motoyuki, Department of Orthopaedic Surgery, Kyoto Inter- 3 The Shoulder Function of Congenital Clavicle Anomalies disciplinary Institute Hospital of Community Medicine KENMOKU Tomonori, Department of Orthopaedics Surgery, Chiba KUROKAWA Masao, Department of Orthopaedic Surgery, Saisei- Univercity Graduate School of Medicine kai Suita Hospital SAISU Takashi, KAMEGAYA Makoto, Division of Orthopaedics Sur- The purpose of this study was to evaluate the modulation of excit- gery, Chiba Children’s Hospital ability of spinal motor neuron function. We investigated F waves af- MIKASA Motohiko, Matsudo Orthopaedic Hospital ter arthroscopic shoulder surgery. We evaluated 7 subjects who There was no report on the shoulder function of congenital clav- underwent an arthroscopic shoulder surgery. There were 5 men icle anomalies. Our purpose was to clarify the role of the clavicle, and 2 women; the mean age at the time of surgery was 33.6 years investigating the shoulder function in patients with clavicle defect old. In our study, F waves were recorded from the abductor pollicis or pseudoarthrosis. muscle after transcutaneous median nerve stimulation at bilateral Thirteen shoulders of 9 patients with congenital clavicle anoma- wrists. -
Presentations
7/4/2019 30th Brucosport Football Medicine: What’s New 2017 Bruges, Belgium 11 March 2017 Aspetar Orthopaedic and Sports Medicine Hospital 1 Dr. Scott Gillogly Chief Medical Officer 26 February 2017 2 1 7/4/2019 Articular Cartilage Injuries in the Knee: Evaluation and Surgical Treatment Options based on Return to Play Scott D. Gillogly, MD 34th FIMS World Sports Medicine Congress Ljubljana, Slovenia 29 September - 2 October 2016 Aspetar Orthopaedic and Sports Medicine Hospital 3 ICRS Annual Meeting 29 September 2016 Aspetar Orthopaedics and Sorrento, Italy Sports Medicine Hospital 4 2 7/4/2019 Articular Cartilage Injuries in the Knee: Evaluation and Surgical Treatment Options based on Return to Play Scott D. Gillogly, MD AFC Team Physiotherapist Sports Medicine Course Doha, Qatar 13-15 June 2016 Aspetar Orthopaedic and Sports Medicine Hospital 5 Cartilage Defects in Athletes: Return To Play (RTP) Scott D. Gillogly, MD 1st GCC Sports Medicine Conference Doha, Qatar 23 April 2016 Aspetar Orthopaedic and Sports Medicine Hospital 6 3 7/4/2019 AAOS Articular Cartilage Restoration: The Modern Frontier 1 April 2016 Aspetar Orthopaedics and Sports Medicine Hospital Chicago, Illinois 7 AAOS Articular Cartilage Restoration: The Modern Frontier 2 April 2016 Aspetar Orthopaedics and Chicago, Illinois Sports Medicine Hospital 8 4 7/4/2019 8 April 2016 Aspetar Orthopaedics and Washington, D.C. Sports Medicine Hospital 9 8 April 2016 Aspetar Orthopaedics and Washington, D.C. Sports Medicine Hospital 10 5 7/4/2019 Return to Play (RTP) After Cartilage Repair of the Knee Scott D. Gillogly, MD Challenges in Football Injuries Doha, Qatar 11‐12 February, 2016 Aspetar Orthopaedic and Sports Medicine Hospital 11 Partial Osteochondral Fractures of the Condyles (Osteochondral Defects) Scott D. -

Rotator Cuff and Subacromial Impingement Syndrome: Anatomy, Etiology, Screening, and Treatment
Rotator Cuff and Subacromial Impingement Syndrome: Anatomy, Etiology, Screening, and Treatment The glenohumeral joint is the most mobile joint in the human body, but this same characteristic also makes it the least stable joint.1-3 The rotator cuff is a group of muscles that are important in supporting the glenohumeral joint, essential in almost every type of shoulder movement.4 These muscles maintain dynamic joint stability which not only avoids mechanical obstruction but also increases the functional range of motion at the joint.1,2 However, dysfunction of these stabilizers often leads to a complex pattern of degeneration, rotator cuff tear arthropathy that often involves subacromial impingement.2,22 Rotator cuff tear arthropathy is strikingly prevalent and is the most common cause of shoulder pain and dysfunction.3,4 It appears to be age-dependent, affecting 9.7% of patients aged 20 years and younger and increasing to 62% of patients of 80 years and older ( P < .001); odds ratio, 15; 95% CI, 9.6-24; P < .001.4 Etiology for rotator cuff pathology varies but rotator cuff tears and tendinopathy are most common in athletes and the elderly.12 It can be the result of a traumatic event or activity-based deterioration such as from excessive use of arms overhead, but some argue that deterioration of these stabilizers is part of the natural aging process given the trend of increased deterioration even in individuals who do not regularly perform overhead activities.2,4 The factors affecting the rotator cuff and subsequent treatment are wide-ranging. The major objectives of this exposition are to describe rotator cuff anatomy, biomechanics, and subacromial impingement; expound upon diagnosis and assessment; and discuss surgical and conservative interventions. -

SLAP Repairs Versus Biceps Tenodesis in Athletes 15 Min Power Points
SLAP Repairs Versus Biceps Tenodesis in Athletes 15 min Power Points • Not all SLAP tears need surgery • Preservation of Native Anatomy GOAL • Not all labral repairs are equal • Kinetic chain MUST be addressed Power Points • Biceps DOES have a function • Tenodesis has consequences • Tenodesis relieves pain reliably BUT……long term effects uncertain ‘SLAPAHOLIC’ T. Romeo • One who fixes EVERY SLAP TEAR and anything that remotely looks like one! Not all SLAP Tears Need Surgery • SLAP tears way overdiagnosed • Beware of positive imaging study - negative exam • Slight labral separation may allow thrower to ‘get the slot’ MRI May OVERDIAGNOSE • Specificity ranges from 63% to 91% MRI and Anatomic Variants • Meniscoid labrum • Buford complex • Cord like MGHL • Age related attritional tear • ALL CAN LOOK LIKE SLAP TEARS ON MRI!! Meniscoid Labrum ‘Buford’ Complex Labral Tears are Part of the Aging Process! Pfahler et al JSES 2003 MANY LABRAL TEARS RESPOND TO REHAB!!!! Nonoperative Treatment of Superior Labrum Anterior Posterior Tears Improvements in Pain, Function, and Quality of Life Edwards et al • Approx. 50% of non operatively treated patients avoided surgery! Scapular strengthening, posterior capsular stretching Overtreat >>>> NIGHTMARE Make Sure History Consistent with SLAP “event” • Sudden loss of velocity (dead arm) • Large increase in pain • “mechanical symptoms” usually present • Rehab no longer effective Exam Hold Key!!! • Load Shift • Passive Distraction test • Mayo Shear • O’Brien’ Test (anterior) • Kim test • Relocation Test Mayo Shear -
THE MANAGEMENT of SLAP INJURIES in the OVERHEAD ATHLETE Michael G
THE MANAGEMENT of SLAP INJURIES in the OVERHEAD ATHLETE Michael G. Ciccotti, MD The Everett J. and Marian Gordon Professor of Orthopaedics Chief, Division of Sports Medicine Rothman Institute Thomas Jefferson University Head Team Physician, Philadelphia Phillies Faculty Disclosure Consultant – Stryker Endoscopy Consultant – Venture MD Research Support – Arthrex Board/Committee Membership – Orthopaedic Learning Center BOD MLB Medical Advisory Committee MLB Elbow Research Study Group AOSSM Fellowship Committee Rothman Institute of Orthopaedics at Thomas Jefferson University Shoulder Injury in the Athlete History Exam 27 y.o. RHD MLB 30 deg. less ABD, FF pitcher 25 deg. less INT ROT Chronic, progressive + Hawkin’s Test right shoulder pain + O’Brien’s & DLS while throwing Tests Worsened acutely + mild-mod supraspinatus Pain is deep and post weakness Unable to throw Rothman Institute of Orthopaedics at Thomas Jefferson University ShoulderDiagnosis: Injury SLAP in the Athlete Tear Rothman Institute of Orthopaedics at Thomas Jefferson University Superior Labrum is Important for the Overhead Athlete! Biceps attachment site Deepens glenoid Distributes contact pressure between humerus & glenoid Harryman, 1992 – Washer Effect Pagnani, 1995 Lee, 2005 Attachment site for glenohumeral Veeger, 2007 ligaments & capsule Lee, 2008 Kibler, 2011 Pressure sensor for proprioception Rothman Institute of Orthopaedics at Thomas Jefferson University Predictable Series of Events in Throwers Progressive Osseous changes Scapular and Cuff -
An Overview of Common Injuries and Imaging Findings
SPORTS RADIOLOGY SHOULDER DISLOCATION AMONG ATHLETES AN OVERVIEW OF COMMON INJURIES AND IMAGING FINDINGS – Written by Nima Hafezi–Nejad, Shadpour Demehri and John A Carrino, USA The Glenohumeral (GH) joint has a mobility is often termed hyperlaxity, a during sports activities. Second, SD may arise large range of motion that leaves it prone common feature among many athletes. as a result of chronic injuries, mostly in the to shoulder instability, ranging from Hyperlaxity may help athletes by enhancing form of recurrent microtrauma and overuse. subluxation to frank shoulder dislocation their range of motion. However, this may Secondary forms of impingement and (SD). Due to the shallow depth of the glenoid’s become a problem when it is accompanied injury to the dynamic soft tissue stabilisers osseous structure, shoulder stability is by a functional deficit and pathological may arise from recurrent microtrauma as achieved through a number of additional symptoms. Typical symptoms include well2. soft tissue stabilisers (including the glenoid pain and a subjective feeling of instability labrum). Rotator cuff muscles are the most or apprehension. While instability and ADVANCED IMAGING FINDINGS – AN important dynamic stabilisers of the GH hyperlaxity are two distinct phenomena, OVERVIEW joint. Other muscles that cross the GH joint, they frequently occur together in athletes Radiography remains the primary such as pectoralis major and latissimus dorsi, suffering from SD1. modality of choice when SD is suspected may potentially act as stabilisers as well. SD While purely atraumatic causes may (Figure 1). However, advanced imaging may arise from abnormal function of either account for a number of SDs among athletes, modalities including computed tomo- osseous (glenoid fossa and coracoacromial there are two main etiologies, behind athlete graphy (CT) and magnetic resonance arch) or soft tissue (glenoid labrum, articular SD. -

Rehab for Bicep Tendon Problems
Rehabilitation for Biceps Tendon Disorders and SLAP Lesions 117 capsulitis will suffer long-term ROM defi cits that may arthroscopic release (5); or MUA and arthroscopic last more than 10 years. Clarke et al. (1975) reported hydrodistension (20). During the long-term follow-up that 42% of patients continued to have motion loss (mean 52.3 months) 59% of patients reported hav- after 6 years of follow-up. Likewise, Schaffer et al. ing normal or near-normal shoulders, 35% reported (1992) reported that 50% of patients managed non- persistent mild/moderate symptoms, and 6% still had operatively remained symptomatic during their long- severe symptoms. Persistent symptoms were reported term follow-up, which occurred 2–11 years after their as mild in 94% of patients, with pain being the most initial visit (mean = 7 years). Of these patients, 60% common complaint. Only 6% of patients complained had a measurable restriction of shoulder motion. of severe pain and/or functional loss. Patients with External rotation was the most chronically restricted the most severe symptoms at condition onset had the movement, providing further evidence that the rotator worst long-term prognosis. In general, patients with interval and coracohumeral ligament are particularly comorbid factors, particularly diabetes, hyperthyroid- affected by adhesive capsulitis. Hand et al. (2008) ism, hypothyroidism, hypoadrenalism, Parkinson's tracked outcomes in 269 shoulders affected by pri- disease, cardiac disease, pulmonary disease, or cere- mary adhesive capsulitis who received no treatment brovascular accident, tend to have more severe and (95); physical therapy (55); steroid injection (139); longer lasting symptoms and tend to be more recalci- manipulation under anesthesia (MUA) (5); MUA and trant to treatment. -

ESR-Endorsed ESSR DIPLOMA CORRECT ANSWERS (In Bold)
ESR-endorsed ESSR DIPLOMA Examination Session at ESSR 2015 York, June 19, 2015 CORRECT ANSWERS (in bold) 1. In the Erdheim-Chester disease, which of the following statements is true: a) it is a frequent disease in Western Europe b) is a Langerhans cell histiocytosis c) bone involvement is almost universal d) it essentially affects the axial skeleton and only rarely the long bones 2. In the POEMS syndrome, which of the following statements is false: a) affected patients are older than patients with standard multiple myeloma b) sclerotic bone lesions are found in the majority of the patients c) sclerotic bone lesions can be mistaken for bone islands d) as a consequence of treatment response, sclerotic bone lesions may to decrease in size 3) Taking into account ankle sprains, the highest incidence of injury can be found in the: a) calcaneofibular ligament b) posterior talofibular ligament c) anterior talofibular ligament d) tibiocalcaneal ligament 4) HIV-positive patients have a higher incidence of: a) bacillary angiomatosis b) thoracic cage tuberculosis c) reiter’s syndrome d) all of the previous entities 5) On MRI, the structures of the rotator cuff interval can be best evaluated on: a) oblique sagittal and oblique coronal images b) axial and oblique coronal images. c) oblique sagittal and axial images d) ABER position. 6) Which structure does not belong to the rotator cuff interval? a) coraco-acromial ligament b) long head of the biceps tendon c) coracohumeral ligament d) superior glenohumeral ligament 7) Most people under the age of -
SLAP Lesions? the Shoulder’S Large, Though Useful, Range of Motion Can Also Lead to Injuries
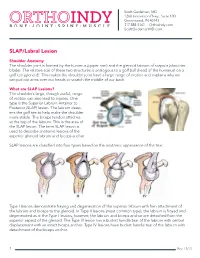
Scott Gudeman, MD 1260 Innovation Pkwy., Suite 100 Greenwood, IN 46143 317.884.5161 OrthoIndy.com ScottGudemanMD.com SLAP/Labral Lesion Shoulder Anatomy The shoulder joint is formed by the humerus (upper arm) and the glenoid labrum of scapula (shoulder blade). The relative size of these two structures is analogous to a golf ball (head of the humerus) on a golf tee (glenoid). This makes the shoulder joint have a large range of motion and explains why we can put our arms over our heads or scratch the middle of our back. What are SLAP Lesions? The shoulder’s large, though useful, range of motion can also lead to injuries. One type is the Superior Labrum Anterior to Posterior (SLAP) lesion. The labrum deep- ens the golf tee to help make the shoulder more stable. The biceps tendon attaches at the top of the labrum. This is the area of the SLAP lesion. The term SLAP lesion is used to describe anatomic lesions of the superior glenoid labrum and biceps anchor. SLAP lesions are classified into four types based on the anatomic appearance of the tear. Type I lesions demonstrate fraying and degeneration of the superior labrum with firm attachment of the labrum and biceps to the glenoid. In Type II lesions (most common type), the labrum is frayed and degenerated as in the Type I lesions; however, the labrum and biceps anchor are detached from the superior aspect of the glenoid. The Type III lesion has a bucket handle tear of the labrum with central displacement with an intact biceps anchor. -

Musculoskeletal Diagnostic Imaging
Musculoskeletal Diagnostic Imaging Vivek Kalia, MD MPH October 02, 2019 Course: Sports Medicine for the Primary Care Physician Department of Radiology University of Michigan @VivekKaliaMD [email protected] Objectives • To review anatomy of joints which commonly present for evaluation in the primary care setting • To review basic clinical features of particular musculoskeletal conditions affecting these joints • To review key imaging features of particular musculoskeletal conditions affecting these joints Outline • Joints – Shoulder – Hip • Rotator Cuff Tendinosis / • Osteoarthritis Tendinitis • (Greater) Trochanteric bursitis • Rotator Cuff Tears • Hip Abductor (Gluteal Tendon) • Adhesive Capsulitis (Frozen Tears Shoulder) • Hamstrings Tendinosis / Tears – Elbow – Knee • Lateral Epicondylitis • Osteoarthritis • Medical Epicondylitis • Popliteal / Baker’s cyst – Hand/Wrist • Meniscus Tear • Rheumatoid Arthritis • Ligament Tear • Osteoarthritis • Cartilage Wear Outline • Joints – Ankle/Foot • Osteoarthritis • Plantar Fasciitis • Spine – Degenerative Disc Disease – Wedge Compression Deformity / Fracture Shoulder Shoulder Rotator Cuff Tendinosis / Tendinitis • Rotator cuff comprised of 4 muscles/tendons: – Supraspinatus – Infraspinatus – Teres minor – Subscapularis • Theory of rotator cuff degeneration / tearing with time: – Degenerative partial-thickness tears allow superior migration of the humeral head in turn causes abrasion of the rotator cuff tendons against the undersurface of the acromion full-thickness tears may progress to -
Rehabilitation Guidelines for Type I and Type II Rotator Cuff Repair and Isolated Subscapularis Repair
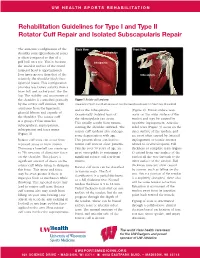
UW HEALTH SPORTS REHABILITATION Rehabilitation Guidelines for Type I and Type II Rotator Cuff Repair and Isolated Subscapularis Repair The anatomic configuration of the Back View Front View shoulder joint (glenohumeral joint) Supraspinatus is often compared to that of a golf ball on a tee. This is because Infraspinatus the articular surface of the round humeral head is approximately Teres four times greater than that of the Minor Subscapularis relatively flat shoulder blade face (glenoid fossa). This configuration provides less boney stability than a truer ball and socket joint, like the hip. The stability and movement of the shoulder is controlled primarily Figure 1 Rotator cuff anatomy by the rotator cuff muscles, with Image property of Primal Pictures, Ltd., primalpictures.com. Use of this image without authorization from Primal Pictures, Ltd. is prohibited. assistance from the ligaments, and/or the infraspinatus. (Figure 2). Bursal surface tears glenoid labrum and capsule of Occasionally isolated tears of occur on the outer surface of the the shoulder. The rotator cuff the subscapularis can occur. tendon and may be caused by is a group of four muscles: This usually results from trauma repetitive impingement. Articular subscapularis, supraspinatus, rotating the shoulder outward. The sided tears (Figure 3) occur on the infraspinatus and teres minor rotator cuff tendons also undergo inner surface of the tendon, and (Figure 1). some degeneration with age. are most often caused by internal Rotator cuff tears can occur from This process alone can lead to impingement or tensile stresses repeated stress or from trauma. rotator cuff tears in older patients. related to overhead sports.