FYN-TRAF3IP2 and KHDRBS1-LCK Hijack T Cell Receptor Signaling in Peripheral T Cell Lymphoma, Not Otherwise Specifed
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SRC Antibody - N-Terminal Region (ARP32476 P050) Data Sheet
SRC antibody - N-terminal region (ARP32476_P050) Data Sheet Product Number ARP32476_P050 Product Name SRC antibody - N-terminal region (ARP32476_P050) Size 50ug Gene Symbol SRC Alias Symbols ASV; SRC1; c-SRC; p60-Src Nucleotide Accession# NM_005417 Protein Size (# AA) 536 amino acids Molecular Weight 60kDa Product Format Lyophilized powder NCBI Gene Id 6714 Host Rabbit Clonality Polyclonal Official Gene Full Name V-src sarcoma (Schmidt-Ruppin A-2) viral oncogene homolog (avian) Gene Family SH2D This is a rabbit polyclonal antibody against SRC. It was validated on Western Blot by Aviva Systems Biology. At Aviva Systems Biology we manufacture rabbit polyclonal antibodies on a large scale (200-1000 Description products/month) of high throughput manner. Our antibodies are peptide based and protein family oriented. We usually provide antibodies covering each member of a whole protein family of your interest. We also use our best efforts to provide you antibodies recognize various epitopes of a target protein. For availability of antibody needed for your experiment, please inquire (). Peptide Sequence Synthetic peptide located within the following region: QTPSKPASADGHRGPSAAFAPAAAEPKLFGGFNSSDTVTSPQRAGPLAGG This gene is highly similar to the v-src gene of Rous sarcoma virus. This proto-oncogene may play a role in the Description of Target regulation of embryonic development and cell growth. SRC protein is a tyrosine-protein kinase whose activity can be inhibited by phosphorylation by c-SRC kinase. Mutations in this gene could be involved in the -

Splicing Regulatory Factors in Breast Cancer Hallmarks and Disease Progression
www.oncotarget.com Oncotarget, 2019, Vol. 10, (No. 57), pp: 6021-6037 Review Splicing regulatory factors in breast cancer hallmarks and disease progression Esmee Koedoot1, Liesanne Wolters1, Bob van de Water1 and Sylvia E. Le Dévédec1 1Division of Drug Discovery and Safety, LACDR, Leiden University, Leiden, The Netherlands Correspondence to: Sylvia E. Le Dévédec, email: [email protected] Keywords: hallmarks of cancer; breast cancer; alternative splicing; splice factors; RNA sequencing Received: April 23, 2019 Accepted: August 29, 2019 Published: October 15, 2019 Copyright: Koedoot et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License 3.0 (CC BY 3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. ABSTRACT By regulating transcript isoform expression levels, alternative splicing provides an additional layer of protein control. Recent studies show evidence that cancer cells use different splicing events to fulfill their requirements in order to develop, progress and metastasize. However, there has been less attention for the role of the complex catalyzing the complicated multistep splicing reaction: the spliceosome. The spliceosome consists of multiple sub-complexes in total comprising 244 proteins or splice factors and 5 associated RNA molecules. Here we discuss the role of splice factors in the oncogenic processes tumors cells need to fulfill their oncogenic properties (the so-called the hallmarks of cancer). Despite the fact that splice factors have been investigated only recently, they seem to play a prominent role in already five hallmarks of cancer: angiogenesis, resisting cell death, sustaining proliferation, deregulating cellular energetics and invasion and metastasis formation by affecting major signaling pathways such as epithelial-to-mesenchymal transition, the Warburg effect, DNA damage response and hormone receptor dependent proliferation. -

University of Groningen BRCA2 Deficiency Instigates Cgas
University of Groningen BRCA2 deficiency instigates cGAS-mediated inflammatory signaling and confers sensitivity to tumor necrosis factor-alpha-mediated cytotoxicity Heijink, Anne Margriet; Talens, Francien; Jae, Lucas T; van Gijn, Stephanie E; Fehrmann, Rudolf S N; Brummelkamp, Thijn R; van Vugt, Marcel A T M Published in: Nature Communications DOI: 10.1038/s41467-018-07927-y IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 2019 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): Heijink, A. M., Talens, F., Jae, L. T., van Gijn, S. E., Fehrmann, R. S. N., Brummelkamp, T. R., & van Vugt, M. A. T. M. (2019). BRCA2 deficiency instigates cGAS-mediated inflammatory signaling and confers sensitivity to tumor necrosis factor-alpha-mediated cytotoxicity. Nature Communications, 10(1), [100]. https://doi.org/10.1038/s41467-018-07927-y Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). The publication may also be distributed here under the terms of Article 25fa of the Dutch Copyright Act, indicated by the “Taverne” license. More information can be found on the University of Groningen website: https://www.rug.nl/library/open-access/self-archiving-pure/taverne- amendment. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -
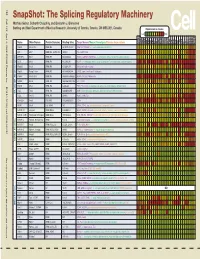
Snapshot: the Splicing Regulatory Machinery Mathieu Gabut, Sidharth Chaudhry, and Benjamin J
192 Cell SnapShot: The Splicing Regulatory Machinery Mathieu Gabut, Sidharth Chaudhry, and Benjamin J. Blencowe 133 Banting and Best Department of Medical Research, University of Toronto, Toronto, ON M5S 3E1, Canada Expression in mouse , April4, 2008©2008Elsevier Inc. Low High Name Other Names Protein Domains Binding Sites Target Genes/Mouse Phenotypes/Disease Associations Amy Ceb Hip Hyp OB Eye SC BM Bo Ht SM Epd Kd Liv Lu Pan Pla Pro Sto Spl Thy Thd Te Ut Ov E6.5 E8.5 E10.5 SRp20 Sfrs3, X16 RRM, RS GCUCCUCUUC SRp20, CT/CGRP; −/− early embryonic lethal E3.5 9G8 Sfrs7 RRM, RS, C2HC Znf (GAC)n Tau, GnRH, 9G8 ASF/SF2 Sfrs1 RRM, RS RGAAGAAC HipK3, CaMKIIδ, HIV RNAs; −/− embryonic lethal, cond. KO cardiomyopathy SC35 Sfrs2 RRM, RS UGCUGUU AChE; −/− embryonic lethal, cond. KO deficient T-cell maturation, cardiomyopathy; LS SRp30c Sfrs9 RRM, RS CUGGAUU Glucocorticoid receptor SRp38 Fusip1, Nssr RRM, RS ACAAAGACAA CREB, type II and type XI collagens SRp40 Sfrs5, HRS RRM, RS AGGAGAAGGGA HipK3, PKCβ-II, Fibronectin SRp55 Sfrs6 RRM, RS GGCAGCACCUG cTnT, CD44 DOI 10.1016/j.cell.2008.03.010 SRp75 Sfrs4 RRM, RS GAAGGA FN1, E1A, CD45; overexpression enhances chondrogenic differentiation Tra2α Tra2a RRM, RS GAAARGARR GnRH; overexpression promotes RA-induced neural differentiation SR and SR-Related Proteins Tra2β Sfrs10 RRM, RS (GAA)n HipK3, SMN, Tau SRm160 Srrm1 RS, PWI AUGAAGAGGA CD44 SWAP Sfrs8 RS, SWAP ND SWAP, CD45, Tau; possible asthma susceptibility gene hnRNP A1 Hnrnpa1 RRM, RGG UAGGGA/U HipK3, SMN2, c-H-ras; rheumatoid arthritis, systemic lupus -

RET Gene Fusions in Malignancies of the Thyroid and Other Tissues
G C A T T A C G G C A T genes Review RET Gene Fusions in Malignancies of the Thyroid and Other Tissues Massimo Santoro 1,*, Marialuisa Moccia 1, Giorgia Federico 1 and Francesca Carlomagno 1,2 1 Department of Molecular Medicine and Medical Biotechnology, University of Naples “Federico II”, 80131 Naples, Italy; [email protected] (M.M.); [email protected] (G.F.); [email protected] (F.C.) 2 Institute of Endocrinology and Experimental Oncology of the CNR, 80131 Naples, Italy * Correspondence: [email protected] Received: 10 March 2020; Accepted: 12 April 2020; Published: 15 April 2020 Abstract: Following the identification of the BCR-ABL1 (Breakpoint Cluster Region-ABelson murine Leukemia) fusion in chronic myelogenous leukemia, gene fusions generating chimeric oncoproteins have been recognized as common genomic structural variations in human malignancies. This is, in particular, a frequent mechanism in the oncogenic conversion of protein kinases. Gene fusion was the first mechanism identified for the oncogenic activation of the receptor tyrosine kinase RET (REarranged during Transfection), initially discovered in papillary thyroid carcinoma (PTC). More recently, the advent of highly sensitive massive parallel (next generation sequencing, NGS) sequencing of tumor DNA or cell-free (cfDNA) circulating tumor DNA, allowed for the detection of RET fusions in many other solid and hematopoietic malignancies. This review summarizes the role of RET fusions in the pathogenesis of human cancer. Keywords: kinase; tyrosine kinase inhibitor; targeted therapy; thyroid cancer 1. The RET Receptor RET (REarranged during Transfection) was initially isolated as a rearranged oncoprotein upon the transfection of a human lymphoma DNA [1]. -

Gorilla Results
Results http://cbl-gorilla.cs.technion.ac.il/GOrilla/2l4v7a1a/GOResultsPROCESS... P-value color scale > 10-3 10-3 to 10-5 10-5 to 10-7 10-7 to 10-9 < 10-9 null Description P-value Enrichment (N, B, n, b) Genes [-] Hide genes ATF3 - activating transcription factor 3 JUN - jun proto-oncogene ADM - adrenomedullin NAMPT - nicotinamide phosphoribosyltransferase GO:0008284 positive regulation of cell proliferation 6.46E-6 4.37 (297,17,40,10) C7orf68 - chromosome 7 open reading frame 68 FOSL2 - fos-like antigen 2 TNFAIP3 - tumor necrosis factor, alpha-induced protein 3 VEGFA - vascular endothelial growth factor a SOX9 - sry (sex determining region y)-box 9 EDN2 - endothelin 2 [-] Hide genes JUN - jun proto-oncogene SPRR1B - small proline-rich protein 1b GO:0030855 epithelial cell differentiation 4.33E-5 5.20 (297,10,40,7) SPRR1A - small proline-rich protein 1a PLAUR - plasminogen activator, urokinase receptor VEGFA - vascular endothelial growth factor a TXNIP - thioredoxin interacting protein ELF3 - e74-like factor 3 (ets domain transcription factor, epithelial-specific ) [-] Hide genes JUN - jun proto-oncogene KHDRBS1 - kh domain containing, rna binding, signal transduction associated 1 MAFF - v-maf musculoaponeurotic fibrosarcoma oncogene homolog f (avian) VEGFA - vascular endothelial growth factor a RRAS - related ras viral (r-ras) oncogene homolog SOX9 - sry (sex determining region y)-box 9 SAT1 - spermidine/spermine n1-acetyltransferase 1 GEM - gtp binding protein overexpressed in skeletal muscle GO:0006807 nitrogen compound metabolic process -

Flexible, Unbiased Analysis of Biological Characteristics Associated with Genomic Regions
bioRxiv preprint doi: https://doi.org/10.1101/279612; this version posted March 22, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. BioFeatureFinder: Flexible, unbiased analysis of biological characteristics associated with genomic regions Felipe E. Ciamponi 1,2,3; Michael T. Lovci 2; Pedro R. S. Cruz 1,2; Katlin B. Massirer *,1,2 1. Structural Genomics Consortium - SGC, University of Campinas, SP, Brazil. 2. Center for Molecular Biology and Genetic Engineering - CBMEG, University of Campinas, Campinas, SP, Brazil. 3. Graduate program in Genetics and Molecular Biology, PGGBM, University of Campinas, Campinas, SP, Brazil. *Corresponding author: [email protected] Mailing address: Center for Molecular Biology and Genetic Engineering - CBMEG, University of Campinas, Campinas, SP, Brazil. Av Candido Rondo, 400 Cidade Universitária CEP 13083-875, Campinas, SP Phone: 55-19-98121-937 bioRxiv preprint doi: https://doi.org/10.1101/279612; this version posted March 22, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. Abstract BioFeatureFinder is a novel algorithm which allows analyses of many biological genomic landmarks (including alternatively spliced exons, DNA/RNA- binding protein binding sites, and gene/transcript functional elements, nucleotide content, conservation, k-mers, secondary structure) to identify distinguishing features. -

Rabbit Anti-CIKS/FITC Conjugated Antibody
SunLong Biotech Co.,LTD Tel: 0086-571- 56623320 Fax:0086-571- 56623318 E-mail:[email protected] www.sunlongbiotech.com Rabbit Anti-CIKS/FITC Conjugated antibody SL6202R-FITC Product Name: Anti-CIKS/FITC Chinese Name: FITC标记的核因子NFκB激活蛋白1抗体 Act 1; ACT1; Activator of cAMP responsive element modulator (CREM) in testis; Adapter protein CIKS; C6ORF4; C6ORF5; C6ORF6; Chromosome 6 Open Reading Frame 4; Chromosome 6 Open Reading Frame 5; Chromosome 6 Open Reading Frame Alias: 6; CIKS; CIKS_HUMAN; Connection to IKK and SAPK / JNK; Connection to IKK and SAPK/JNK; Nuclear Factor Kappa B Activator 1; Nuclear factor NF kappa B activator 1; Nuclear factor NF-kappa-B activator 1; TRAF3 interacting protein 2; TRAF3-interacting protein 2; TRAF3IP2. Organism Species: Rabbit Clonality: Polyclonal React Species: Human,Mouse,Rat,Chicken,Dog,Pig,Cow,Rabbit, IF=1:50-200 Applications: not yet tested in other applications. optimal dilutions/concentrations should be determined by the end user. Molecular weight: 63kDa Form: Lyophilized or Liquid Concentration: 1mg/mlwww.sunlongbiotech.com KLH conjugated synthetic peptide derived from human Nuclear Factor Kappa B immunogen: Activator 1 Lsotype: IgG Purification: affinity purified by Protein A Storage Buffer: 0.01M TBS(pH7.4) with 1% BSA, 0.03% Proclin300 and 50% Glycerol. Store at -20 °C for one year. Avoid repeated freeze/thaw cycles. The lyophilized antibody is stable at room temperature for at least one month and for greater than a year Storage: when kept at -20°C. When reconstituted in sterile pH 7.4 0.01M PBS or diluent of antibody the antibody is stable for at least two weeks at 2-4 °C. -

The Genetics of Bipolar Disorder
Molecular Psychiatry (2008) 13, 742–771 & 2008 Nature Publishing Group All rights reserved 1359-4184/08 $30.00 www.nature.com/mp FEATURE REVIEW The genetics of bipolar disorder: genome ‘hot regions,’ genes, new potential candidates and future directions A Serretti and L Mandelli Institute of Psychiatry, University of Bologna, Bologna, Italy Bipolar disorder (BP) is a complex disorder caused by a number of liability genes interacting with the environment. In recent years, a large number of linkage and association studies have been conducted producing an extremely large number of findings often not replicated or partially replicated. Further, results from linkage and association studies are not always easily comparable. Unfortunately, at present a comprehensive coverage of available evidence is still lacking. In the present paper, we summarized results obtained from both linkage and association studies in BP. Further, we indicated new potential interesting genes, located in genome ‘hot regions’ for BP and being expressed in the brain. We reviewed published studies on the subject till December 2007. We precisely localized regions where positive linkage has been found, by the NCBI Map viewer (http://www.ncbi.nlm.nih.gov/mapview/); further, we identified genes located in interesting areas and expressed in the brain, by the Entrez gene, Unigene databases (http://www.ncbi.nlm.nih.gov/entrez/) and Human Protein Reference Database (http://www.hprd.org); these genes could be of interest in future investigations. The review of association studies gave interesting results, as a number of genes seem to be definitively involved in BP, such as SLC6A4, TPH2, DRD4, SLC6A3, DAOA, DTNBP1, NRG1, DISC1 and BDNF. -

SPINAL MUSCULAR ATROPHY: PATHOLOGY, DIAGNOSIS, CLINICAL PRESENTATION, THERAPEUTIC STRATEGIES & TREATMENTS Content
SPINAL MUSCULAR ATROPHY: PATHOLOGY, DIAGNOSIS, CLINICAL PRESENTATION, THERAPEUTIC STRATEGIES & TREATMENTS Content 1. DISCLAIMER 2. INTRODUCTION 3. SPINAL MUSCULAR ATROPHY: PATHOLOGY, DIAGNOSIS, CLINICAL PRESENTATION, THERAPEUTIC STRATEGIES & TREATMENTS 4. BIBLIOGRAPHY 5. GLOSSARY OF MEDICAL TERMS 1 SPINAL MUSCULAR ATROPHY: PATHOLOGY, DIAGNOSIS, CLINICAL PRESENTATION, THERAPEUTIC STRATEGIES & TREATMENTS Disclaimer The information in this document is provided for information purposes only. It does not constitute advice on any medical, legal, or regulatory matters and should not be used in place of consultation with appropriate medical, legal, or regulatory personnel. Receipt or use of this document does not create a relationship between the recipient or user and SMA Europe, or any other third party. The information included in this document is presented as a synopsis, may not be exhaustive and is dated November 2020. As such, it may no longer be current. Guidance from regulatory authorities, study sponsors, and institutional review boards should be obtained before taking action based on the information provided in this document. This document was prepared by SMA Europe. SMA Europe cannot guarantee that it will meet requirements or be error-free. The users and recipients of this document take on any risk when using the information contained herein. SMA Europe is an umbrella organisation, founded in 2006, which includes spinal muscular atrophy (SMA) patient and research organisations from across Europe. SMA Europe campaigns to improve the quality of life of people who live with SMA, to bring effective therapies to patients in a timely and sustainable way, and to encourage optimal patient care. SMA Europe is a non-profit umbrella organisation that consists of 23 SMA patients and research organisations from 22 countries across Europe. -

Loss of B Cells in Patients with Heterozygous Mutations in IKAROS
The new england journal of medicine Original Article Loss of B Cells in Patients with Heterozygous Mutations in IKAROS H.S. Kuehn, B. Boisson, C. Cunningham-Rundles, J. Reichenbach, A. Stray-Pedersen, E.W. Gelfand, P. Maffucci, K.R. Pierce, J.K. Abbott, K.V. Voelkerding, S.T. South, N.H. Augustine, J.S. Bush, W.K. Dolen, B.B. Wray, Y. Itan, A. Cobat, H.S. Sorte, S. Ganesan, S. Prader, T.B. Martins, M.G. Lawrence, J.S. Orange, K.R. Calvo, J.E. Niemela, J.-L. Casanova, T.A. Fleisher, H.R. Hill, A. Kumánovics, M.E. Conley, and S.D. Rosenzweig ABSTRACT BACKGROUND The authors’ full names, academic de- Common variable immunodeficiency (CVID) is characterized by late-onset hypo- grees, and affiliations are listed in the gammaglobulinemia in the absence of predisposing factors. The genetic cause is Appendix. Address reprint requests to Dr. Conley at St. Giles Laboratory of Human unknown in the majority of cases, and less than 10% of patients have a family Genetics of Infectious Diseases, Rocke- history of the disease. Most patients have normal numbers of B cells but lack feller University, 1230 York Ave., Box 163, plasma cells. New York, NY 10065-6399, or at mconley@ rockefeller . edu. METHODS Drs. Kuehn and Boisson and Drs. Conley We used whole-exome sequencing and array-based comparative genomic hybrid- and Rosenzweig contributed equally to this article. ization to evaluate a subset of patients with CVID and low B-cell numbers. Mutant proteins were analyzed for DNA binding with the use of an electrophoretic mobility- N Engl J Med 2016;374:1032-43.