Using Collaborative Improvement to Enhance Postpartum Family Planning in Niger
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

World Bank Document
SFG1950 Public Disclosure Authorized _________ Projet d’Appui à l’Agriculture Sensible aux Risques Climatiques (PASEC) _________ Public Disclosure Authorized Public Disclosure Authorized CADRE DE GESTION ENVIRONNEMENTAL ET SOCIAL (CGES) Public Disclosure Authorized RAPPORT DEFINITIF Janvier 2016 TABLE DES MATIERES ESMF SUMMARY ............................................................................................................................................... 7 RESUME ............................................................................................................................................................... 9 INTRODUCTION ............................................................................................................................................... 11 CONTEXTE ........................................................................................................................................................ 11 OBJECTIFS DE L’ÉTUDE ..................................................................................................................................... 11 MÉTHODOLOGIE ................................................................................................................................................ 12 STRUCTURATION DU RAPPORT .......................................................................................................................... 12 1. DESCRIPTION DU PROJET ................................................................................................................. -

Aperçu Des Besoins Humanitaires Niger
CYCLE DE APERÇU DES BESOINS PROGRAMME HUMANITAIRE 2021 HUMANITAIRES PUBLIÉ EN JANVIER 2021 NIGER 01 APERÇU DES BESOINS HUMANITAIRES 2021 À propos Pour les plus récentes mises à jour Ce document est consolidé par OCHA pour le compte de l’Équipe humanitaire pays et des partenaires. Il présente une compréhension commune de la crise, notamment les besoins OCHA coordonne l’action humanitaire pour humanitaires les plus pressants et le nombre estimé de garantir que les personnes affectées par une personnes ayant besoin d’assistance. Il constitue une base crise reçoivent l’assistance et la protection dont elles ont besoin. OCHA s’efforce factuelle aidant à informer la planification stratégique conjointe de surmonter les obstacles empêchant de la réponse. l’assistance humanitaire de joindre les personnes affectées par des crises et PHOTO DE COUVERTURE est chef de file dans la mobilisation de l’assistance et de ressources pour le compte MAINÉ SOROA/DIFFA, NIGER du système humanitaire. Ménage PDIs du village Kublé www.unocha.org/niger Photo: IRC/Niger, Novembre 2020 twitter.com/OCHA_Niger?lang=fr Les désignations employées et la présentation des éléments dans le présent rapport ne signifient pas l’expression de quelque opinion que ce soit de la part du Secrétariat des Nations Unies concernant le statut juridique d’un pays, d’un territoire, d’une ville ou d’une zone ou de leurs autorités ou concernant la délimitation de ses frontières ou de ses limites. La réponse humanitaire est destinée à être le site Web central des outils et des services de Gestion de l’information permettant l’échange d’informations entre les clusters et les membres de l’IASC intervenant dans une crise. -

(Between Warrior and Helplessness in the Valley of Azawaɤ ) Appendix 1: Northern Mali and Niger Tuareg Participation in Violenc
Appendix 1: Northern Mali and Niger Tuareg Participation in violence as perpetrators, victims, bystanders from November 2013 to August 2014 (Between Warrior and Helplessness in the Valley of Azawaɤ ) Northern Mali/Niger Tuareg participation in violence (perpetrators, victims, bystanders) November 2013 – August 2014. Summarized list of sample incidents from Northern Niger and Northern Mali from reporting tracking by US Military Advisory Team, Niger/Mali – Special Operations Command – Africa, USAFRICOM. Entries in Red indicate no Tuareg involvement; Entries in Blue indicate Tuareg involvement as victims and/or perpetrators. 28 November – Niger FAN arrests Beidari Moulid in Niamey for planning terror attacks in Niger. 28 November – MNLA organizes protest against Mali PMs Visit to Kidal; Mali army fires on protestors killing 1, injuring 5. 30 November – AQIM or related forces attack French forces in Menaka with Suicide bomber. 9 December – AQIM and French forces clash in Asler, with 19 casualties. 14 December – AQIM or related forces employ VBIED against UN and Mali forces in Kidal with 3 casualties. 14 December – MUJWA/AQIM assault a Tuareg encampment with 2 casualties in Tarandallet. 13 January – AQIM or related forces kidnap MNLA political leader in Tessalit. 16 January – AQIM kidnap/executes MNLA officer in Abeibera. 17 January – AQIM or related forces plant explosive device near Christian school and church in Gao; UN forces found/deactivated device. 20 January – AQIM or related forces attacks UN forces with IED in Kidal, 5 WIA. 22 January – AQIM clashes with French Army forces in Timbuktu with 11 Jihadist casualties. 24 January – AQIM or related forces fires two rockets at city of Kidal with no casualties. -

F:\Niger En Chiffres 2014 Draft
Le Niger en Chiffres 2014 Le Niger en Chiffres 2014 1 Novembre 2014 Le Niger en Chiffres 2014 Direction Générale de l’Institut National de la Statistique 182, Rue de la Sirba, BP 13416, Niamey – Niger, Tél. : +227 20 72 35 60 Fax : +227 20 72 21 74, NIF : 9617/R, http://www.ins.ne, e-mail : [email protected] 2 Le Niger en Chiffres 2014 Le Niger en Chiffres 2014 Pays : Niger Capitale : Niamey Date de proclamation - de la République 18 décembre 1958 - de l’Indépendance 3 août 1960 Population* (en 2013) : 17.807.117 d’habitants Superficie : 1 267 000 km² Monnaie : Francs CFA (1 euro = 655,957 FCFA) Religion : 99% Musulmans, 1% Autres * Estimations à partir des données définitives du RGP/H 2012 3 Le Niger en Chiffres 2014 4 Le Niger en Chiffres 2014 Ce document est l’une des publications annuelles de l’Institut National de la Statistique. Il a été préparé par : - Sani ALI, Chef de Service de la Coordination Statistique. Ont également participé à l’élaboration de cette publication, les structures et personnes suivantes de l’INS : les structures : - Direction des Statistiques et des Etudes Economiques (DSEE) ; - Direction des Statistiques et des Etudes Démographiques et Sociales (DSEDS). les personnes : - Idrissa ALICHINA KOURGUENI, Directeur Général de l’Institut National de la Statistique ; - Ibrahim SOUMAILA, Secrétaire Général P.I de l’Institut National de la Statistique. Ce document a été examiné et validé par les membres du Comité de Lecture de l’INS. Il s’agit de : - Adamou BOUZOU, Président du comité de lecture de l’Institut National de la Statistique ; - Djibo SAIDOU, membre du comité - Mahamadou CHEKARAOU, membre du comité - Tassiou ALMADJIR, membre du comité - Halissa HASSAN DAN AZOUMI, membre du comité - Issiak Balarabé MAHAMAN, membre du comité - Ibrahim ISSOUFOU ALI KIAFFI, membre du comité - Abdou MAINA, membre du comité. -

REPUBLIQUE DU NIGER Fraternité
REPUBLIQUE DU NIGER Fraternité – Travail – Progrès Public Disclosure Authorized ======================================== CABINET DU PREMIER MINISTRE ====================================================== Projet de Gestion des Risques de Catastrophes et de Développement Urbain Public Disclosure Authorized CADRE DE GESTION ENVIRONNEMENTAL ET SOCIAL (CGES) Public Disclosure Authorized RAPPORT ACTUALISE Version Définitive Février 2019 Public Disclosure Authorized TABLE DES MATIERES TABLE DES MATIERES .................................................................................................................................................I LISTE DES CARTES .................................................................................................................................................... III LISTE DES TABLEAUX ............................................................................................................................................... IV ACRONYMES ................................................................................................................................................................ VI INTRODUCTION ............................................................................................................................................................ 9 I. DESCRIPTION DU PROJET ................................................................................................................... 11 1.1. OBJECTIFS DE DEVELOPPEMENT .................................................................................................................... -

Foreign Assistance
TREATIES AND OTHER INTERNATIONAL ACTS SERIES 18-126 ________________________________________________________________________ FOREIGN ASSISTANCE Millennium Challenge Compact Between the UNITED STATES OF AMERICA and NIGER Signed at Washington July 29, 2016 with Annexes NOTE BY THE DEPARTMENT OF STATE Pursuant to Public Law 89—497, approved July 8, 1966 (80 Stat. 271; 1 U.S.C. 113)— “. .the Treaties and Other International Acts Series issued under the authority of the Secretary of State shall be competent evidence . of the treaties, international agreements other than treaties, and proclamations by the President of such treaties and international agreements other than treaties, as the case may be, therein contained, in all the courts of law and equity and of maritime jurisdiction, and in all the tribunals and public offices of the United States, and of the several States, without any further proof or authentication thereof.” NIGER Foreign Assistance Millennium Challenge Compact signed at Washington July 29, 2016; Entered into force January 26, 2018. With annexes. MILLENNIUM CHALLENGE COMPACT BETWEEN THE UNITED STATES OF AMERICA ACTING THROUGH THE MILLENNIUM CIIA£LENGE CORPORATION AND THE REPUBLIC OF NIGER ACTING THROUGH THE MINISTRY IN CHARGE OF FOREIGN AFFAIRS AND COOPERATION MILLENNIUM CHALLENGE COMPACT TABLE OF CONTENTS ARTICLE 1. GOAL AND OBJECTIVES .................................................................................... 1 Section 1.1 Compact Goal ..................................................................................................... -

«Fichier Electoral Biométrique Au Niger»
«Fichier Electoral Biométrique au Niger» DIFEB, le 16 Août 2019 SOMMAIRE CEV Plan de déploiement Détails Zone 1 Détails Zone 2 Avantages/Limites CEV Centre d’Enrôlement et de Vote CEV: Centre d’Enrôlement et de Vote Notion apparue avec l’introduction de la Biométrie dans le système électoral nigérien. ▪ Avec l’utilisation de matériels sensible (fragile et lourd), difficile de faire de maison en maison pour un recensement, C’est l’emplacement physique où se rendront les populations pour leur inscription sur la Liste Electorale Biométrique (LEB) dans une localité donnée. Pour ne pas désorienter les gens, le CEV servira aussi de lieu de vote pour les élections à venir. Ainsi, le CEV contiendra un ou plusieurs bureaux de vote selon le nombre de personnes enrôlées dans le centre et conformément aux dispositions de création de bureaux de vote (Art 79 code électoral) COLLECTE DES INFORMATIONS SUR LES CEV Création d’une fiche d’identification de CEV; Formation des acteurs locaux (maire ou son représentant, responsable d’état civil) pour le remplissage de la fiche; Remplissage des fiches dans les communes (maire ou son représentant, responsable d’état civil et 3 personnes ressources); Centralisation et traitement des fiches par commune; Validation des CEV avec les acteurs locaux (Traitement des erreurs sur place) Liste définitive par commune NOMBRE DE CEV PAR REGION Région Nombre de CEV AGADEZ 765 TAHOUA 3372 DOSSO 2398 TILLABERY 3742 18 400 DIFFA 912 MARADI 3241 ZINDER 3788 NIAMEY 182 ETRANGER 247 TOTAL 18 647 Plan de Déploiement Plan de Déploiement couvrir tous les 18 647 CEV : Sur une superficie de 1 267 000 km2 Avec une population électorale attendue de 9 751 462 Et 3 500 kits (3000 kits fixes et 500 tablettes) ❖ KIT = Valise d’enrôlement constitués de plusieurs composants (PC ou Tablette, lecteur d’empreintes digitales, appareil photo, capteur de signature, scanner, etc…) Le pays est divisé en 2 zones d’intervention (4 régions chacune) et chaque région en 5 aires. -
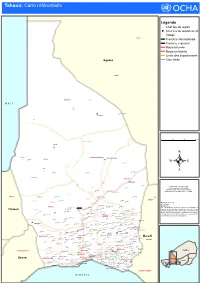
Ref Tahoua A1.Pdf
Tahoua: Carte référentielle Légende Chef lieu de région Chef lieu de département ! Village ARLIT Frontière internationale Frontière régionale Route bitumée Route en latérite Limite des départements Agadez Cour d'eau INGAL TASSARA Tassara M A L I Tezalite ! Nakonawa Sami ! TASSARA Tillia 0 25 50 75 kms Tchin Tabaradene TILLIA Chinwaren TCHINTABARADENE TCHIN TABARADEN ! Agando TILLIA ! Abalak Intikane ! Télemsès Efeinatas ! Amerkay ! . ! Assagueiguei ! ABALAK Kao ABALAK ! Taza ! Tamaya Creation Date: 20 Février 2015 Kao Assas ! Projection/Datum: GSC/WGS84 Web Resources: www.unocha.org/niger Haringué Ibessetene ! ! Akoubounou Nominal Scale at A1 paper size: 1: 750 000 Affala Tabalak Takanamat Takanamat Akarzaza ABALA ! Kafate ! Tabalak ! Barmou ! In Lelou BERMO ! In Aouara Alagaza ! ! In Najin Takanamat ! Toumfafi Map data source(s): ! OCHA Niger Ibazaouane ! DjiguinaLoudou Karkamat Disclaimers: TAHOUA Koureya ! ! ! ! Tahoua I et II Tahoua ! The designations employed and the presentation of I-n-Safari KardagaDafan Kaloma Kalfou Azeye Tebaram ! ! ! Kounkouzout material on this map do not imply the expression of any Tillaberi ! ! Ibohamane Labandam ! opinion whatsoever on the part of the Secretariat of the Tebaram In Karkada Kalfou Sokolé ! Edir ! ! Tchingaran ! Sabon GariAlibou Keita Ibohamane Gadamata Aliou ! United Nations concerning the legal status of any country, ! ! ! ! ! Tagatil territory, city or area or of its authorities, or concerning the May Farin Kay Founkouey KEITA Bargat ! ! ! Kéda ! Toudou KEITA ! Zango Amadou delimitation -

Retour Du Refoulé Et Effet Chef-Lieu. Frédéric Giraut
Retour du refoulé et effet chef-lieu. Frédéric Giraut To cite this version: Frédéric Giraut. Retour du refoulé et effet chef-lieu. : Analyse d’une refonte politico-administrative virtuelle au Niger. UMR PRODIG (Coll Graphigeo), pp.100, 1999. hal-00162001 HAL Id: hal-00162001 https://hal.archives-ouvertes.fr/hal-00162001 Submitted on 19 Jul 2007 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. RETOUR DU REFOULÉ ET EFFET CHEF-LIEU Analyse d’une refonte politico- administrative virtuelle au Niger GÉO Frédéric GIRAUT GRAFI 1999-7 Collection mémoires et documents de l’ UMR PRODIG RETOUR DU REFOULÉ ET EFFET CHEF-LIEU Analyse d’une refonte politico- administrative virtuelle au Niger DANS LA MÊME COLLECTION (ISSN 1281-6477) La Francophonie au Vanuatu. Géographie d’un choc culturel par Maud Lasseur (Grafigéo 1997, n° 1, ISBN 2-901560-30-X) La géographie tropicale allemande par Hélène Sallard (Grafigéo 1997, n° 2, ISBN 2-901560-31-8) Le repeuplement de la côte Est de Pentecôte. Territoires et mobilité au Vanuatu par Patricia Siméoni (Grafigéo 1997, n° 3, ISBN 2-901560-32-6) B. comme Big Man Hommage à Joël Bonnemaison (Grafigéo 1998, n° 4, ISBN 2-901560-34-2) Siem Reap-Angkor Une région du Nord-Cambodge en voie de mutation par Christel Thibault (Grafigéo 1998, n° 5, ISBN 2-901560-36-9) La colonisation mennonite en Bolivie par Gwenaelle Pasco (Grafigéo 1999, n° 6, ISBN 2-901560-37-7) SOUS PRESSE Transition malienne, décentralisation, gestion communale bamakoise par Monique Bertrand (Grafigéo 1999, n° 8) À PARAÎTRE Inventaire géomorphologique de la région de Fejej (Sud de l’Ethiopie). -

NER Zones De Couverture Programme Spotlight
NIGER Tillabéri - Initiative Spotlight Programme Niger - Communes d’intervention 2019-2022* Janvier 2019 Abala Sanam MALI Tondikiwindi MAI TALAKIA Anzourou Inatès Banibangou TALCHO Banibangou KOUFFEY Filingué Abala Ouallam TIDANI Abala BANIZOUMBOU Ayerou FAZAOU Sanam Dingazi TillabériAyerou GARBEY MALO KOIRA TOUNFALIS Sakoïra KOIRA TEGUI Tondikiwindi Gorouol DABRE CHICAL CHANYASSOU Sinder Ouallam SARGANE TILLAKAINA KOIRA ZENO Filingué KABIA Anzourou KOSSEY MAI TALAKIA BAGDAD GAOBANDA GUESSE HASSOU DINGAZI BANDA GARIE Tillabéri GOUTOUMBOU GOUROUKE Kourfeye Centre LOUMA TALCHO Bankilaré DAIBERI Dessa DIEP BERI KOUFFEY SIMIRI KANDA Bankilaré GANDOU BERI Ouallam TIDANI BANIZOUMBOU Filingué MORIBANE TASSI DEYBANDA ITCHIGUINE Bibiyergou FAZAOU TOMBO Méhana Simiri Dingazi Imanan KOKOMANI HAOUSSA Sakoïra Tondikandia BONKOUKOU SHETT FANDOU ET GOUBEY Tillabéri TOUNFALIS Kourteye GARBEY MALO KOIRA DALWAY EGROU KOIRA TEGUI MARIDOUMBOU Ouallam LOKI DABRE CHICAL CHANYASSOU LOSSA KADO SARGANE KRIP BANIZOUMBOU SIGUIRADO Sinder TILLAKAINA KOIRA ZENO Filingué Kokorou HASSOU KABIA GAOBANDA GUESSE KOSSEY Gothèye GARIE Tillabéri SANSANE HAOUSSA BAGDAD DINGAZI BANDA GARDAMA KOIRA GOUTOUMBOU GOUROUKE Kourfeye Centre DAIBERI LOUMA DIEP BERI SIMIRI BANIZOUMBOU KANDA TIBEWA (DODO KOIRA) Téra GOUNOU BANGOU ZONGO AGGOU GANDOU BERI JIDAKAMAT MORIBANE KORIA HAOUSSA TONDIGAMEYE ITCHIGUINE Karma KONE BERI ZAGAGADAN Téra TASSI DEYBANDA KORIA GOURMA BANNE BERI Imanan TOMBO KOKOMANI HAOUSSA Hamdallaye Simiri Balleyara BONKOUKOU NAMARO NIAME Tondikandia SHETT FANDOU ET -

C:\Mes Documents\Annuaires\Annu
ANNUAIRE STATISTIQUE DU NIGER 2013 - 2017 REPUBLIQUE DU NIGER MINISTERE DU PLAN -©©©- INSTITUT NATIONAL DE LA STATISTIQUE Etablissement Public à Caractère Administratif ANNUAIRE STATISTIQUE 2013-2017 Edition 2018 Novembre 2018 1 Institut National de la Statistique ANNUAIRE STATISTIQUE DU NIGER 2013 - 2017 2 Institut National de la Statistique ANNUAIRE STATISTIQUE DU NIGER 2013 - 2017 ANNUAIRE STATISTIQUE 2013 - 2017 EDITION 2018 Novembre 2018 3 Institut National de la Statistique ANNUAIRE STATISTIQUE DU NIGER 2013 - 2017 4 Institut National de la Statistique ANNUAIRE STATISTIQUE DU NIGER 2013 - 2017 Ce document a été élaboré par : - Sani ALI, Chef de Division de la Coordination Statistique et de la Coopération Ont également participé à l’élaboration de cette publication, les structures et personnes suivantes de l’Institut National de la Statistique (INS) : Les structures : - Direction de la Comptabilité Nationale, de la Conjoncture et des Etudes Economiques (DCNCEE) ; - Direction des Statistiques et des Etudes Démographiques et Sociales (DSEDS). Les personnes : - Idrissa ALICHINA KOURGUENI, Directeur Général de l’Institut National de la Statistique ; - Issoufou SAIDOU, Directeur de la Coordination et du Management de l’Information Statistique. Ce document a été examiné et validé par les personnes ci-après : - Maman Laouali ADO, Conseiller du DG/INS ; - Djibo SAIDOU, Inspecteur des Services Statistiques (ISS) ; - Ghalio EKADE, Inspecteur de Services Statistiques (ISS) ; - Sani ALI, Chef de Division de la Coordination Statistique et de -
C:\Mes Documents\Annuaires\Annu
ANNUAIRE STATISTIQUE DU NIGER 2011 - 2015 REPUBLIQUE DU NIGER MINISTERE DU PLAN -©©©- INSTITUT NATIONAL DE LA STATISTIQUE Etablissement Public à Caractère Administratif ANNUAIRE STATISTIQUE 2011-2015 Edition 2016 Novembre 2016 1 ANNUAIRE STATISTIQUE DU NIGER 2011 - 2015 2 ANNUAIRE STATISTIQUE DU NIGER 2011 - 2015 ANNUAIRE STATISTIQUE 2011 - 2015 EDITION 2016 Novembre 2016 3 ANNUAIRE STATISTIQUE DU NIGER 2011 - 2015 4 ANNUAIRE STATISTIQUE DU NIGER 2011 - 2015 Ce document a été élaboré par : - Sani ALI, Chef de Service de la Coordination Statistique Ont également participé à l’élaboration de cette publication, les structures et personnes suivantes de l’Institut National de la Statistique (INS) : les structures : - Direction de la Comptabilité Nationale, de la Conjoncture et des Etudes Economiques (DCNCEE) ; - Direction des Statistiques et des Etudes Démographiques et Sociales (DSEDS). les personnes : - Idrissa ALICHINA KOURGUENI, Directeur Général de l’Institut National de la Statistique ; - Moussa MAMAN HASSAN, Directeur de la Coordination et du Management de l’Information Statistique ; - Issoufou SAIDOU, Chef de Division de la Coordination Statistique et de la Coopération. Ce document a été examiné et validé par les personnes ci-après : - Djibo SAIDOU, Inspecteur des Services Statistiques (ISS) ; - Ghalio EKADE, Inspecteur de Services Statistiques (ISS) ; - Ousseini HAMIDOU, Inspecteur de Services Statistiques (ISS) ; - Mahamadou CHEKARAO, Directeur / DCNCEE ; - Gapto MAI MOUSSA, Chef de Division des Statistiques Sociales (DSS) - Amadou MOSSI DIORI, Chef de Division de la Conjoncture ; - Tassiou ALMADJIR, Chef de Division des Comptes Nationaux. La reproduction de ce document a été assurée par le Service de Reprographie de l’INS : - Mme Mossi ODILE ECLOU, Chef de Service ; - Abdoul Aziz HAMANI ; - Mohamed MOUSSA ; - Alhassane TAHIROU.