A Conceptually New Treatment Approach for Relapsed
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Self-Inhibitory Nature of Metabolic Networks and Its Alleviation Through Compartmentalization
ARTICLE Received 30 Oct 2016 | Accepted 23 May 2017 | Published 10 Jul 2017 DOI: 10.1038/ncomms16018 OPEN The self-inhibitory nature of metabolic networks and its alleviation through compartmentalization Mohammad Tauqeer Alam1,2, Viridiana Olin-Sandoval1,3, Anna Stincone1,w, Markus A. Keller1,4, Aleksej Zelezniak1,5,6, Ben F. Luisi1 & Markus Ralser1,5 Metabolites can inhibit the enzymes that generate them. To explore the general nature of metabolic self-inhibition, we surveyed enzymological data accrued from a century of experimentation and generated a genome-scale enzyme-inhibition network. Enzyme inhibition is often driven by essential metabolites, affects the majority of biochemical processes, and is executed by a structured network whose topological organization is reflecting chemical similarities that exist between metabolites. Most inhibitory interactions are competitive, emerge in the close neighbourhood of the inhibited enzymes, and result from structural similarities between substrate and inhibitors. Structural constraints also explain one-third of allosteric inhibitors, a finding rationalized by crystallographic analysis of allosterically inhibited L-lactate dehydrogenase. Our findings suggest that the primary cause of metabolic enzyme inhibition is not the evolution of regulatory metabolite–enzyme interactions, but a finite structural diversity prevalent within the metabolome. In eukaryotes, compartmentalization minimizes inevitable enzyme inhibition and alleviates constraints that self-inhibition places on metabolism. 1 Department of Biochemistry and Cambridge Systems Biology Centre, University of Cambridge, 80 Tennis Court Road, Cambridge CB2 1GA, UK. 2 Division of Biomedical Sciences, Warwick Medical School, University of Warwick, Gibbet Hill Road, Coventry CV4 7AL, UK. 3 Department of Food Science and Technology, Instituto Nacional de Ciencias Me´dicas y Nutricio´n Salvador Zubira´n, Vasco de Quiroga 15, Tlalpan, 14080 Mexico City, Mexico. -

Plant Protease Inhibitors: a Defense Strategy in Plants
Biotechnology and Molecular Biology Review Vol. 2 (3), pp. 068-085, August 2007 Available online at http://www.academicjournals.org/BMBR ISSN 1538-2273 © 2007 Academic Journals Standard Review Plant protease inhibitors: a defense strategy in plants Huma Habib and Khalid Majid Fazili* Department of Biotechnology, The University of Kashmir, P/O Naseembagh, Hazratbal, Srinagar -190006, Jammu and Kashmir, India. Accepted 7 July, 2007 Proteases, though essentially indispensable to the maintenance and survival of their host organisms, can be potentially damaging when overexpressed or present in higher concentrations, and their activities need to be correctly regulated. An important means of regulation involves modulation of their activities through interaction with substances, mostly proteins, called protease inhibitors. Some insects and many of the phytopathogenic microorganisms secrete extracellular enzymes and, in particular, enzymes causing proteolytic digestion of proteins, which play important roles in pathogenesis. Plants, however, have also developed mechanisms to fight these pathogenic organisms. One important line of defense that plants have to fight these pathogens is through various inhibitors that act against these proteolytic enzymes. These inhibitors are thus active in endogenous as well as exogenous defense systems. Protease inhibitors active against different mechanistic classes of proteases have been classified into different families on the basis of significant sequence similarities and structural relationships. Specific protease inhibitors are currently being overexpressed in certain transgenic plants to protect them against invaders. The current knowledge about plant protease inhibitors, their structure and their role in plant defense is briefly reviewed. Key words: Proteases, enzymes, protease inhibitors, serpins, cystatins, pathogens, defense. Table of content 1. -

Effect of Statins and ACE Inhibitors Alone and in Combination on Clinical Outcome in Patients with Coronary Heart Disease
Journal of Human Hypertension (2004) 18, 781–788 & 2004 Nature Publishing Group All rights reserved 0950-9240/04 $30.00 www.nature.com/jhh ORIGINAL ARTICLE Effect of statins and ACE inhibitors alone and in combination on clinical outcome in patients with coronary heart disease VG Athyros1, DP Mikhailidis3, AA Papageorgiou2, VI Bouloukos1, AN Pehlivanidis1, AN Symeonidis4 and M Elisaf5, for the GREACE Study Collaborative Group 1Atherosclerosis Unit, Aristotelian University, Hippocration Hospital, Thessaloniki, Greece; 2Department of Clinical Biochemistry, Royal Free Hospital, Royal Free and University College Medical School, Pond Street, London, UK; 32nd Propedeutic Department of Internal Medicine, Aristotelian University, Hippocration Hospital, Thessaloniki, Greece; 4Greek Society of General Practitioners, Thessaloniki, Greece; 5Department of Internal Medicine, Medical School, University of Ioannina, Greece We assessed the ‘synergy’ of statins and angiotensin- point in group A was 31%, (95% CI À48 to À6%, P ¼ 0.01) converting enzyme inhibitors (ACEI) in reducing vascu- in comparison to group B, 59% (95% CI À72 to À48%, lar events in patients with coronary heart disease (CHD). Po0.0001) to group C and 63% (95% CI À74 to À51%, The GREek Atorvastatin and CHD Evaluation (GREACE) Po0.0001) to group D. There was no significant Study, suggested that aggressive reduction of low difference in RRR between groups C and D (9%, CI density lipoprotein cholesterol to 2.59 mmol/l À27–10%, P ¼ 0.1). Other factors (eg the blood pressure) (o100 mg/dl) significantly reduces morbidity and mor- that can influence clinical outcome did not differ tality in CHD patients, in comparison to undertreated significantly between the four treatment groups. -

Kinase-Targeted Cancer Therapies: Progress, Challenges and Future Directions Khushwant S
Bhullar et al. Molecular Cancer (2018) 17:48 https://doi.org/10.1186/s12943-018-0804-2 REVIEW Open Access Kinase-targeted cancer therapies: progress, challenges and future directions Khushwant S. Bhullar1, Naiara Orrego Lagarón2, Eileen M. McGowan3, Indu Parmar4, Amitabh Jha5, Basil P. Hubbard1 and H. P. Vasantha Rupasinghe6,7* Abstract The human genome encodes 538 protein kinases that transfer a γ-phosphate group from ATP to serine, threonine, or tyrosine residues. Many of these kinases are associated with human cancer initiation and progression. The recent development of small-molecule kinase inhibitors for the treatment of diverse types of cancer has proven successful in clinical therapy. Significantly, protein kinases are the second most targeted group of drug targets, after the G-protein- coupled receptors. Since the development of the first protein kinase inhibitor, in the early 1980s, 37 kinase inhibitors have received FDA approval for treatment of malignancies such as breast and lung cancer. Furthermore, about 150 kinase-targeted drugs are in clinical phase trials, and many kinase-specific inhibitors are in the preclinical stage of drug development. Nevertheless, many factors confound the clinical efficacy of these molecules. Specific tumor genetics, tumor microenvironment, drug resistance, and pharmacogenomics determine how useful a compound will be in the treatment of a given cancer. This review provides an overview of kinase-targeted drug discovery and development in relation to oncology and highlights the challenges and future potential for kinase-targeted cancer therapies. Keywords: Kinases, Kinase inhibition, Small-molecule drugs, Cancer, Oncology Background Recent advances in our understanding of the fundamen- Kinases are enzymes that transfer a phosphate group to a tal molecular mechanisms underlying cancer cell signaling protein while phosphatases remove a phosphate group have elucidated a crucial role for kinases in the carcino- from protein. -

Identification of Novel Monoamine Oxidase B Inhibitors from Ligand Based Virtual Screening
Identification of novel monoamine oxidase B inhibitors from ligand based virtual screening A thesis submitted to Kent State University in partial Fulfillment of the requirements for the Degree of Master of Science By Mohammed Alaasam August, 2014 Thesis written by Mohammed Alaasam B.S., University of Baghdad, 2007 M.S., Kent State University, 2014 Approved by Werner Geldenhuys , Chair, Master’s Thesis Committee Richard Carroll , Member, Master’s Thesis Committee Prabodh Sadana , Member, Master’s Thesis Committee Eric Mintz , Director, School of Biomedical Sciences James Blank , Dean, College of Arts and Sciences ii Table of Contents List of figure ...................................................................................................................... vi List of tables ..................................................................................................................... xiii Acknowledgments............................................................................................................ xiv Chapter one: Introduction ............................................................................................... 1 1.1.Parkinson's disease ....................................................................................................... 1 1.2.Monoamine oxidase enzymes ....................................................................................... 7 1.3.Structures of MAO enzymes ....................................................................................... 12 1.4.Three dimentiona -

Evaluation of Squalestatine 1 As an Enzyme Inhibitor for Lowering Cholesterol
Evaluation of Squalestatine 1 as an Enzyme Inhibitor for Lowering Cholesterol By Samaneh Noor-Mohammadi Daniel-Frank Feze University Of Oklahoma College of Engineering School of Chemical, Biological and Materials Engineering Spring 2008 1 Table of Contents Abstract .......................................................................................................................................... 6 Introduction and Background ..................................................................................................... 7 Cholesterol ................................................................................................................................................ 7 Methods for Reducing Cholesterol Level .............................................................................................. 9 The Drug Model .......................................................................................................................... 11 Problem with Statin Drugs ...................................................................................................................... 11 Squalestatin 1 .......................................................................................................................................... 12 Drug Model ............................................................................................................................................. 14 Dosage .................................................................................................................................................... -
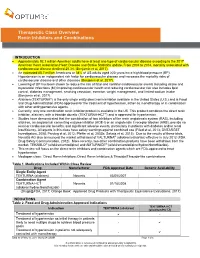
Therapeutic Class Overview Renin Inhibitors and Combinations
Therapeutic Class Overview Renin Inhibitors and Combinations INTRODUCTION Approximately 92.1 million American adults have at least one type of cardiovascular disease according to the 2017 American Heart Association Heart Disease and Stroke Statistics update. From 2004 to 2014, mortality associated with cardiovascular disease declined 25.3% (Benjamin et al, 2017). An estimated 85.7 million Americans or 34% of US adults aged ≥20 years have high blood pressure (BP). Hypertension is an independent risk factor for cardiovascular disease and increases the mortality risks of cardiovascular disease and other diseases (Benjamin et al, 2017). Lowering of BP has been shown to reduce the risk of fatal and nonfatal cardiovascular events including stroke and myocardial infarctions (MI) improving cardiovascular health and reducing cardiovascular risk also includes lipid control, diabetes management, smoking cessation, exercise, weight management, and limited sodium intake (Benjamin et al, 2017). Aliskiren (TEKTURNA®) is the only single entity direct renin inhibitor available in the United States (U.S.) and is Food and Drug Administration (FDA)-approved for the treatment of hypertension, either as monotherapy or in combination with other antihypertensive agents. Currently, only one combination renin inhibitor product is available in the US. This product combines the direct renin inhibitor, aliskiren, with a thiazide diuretic (TEKTURNA-HCT®) and is approved for hypertension. Studies have demonstrated that the combination of two inhibitors of the renin angiotensin system (RAS), including aliskiren, an angiotensin converting enzyme inhibitor (ACE-I) or an angiotensin II receptor blocker (ARB), provide no renal or cardiovascular benefits, and significant adverse events, particularly in patients with diabetes and/or renal insufficiency. -

Plant Serine Protease Inhibitors: Biotechnology Application in Agriculture and Molecular Farming
International Journal of Molecular Sciences Review Plant Serine Protease Inhibitors: Biotechnology Application in Agriculture and Molecular Farming Marina Clemente *, Mariana G. Corigliano, Sebastián A. Pariani, Edwin F. Sánchez-López, Valeria A. Sander and Víctor A. Ramos-Duarte Instituto Tecnológico Chascomús (INTECH), UNSAM-CONICET, Chascomús, Provincia de Buenos Aires B7130, Argentina; [email protected] (M.G.C.); [email protected] (S.A.P.); [email protected] (E.F.S.-L.); [email protected] (V.A.S.); [email protected] (V.A.R.-D.) * Correspondence: [email protected] Received: 12 January 2019; Accepted: 18 February 2019; Published: 17 March 2019 Abstract: The serine protease inhibitors (SPIs) are widely distributed in living organisms like bacteria, fungi, plants, and humans. The main function of SPIs as protease enzymes is to regulate the proteolytic activity. In plants, most of the studies of SPIs have been focused on their physiological role. The initial studies carried out in plants showed that SPIs participate in the regulation of endogenous proteolytic processes, as the regulation of proteases in seeds. Besides, it was observed that SPIs also participate in the regulation of cell death during plant development and senescence. On the other hand, plant SPIs have an important role in plant defense against pests and phytopathogenic microorganisms. In the last 20 years, several transgenic plants over-expressing SPIs have been produced and tested in order to achieve the increase of the resistance against pathogenic insects. Finally, in molecular farming, SPIs have been employed to minimize the proteolysis of recombinant proteins expressed in plants. The present review discusses the potential biotechnological applications of plant SPIs in the agriculture field. -

Disulfiram (Antabusr) in Bezug Auf Lyme-‐Borreliose. Private Notizen
Disulfiram (AntabusR) in Bezug auf Lyme-Borreliose. Private Notizen von J. Luché-Thayer, . 1 (Mail 15.3.2019). ohne Gewähr. Siehe auch: httPs://de.wikiPedia.org/wiki/Disulfiram Disulfiram (brand name Antabuse) not an antibiotic/ it is a generic drug. Has Antiparasitic (malaria/babesia) antiviral (HIV) & antibacterial aspects and has been around since the 1950s. 3 patients, who were previously very ill, have now been symptom free for 21 Months ------------------------------------------------------------------------------------- It is distributed by Teva in the US. By Ferring (a European company) in Mexico. The tablets are 250 mg. https://www.glowm.com/resources/glowm/cd/pages/drugs/d053.html ------------------------------------------------------------------------------------- Also, you can look up the basic info on Wikipekia: https://en.wikipedia.org/wiki/Disulfiram ²²²²²²²²²²²²²²²²²²²²²²²²²²²²²² Here is the elongated version of everything there is to know: https://pubchem.ncbi.nlm.nih.gov/compound/disulfiram#section=Solubility The more therapeutic information would be in the PDR, if you have one. ²²²²²²²²²²²²²²²²²²²²²²²²²²²²²²² (Dr. Kim Lewis, microbiologist and others.) They discovered Borrelia could not be killed with one round of antibiotics, even in the lab. Dr. Lewis had been researching persister bacteria, years before he started looking at Borrelia. 7KLVW\SHRIGUXJVWXG\VKRXOGKDYHEHHQFRQGXFWHGLQWKH¶VZKHQWKH<DOHUHVHDUFKHUV observed a progression of post-treatment symptoms occurring in some patients. Steere insisted the treatment was effective and the continuing or re-emergent symptoms were caused by an autoimmune response. This study revealed a failed round of antibiotic treatment increased the previous population of persister cells present. pre-treatment. Persister cells are less sensitive than non-persisters to the action of antibiotics. Additional antibiotic trials may increase the persister population, resulting in increased difficulty of treatment effectiveness of antibiotics in the future. -

Plant Protease Inhibitors in Control of Phytophagous Insects
EJB Electronic Journal of Biotechnology ISSN: 0717-3458 Vol.5 No.1, Issue of April 15, 2002 © 2002 by Universidad Católica de Valparaíso -- Chile Received August 20, 2001 / Accepted April 1, 2002 REVIEW ARTICLE Plant protease inhibitors in control of phytophagous insects Paulraj K. Lawrence* Department of Biological Sciences Texas Tech University Box No 43131 Lubbock, TX 79409-3131, USA Tel: 806 742 2740 Fax: 806 742 2963 E-mail: [email protected] Kripa Ram Koundal National Research Center on Plant Biotechnology Indian Agricultural Research Institute PUSA, New Delhi, India-110012, India Tel: 91 011 5711554 Fax: 91 011 5766420 E-mail: [email protected] Keywords: crop pests, protease inhibitors, transgenic plants. Plant proteinase inhibitors (PIs) have been well confounds the problem (Roush and McKenzie, 1987). established to play a potent defensive role against Under these circumstances, provision of food to the rapidly predators and pathogens. Although diverse endogenous expanding population has always been a challenge facing functions for these proteins has been proposed, ranging mankind. This problem is more acute in the tropics and sub- from regulators of endogenous proteinases to act as tropics, where the climate provides a highly condusive storage proteins, evidence for many of these roles is environment for a wide range of insects and necessitates partial, or confined to isolated examples. On the other massive efforts to suppress the population densities of hand, many PIs have been shown to act as defensive different pests in order to achieve an adequate supply of compounds against pests by direct assay or by food. In developing countries, the problem of competition expression in transgenic crop plants, and a body of from insect pests is further complicated with a rapid annual evidence for their role in plant defense has been increase in the human population (2.5-3.0 percentage) in accumulated consistently. -

Spring 2013 Lecture 16 & 17
CHM333 LECTURES 16 & 17: 2/22 – 25/13 SPRING 2013 Professor Christine Hrycyna ENZYME INHIBITION - INHIBITORS: • Interfere with the action of an enzyme • Decrease the rates of their catalysis • Inhibitors are a great focus of many drug companies – want to develop compounds to prevent/control certain diseases due to an enzymatic activity 1. e.g. AIDS and HIV protease inhibitors • HIV protease essential for processing of proteins in virus • Without these proteins, viable viruses cannot be released to cause further infection - Inhibitors can be REVERSIBLE or IRREVERSIBLE • Irreversible Inhibitors o Enzyme is COVALENTLY modified after interaction with inhibitor o Derivatized enzyme is NO longer a catalyst – loses enzymatic activity o Original activity cannot be regenerated o Also called SUICIDE INHIBITORS § e.g. nerve gas, VX gas § Aspirin! Acetylates Ser in active site of cyclooxygenase (COX) enzyme • Reversible Inhibitors o Bind to enzyme and are subsequently released o Leave enzyme in original condition o Three subclasses: § Competitive Inhibitors § Non-competitive Inhibitors § Uncompetitive Inhibitors o Can be distinguished by their kinetics of inhibition How are inhibitors characterized experimentally? • First, perform experiment without inhibitor o Measure velocity at different substrate concentrations, keeping [E] constant. Choose values of [S] o Get [S] and V values from experiment o Take reciprocal of [S] and V values (“1 over”) o Plot on graph 1/[S] (x) vs. 1/V (y) – don’t use Michaelis-Menten – not reliable • Second, do the SAME experiment in parallel using a fixed amount of inhibitor and same values for E and S • Get V values and plot together with uninhibited reaction • Depending on how the graph looks and using the subsequent equation of the line we can: o Determine type of inhibition (competitive vs. -

The Kinetics of Acetylcholinesterase Inhibition and the Influence of Fluoride and Fluoride Complexes on the Permeability of Erythrocyte Membranes
The Kinetics of Acetylcholinesterase Inhibition and the Influence of Fluoride and Fluoride Complexes on the Permeability of Erythrocyte Membranes Dissertation to receive Ph.D. in Chemistry from the University of Hamburg By Johannes Westendorf Hamburg, Germany – 1975 Reviewer: Prof. Dr. A. Knappwost Co-Reviewers: Prof. Dr. Malorny Prof. Dr. Strehlow Prof. Dr. Hilz Prof. Dr. Gercken The oral defense took place on 2/18/1975 Translation from German by: Jakob von Moltke Dartmouth College December 2000* *With proof corrections by MJ Coplan 1 Contents I. Introduction …………………………………………………………………………….. 3 II. Presentation of the Problem……………………………………………………………… 8 III. Procedure and Results………………………………………………………………….... 9 A. Inhibition of Acetylcholinesterases………………………………………………… 9 1. General Information………………………………………………………… 9 2. Theoretical Treatment of the Enzymatic Kinetics………….……………….10 3. Procedure……………………………………………………………………16 a. Description of the Tracer Method……………………..…………….16 b. Equipment….. ……………...…….…………………………………18 4. Carrying out the Measurements……………………………………………..19 a. Acetylcholinesterase Inhibition by NaF……………………………..20 b. pH Dependence of the Inhibition………………...………………….26 c. Dissociation Behavior of Several Fluoride Complexes ……………. 30 d. Inhibition of Acetylcholinesterase by Complexed Fluorides ..…….. 37 B. Effect of Fluoride on the Permeability of Erythrocyte Membranes for Na+, K+, 2+ - 2- Ca , F , HPO4 , and Glucose…………………………………………………. 49 1. Description of the Isotopes Used…………………………………………… 49 2. Presentation of the Permeability Experiments………………………………